Translate this page into:
Pain relief can be painful
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Mandibular nerve block is periodically used procedure used to treat neuralgic pain in the distribution of trigeminal nerve. It is a commonly performed block in outpatient settings at our institute. We present a case of an elderly edentulous patient with trigeminal neuralgia who suffered recurrent temporomandibular joint (TMJ) dislocation following mandibular nerve block. The patient presented with complaints of severe pain, inability to close mouth, and eat food since 2 days. Anterior closed reduction of TMJ resulted in reduction of joint and immediate pain relief. However, the maneuver failed due to recurrent dislocation of the joint. A Barton dressing was applied to prevent another dislocation. This was followed by autologous blood injection into the joint. This case focuses on the preponderance of clinical evaluation and accentuates the need for additional forethought to be taken during pain procedures, particularly in the geriatric population.
Keywords
Complication
Management
Mandibular nerve block complication
Neuralgia
Painful temporomandibular joint dislocation
INTRODUCTION
Blockade or destruction of portions of trigeminal nerve distal to the Gasserian ganglion is a well-demonstrated procedure to manage neuralgic pain in the distribution of the nerve.[12] Mandibular nerve block with alcohol is a frequently implemented procedure customarily in an outpatient context with minimal monitoring to treat trigeminal neuralgia with predominant pain in mandibular region.[3] This procedure is periodically used and is generally considered a safe procedure resulting in desiderata pain control. The reported complications of mandibular nerve block are less than 1% and those described in the literature are intravascular injection, hypoesthesia, dysesthesia, sensory and motor loss in the mandibular nerve distribution, prolonged vertigo, facial swelling, diplopia, etc.[456]
Here, we present a case of an elderly edentulous patient with trigeminal neuralgia who suffered recurrent temporomandibular joint (TMJ) dislocation following mandibular nerve block. While difficulty in chewing due to masseter muscle weakness is a common complaint in these patients, but TMJ dislocation is hardly seen. This case focuses on the preponderance of clinical evaluation and accentuates need for additional forethought to be taken during pain procedures, particularly in geriatric population.
CASE REPORT
An 85-year-old male patient, a known case of trigeminal neuralgia, presented to ourpain clinic with complaints of sharp, lancinating pain in left jaw and face, agnate to the distribution of left mandibular division of trigeminal nerve since last 10 years. There was no history of facial injury, dental manipulations, or intraoral infection. Physical and neurological examination was unremarkable. The TMJ movement were normal. The previous magnetic resonance imaging of the patient was normal and there was no evidence neural compression by vascular loop. In contempt of regular medical therapy with carbamazepine 200 mg thrice a day, there was little pain relief for last 2 months. His symptoms hadexacerbated in last few days and the pain became obstinate to treatment and patient was reluctant to increase the dose of drugs as it resulted in excessive sedation. Hence, he was prepared for mandibularnerve block on outpatient basis. He had no comorbidities and no positive medical history. Patient's vitals were stable and his physical examination was unremarkable. Written informed consent was received and the patient was taken up in the procedure room and standard monitors attached. After preparing the left side of the face with povidone iodine, sterile rapes were placed. Extraoral approach for mandibular nerve block was used. The patient was placed in a supine position with head tilted to the left side. After aseptic preparation and draping of the part, a 9.0 cm 22 gauge (G) needle was introduced perpendicularly in the middle of the coronal process at midpoint of the inferior border of the right zygomatic arch. The needle was advanced to hit the lateral pterygoid plate. The needle was withdrawn slightly and directed posteriorly toward the ear so that it passed the posterior border of the pterygoid plate. The needle was then carefully advanced 0.5 cm each time till the nerve stimulation was obtained. The mandibular nerve was stimulated at 1 mA for 0.1s stimulus duration with the help of a nerve stimulator, following which 2 ml of 2% lignocaine was injected after ensuring negative aspiration, which was followed by 1.0 ml absolute alcohol injection (1-Butanol, USP; Merck Specialties, Mumbai, India).[3] The procedure was uneventful and patient had immediate pain relief on the left side, but started complaining of mild pain on the right side of the face in preauricular region. In the absence of apparent physical findings we assumed it to be nonspecific and patient was sent home.
Two days post block, the patient presented with complaints of severe pain, inability to close mouth, and eat food since 2 days. On physical examination, right mandibular condyle was palpated anterior to the articular eminence. TMJ dislocation was obvious from history and physical examination. Maxillofacial surgeons were consulted who did anterior closed reduction of TMJ. The patient was positioned horizontal with the doctor standing behind the head of the patient. The thumbs were placed upon the ridge of the edentulous mandible intraorally, with the fingers swaddled externally around the mandible. Firm, passive and unwavering pressure was applied in a downward and posterior direction until the jaw came back into place. After few minutes the joint dislocated again. Two more closed reductions were attempted, but all in vain. A Barton's bandage was then applied to prevent another dislocation and the patient was cautioned to avoid opening the mouth wide. He was asked to come up for a follow-up in the maxillofacial outpatient department (OPD). Radiographic investigations were done, which showed deepened glenoid fossa and steep articular eminence [Figure 1]. The patient and his family were not amenable for the surgical treatment for dislocation, so it was decided to treat the recurrent dislocation by autologous blood injection.[7] Local anesthesia (2% lignocaine) was injected into the preauricular site, and a 21 gauge needle was inserted into the superior articular cavity of right side TMJ. Five milliliter blood was collected from a peripheral vein. Of this, 3 ml was injected into the superior articular activity and 1 ml was injected around the articular capsule. The mandible was then fixed with a bandage. Further, subluxation reoccurred over the next several days, but then desists after some days. Use of bandage was continued for 1 month as a precaution. Patient was pain free and able to carry out his normal daily activities like chewing, yawning, and mouth opening with reasonable ease 6 months post procedure [Figure 2]. Treatment done did not seem to affect his daily life, so it was decided not to perform further treatment.
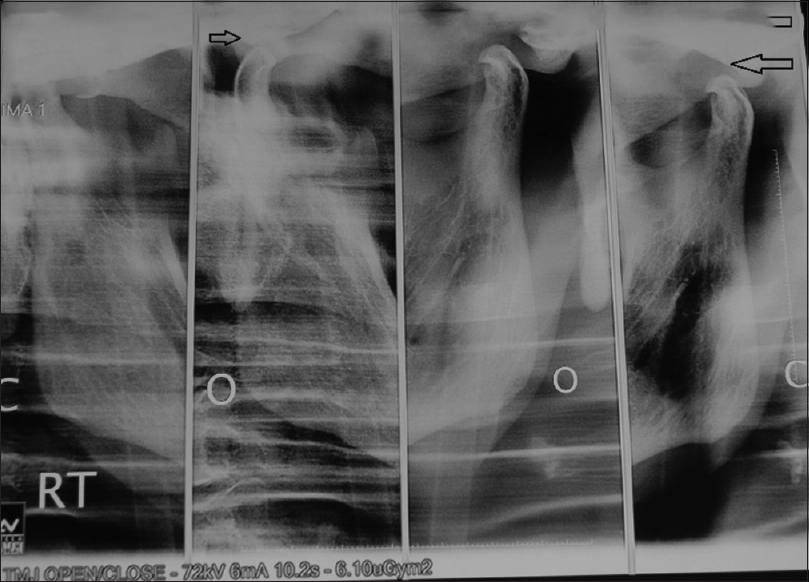
- Temporomandibular joint open and closed view showing deepened glenoid fossa and steep articular eminence.

- Six months postoperative photograph of the patient.
DISCUSSION
Neurolytic alcohol blocks are commonly used in patients with trigeminal neuralgia pertaining to mandibular distribution of the nerve. Usually done as an outpatient procedure with minimal complications and good pain relief for considerable time. However, these blocks offer limited pain relief and repeated blocks are less successful and associated with higher risk of neuritis.[3] This case reports occurrence of rare but disabling complication which happened not because of the neural blockade, but as a consequence of pain relief.
Usual complications of mandibular nerve block are hypoesthesia, dysesthesia, sensory loss in mandibular nerve distribution, facial swelling, and masseter muscle weakness,[8] but dislocation of the joint following mandibular nerve block for inferior alveolar nerve neuralgia is never reported in the literature. Dislocation of the TMJ represent 3% of all reported dislocated joints in the body.[9] TMJ dislocation is a painful condition occurring due to fixation of mandibular condyle in the anterosuperior aspect of the articular eminence. We assume that in this case, patient restrained his mouth opening while laughing, yawning, or biting due to severe neuralgic pain. But once there was pain relief following mandibular nerve block, the mobility across TMJ was regained and due to previous excessive looseness/laxity of the mandibular and capsular ligaments, dislocation occurred. This laxity of ligaments attributed to hypermobility of the mandible along with the presence of steep articular eminence in old age precipitating dislocation. Additionally, patients with weakness of the joint capsule, anatomic aberration of the joint, or injury to the associated ligaments are at greater risk of dislocation.[10] Role of muscles and their tone for control of TMJ movements and possibility of loss of tone adding to recurrent dislocations cannot be ruled out.
Autologous blood is a lucid and minimally invasive method for the treatment for recurrent TMJ dislocation. The paramount desideratum of autologous blood injection is to limit mandibular movement. The contingent mechanism of action is that blood injected would result in formation of local bed for fibrous tissue, that will eventually lead to the embodiment of adhesions in the cavity.[11] This is a unique case report of occurrence of rare complication like temporomandibular dislocation following peripheral trigeminal nerve block procedure.
The intent of reporting this case is to raise the alertness of probableserious complication like TMJ dislocation, especially in edentulous geriatric patients following pain relief due to peripheral mandibular nerve blocks which are customarily contemplated as minor outpatient procedures.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Trigeminal neuralgia: Assessment and management by oral and maxillofacial surgeons in the United Kingdom. Br J Oral Maxillofac Surg. 2009;47:42-5.
- [Google Scholar]
- Practice parameter: The diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology. 2008;71:1183-90.
- [Google Scholar]
- Brief report: The long-term outcome of mandibular nerve block with alcohol for the treatment of trigeminal neuralgia. Anesth Analg. 2010;111:550-3.
- [Google Scholar]
- Prolonged vertigo and ataxia after mandibular nerve block for treatment of trigeminal neuralgia. J Anaesthesiol Clin Pharmacol. 2011;27:386-8.
- [Google Scholar]
- Diplopia after inferior alveolar nerve block anesthesia: Report of 2 cases and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e21-4.
- [Google Scholar]
- Autologous blood injection into the articular cavity for the treatment of recurrent temporomandibular joint dislocation: A case report. J Oral Sci. 2007;49:237-9.
- [Google Scholar]
- Complications of alcohol injection into the mandibular nerve. Gasserian palsy and oculomotor palsy (author's transl) Reg Anaesth. 1982;5:39-41.
- [Google Scholar]
- Reduction eminoplasty for chronic recurrent luxation of the temporomandibular joint. J Can Dent Assoc. 1981;47:179-84.
- [Google Scholar]
- Dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:662-8.
- [Google Scholar]
- Autologous blood injection for treatment of recurrent temporomandibular joint dislocation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:390-3.
- [Google Scholar]






