Translate this page into:
Specialist Pediatric Palliative Care Prescribing Practices: A Large 5-year Retrospective Audit
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
There is a gradual increasing trend in childhood cancers in India and pediatric palliative care in India is an emerging specialty. Prescribing pain and symptom control drugs in children with cancer requires knowledge of palliative care formulary, dosing schedules, and prescription guidelines. This study is a retrospective audit of prescribing practices of a specialist palliative care service situated in a tertiary cancer center.
Methods:
A total of 1135 medication records of children receiving specialist pediatric palliative care services were audited for 5 years (2010–2014) to evaluate prescribing practices in children with advanced cancer.
Results:
A total of 51 types of drugs were prescribed with an average of 4.2 drugs per prescription. 66.9% of the prescriptions had paracetamol, and 33.9% of the prescriptions had morphine. Most common nonsteroidal anti-inflammatory drugs prescribed was ibuprofen (23.9%), and more than 50% of the prescriptions had aperients. The most commonly prescribed aperient was a combination of liquid paraffin and sodium-picosulfate. Dexamethasone was prescribed in 51.9% of patients and in most cases this was part of oral chemotherapy regimen. Generic names in prescription were used only in 33% of cases, and adverse effects of the drugs were documented in only 9% of cases. In 25% of cases, noncompliance to the WHO prescription guidelines was seen, and patient compliance to prescription was seen in 40% of cases.
Conclusions:
Audit of the prescribing practices in specialist pediatric palliative care service shows that knowledge of pediatric palliative care formulary, rational drug use, dosing, and prescribing guidelines is essential for symptom control in children with advanced life-limiting illness. Noncompliance to WHO prescribing guidelines in one fourth of cases and using nongeneric names in two-thirds of prescription indicates poor prescribing practices and warrants prescriber education. Prescription noncompliance by almost two-thirds of patients is alarming and necessitates intense patient, family, and caregiver education and empowerment.
Keywords
Audit
Prescribing practices
Specialist pediatric palliative care
INTRODUCTION
Pediatric palliative care as defined by WHO comprises of active total care of child's body, mind, and spirit and also involves providing support to the family. It begins with diagnosis of illness and continues regardless of whether or not a child receives disease-directed treatment.[1] The life-limiting conditions that are encountered in pediatric palliative care practice are genetic/congenital (40.8%), neuromuscular (39.2%), cancer (19.8%), chronic respiratory (12.8%), and gastrointestinal (GI) (10.7%) conditions.[2] The proportion of childhood cancers in India as compared to overall cancers is between 0.8% to 5.8% in boys, and between 0.5% to 3.4% in girls.[3] 80% children in the world live in low- and middle-income countries. Each year 200,000 children are diagnosed with cancer and due to limited access to curative treatment, only about 25% survive.[4] Pediatric palliative care is being increasingly recognized as an essential health care need over past decade and is integrated into the mainstream care of children with life-limiting illnesses.[5] The evidenced-based practice of palliative medicine involves integrating the best available evidence from clinical research into the day-to-day practice of palliative medicine. There is a lack of quality research in pediatric palliative care due to lesser number of studies conducted in pediatric palliative care and ethical issues involved in conducting these studies.[6] There is dearth of literature about the symptom burden in childhood cancer patients presenting to palliative medicine department and prescribing patterns of symptom control drugs. The rational use of drugs requires that “patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period, at the lowest cost to them and their community.”[7] Moreover, the treatment of diseases by the use of essential drugs, prescribed by their generic names, has been emphasized by WHO and National Health Policy of India.[8] Irrational prescribing is a problem as it leads to ineffective and unsafe treatment of symptoms, exacerbation or prolongation of illness or complications, distress and harm to the patient, and financial burden to the family.
Various factors influence prescribing behavior of clinicians and to modify these behaviors it is necessary to understand the factors that underpin these prescribing behaviors.[910] Various factors responsible for irrational prescribing patterns may be due to poor symptom reporting, peer prescribing practices, and high-powered salesmanship by drug company representatives. In teaching hospitals, junior doctors emulate the prescribing practices of senior clinicians. It is important to know the existing prescription patterns to monitor, assess, evaluate and suggest appropriate modifications to the current drug prescribing practices.[11] In addition, the assessment of drug compliance in patients is important for clinical, educational, and economic reasons.[12] Data about drug usage patterns in India are particularly lacking.[8]
WHO recommends that it is important to pay attention to the frequency and severity of the adverse drug reactions, identify the spectrum of disease and comorbidities, country-specific medicine handling circumstances, drug interactions with the traditional medicines, differences in genetic compositions of the populations in developed and developing countries and pharmaceutical quality of the locally manufactured medicines. Hence, it is important to have country-specific data about the prescribing patterns of drugs in children and their adverse reactions as the data generated elsewhere may not be relevant.[13]
This audit aims to evaluate the drug prescribing practices in specialist pediatric palliative care unit of a tertiary referral cancer and assesses their adherence to WHO recommendations for drug prescribing in children.
METHODS
Study method and population
This is a retrospective audit of the prescribing patterns of all patients referred to specialist pediatric palliative care unit over a period of 5 years from January 1, 2010, to December 31, 2014. Data was obtained from the review of medical charts of the patients enrolled with specialist pediatric palliative care services.
All children ≤18 years of age enrolled with specialist pediatric palliative care services of the Department of Palliative Medicine at the Tata Memorial Centre (Mumbai) from January 1, 2010, to December 31, 2014, were included in the study. The Tata Memorial Centre, Institutional Review Board (IRB) ethics approval was obtained. As this study was a retrospective audit, IRB permitted waiver of consent.
Data collection and outcome measures
Audit
Data required to know the prescribing practices of specialist pediatric palliative care unit was recorded for each patient encounter and data was manually entered into the study case record form. The following variables were recorded:
-
Sociodemographic information (age, gender, primary caregiver, monthly family income, educational status of patient and primary caregiver)
-
Clinical information recorded were Eastern Cooperative Oncology Group (ECOG) score, diagnosis, stage of disease, sites of metastasis, treatment received, date of last treatment, ongoing medications at the time of initial referral, drug allergies, symptoms at the time of initial referral, symptom control medications prescribed, use of generic names in prescription, route of administration, and deviation from the standards recommended by the WHO[1314]
-
Body weight
-
Follow-up visit information recorded were date of follow-up, ECOG score, weight, treatment compliance, recording of symptoms, adverse effects of drugs, changes made to prescription during follow-up, deviation from standards recommended by the WHO.
The outcome measures were:
-
Sociodemographic and clinical characteristics of patients who received services from specialist pediatric palliative care unit
-
Performance status at each consultation was measured using ECOG Score. It is a standard tool used to assess the performance status of the patient.[15] It is used to assess the impact of the disease on activities of daily living, performance, ability to self-care, which in turn could help to determine the prognosis and plan appropriate treatment for the patient. It is an open assess tool and hence no permission was required for its use
-
Symptoms and its severity at presentation and follow-up visits to pediatric palliative care unit were measured using Edmonton Symptom Assessment System (ESAS).[16] Symptom burden at baseline and change in symptom burden was recorded using ESAS, which is a valid multidimensional symptom assessment tool, comprising of commonly encountered symptoms, and their severity is recorded on a scale of 0-10. It is used as a part of routine assessment in palliative medicine unit
-
Symptom control medications during initial referral, and any known drug allergy
-
Number of drugs prescribed, generic names used, and route of medications
-
Adverse effects of drugs during follow-up visit
-
Comparison of the prescribing practices with standard WHO guidelines for prescribing practices by WHO. The WHO has recommended the following core indicators for prescribing in pediatric population, namely, an average number of drugs prescribed, percentage of drugs prescribed by generic name, percentage of antibiotics prescribed, percentage of injections prescribed, percentage of drugs prescribed from the essential drug list. These indicators and the adherence to the drugs and dosage guidelines were studied.[1314]
Statistical analysis
Data necessary to measure the drug prescribing practices was recorded for each patient encounter and entered directly into the case record form. Using the final compiled master database, descriptive statistics (proportions, means and standard deviation, medians, as appropriate) was used to describe patient characteristics, symptoms, and details of drug prescribing practices. Equivalency of proportions in contingency tables was tested using the Wilcoxon Signed Ranks Test for ESAS scores with baseline and follow-up to determine if there is any significant improvement. P < 0.05 was taken as significant. Statistical analyses were performed using SPSS 20 (IBM SPSS Statistics for Windows, version 20.0, IBM Corp., Armonk, NY, USA).
RESULTS
Patient characteristics
A total of 1135 children with advanced cancer were enrolled in the pediatric palliative care service from January 1, 2010, to December 31, 2014. There was a steady rise in the referrals to the specialist pediatric palliative care during the audit period [Figure 1].
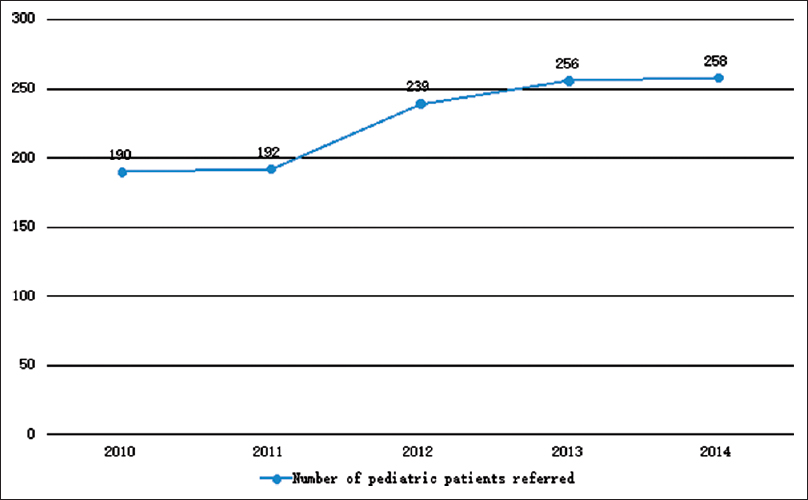
- Number of pediatric patients referred
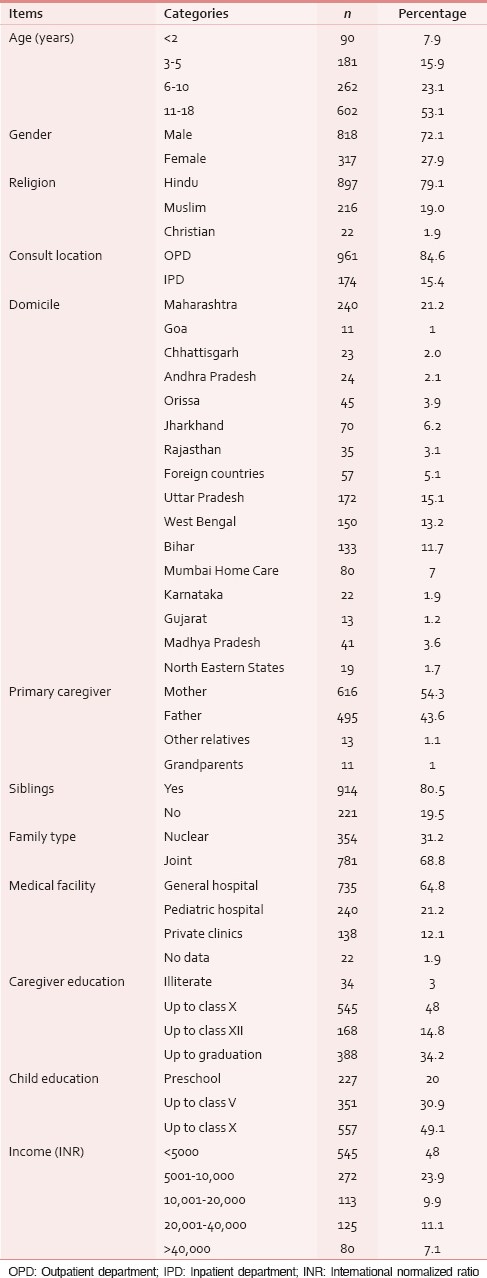
Among the total number of patients referred 818 (72.1%) were male. 602 (53.1%) patients were above 10 years. 961 (84.6%) consultations took place in outpatient setting. In 1111 (97.9%) cases, parents were the primary caregivers. 914 (80.5%) children had siblings and had extended families in 781 (68.8%) of the cases. 545 (48%) caregivers had completed high school education. 545 (48%) of the families had serious economic constraints and earned <5000 INR (approximately 73 USD) per month. 240 (21.2%) patients had access to specialist pediatric health care services at their local place. 1055 (93%) patients were from places outside Mumbai. Only 56 (4.9%) completed more than 2 follow-ups [Table 1].
Clinical data
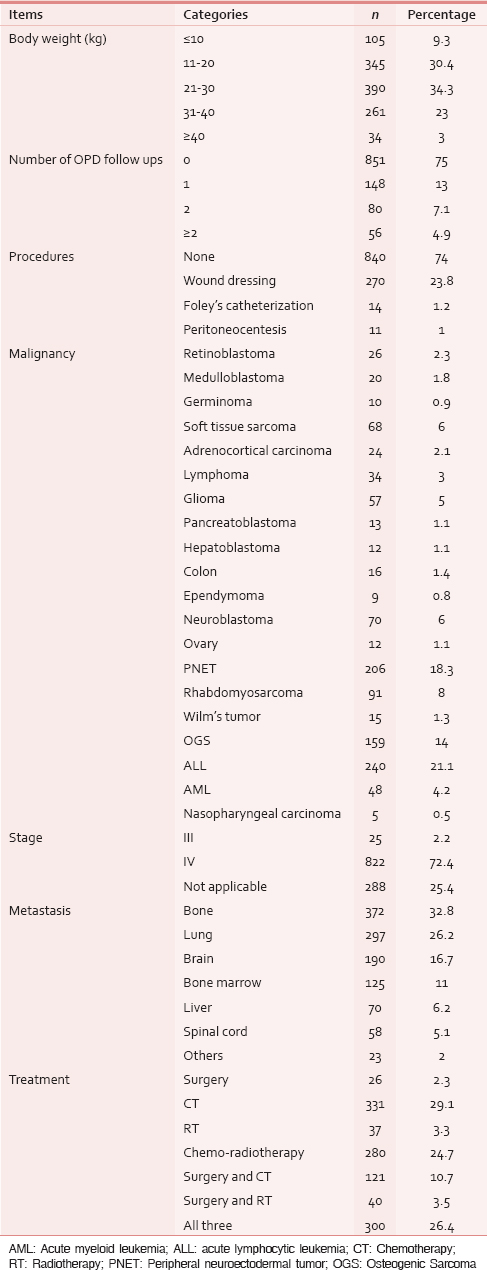
322 (28.3%) referrals were from pediatric hematology-oncology unit. 822 (72.4%) children had relapse or progressive disease and were not amenable for further disease modifying treatment at time of referral. 331 (29.1%) received oral chemotherapy as major treatment modality. 372 (32.8%) patients had skeletal metastasis [Table 2].
Eastern cooperative oncology group and edmonton symptom assessment system scores at referral
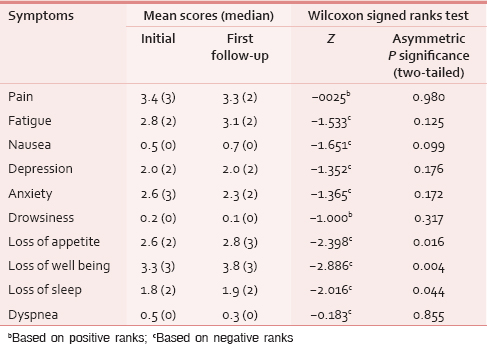
A total of 447 (39%) patients had performance score of 2 on ECOG scale. Symptoms were screened using ESAS scale during the first visit. Wong-Baker Faces Pain Rating Scale was used for children under 8 years. Severe pain (median score 3) was present in 229 (20.2%) patients, followed by severe loss of well-being (median score 3) in 112 (9.8%), and severe fatigue (median score 2) in 86 (7.6%). Symptoms such as drowsiness, breathlessness, and nausea were less common. Since ESAS scoring system was used, depression and anxiety scores were not assessed in children <5 years of age. 491 (43.3%) had mild depression (median score 2), and 629 (55.4%) had mild anxiety (median score 3) on ESAS [Table 3].
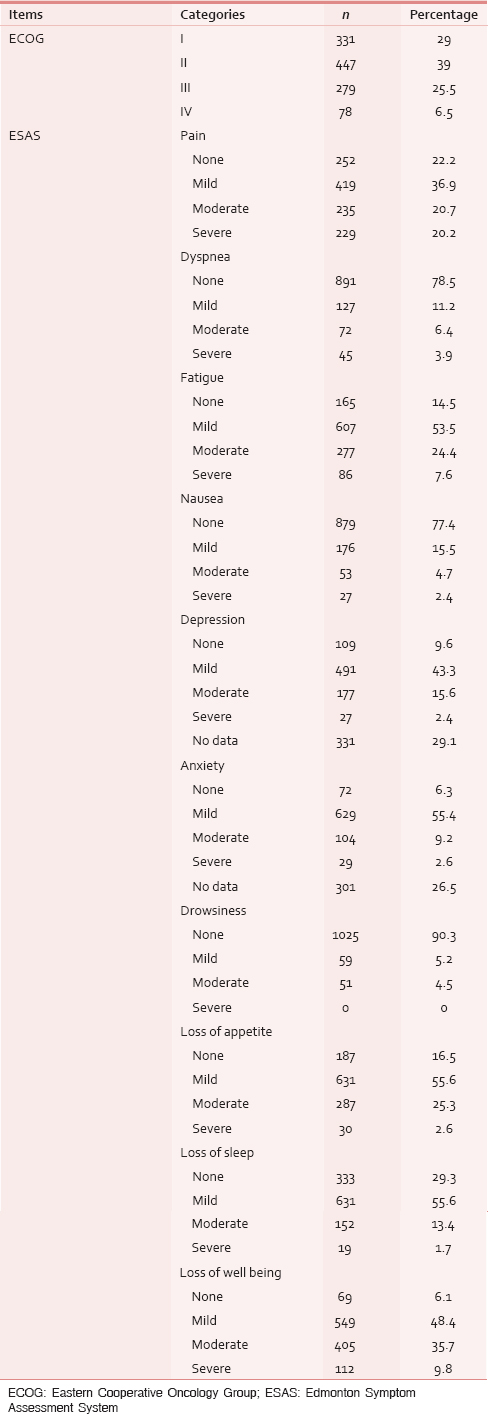
Change in symptom burden was recorded using ESAS at first follow-up. Statistically significant improvement was noted in loss of appetite (P = 0.016), loss of well-being (P = 0.004), and loss of sleep (P = 0.044) [Table 4].
Prescribing data
Palliative care formulary is used as a reference guide to inform the prescribing practices of the department.[17] Audit showed 51 types of drugs were prescribed by the specialist pediatric palliative care service. The service over a period of 5 years (2010–2014) prescribed 5920 drugs in 1491 prescriptions. Most commonly used opioid was morphine, found in 385 (33.9%) prescriptions. Although Codeine is not recommended in children, Codeine was prescribed in 147 (12.9%) prescriptions. Paracetamol was found in 760 (66.9%) prescriptions. Most common nonsteroidal anti-inflammatory drugs prescribed were ibuprofen found in 272 (23.9%) prescriptions. For neuropathic pain mostly common drug prescribed was amitriptyline found in 67 (5.9%) prescriptions. Among the drugs acting on GI system, pantoprazole was found in 397 (34.9%) prescriptions, and liquid paraffin-based laxative was found in 624 (54.9%) prescriptions. Among the antibiotics prescribed, amoxicillin was the most commonly prescribed antibiotic found in 45 (3.9%) prescriptions. Dexamethasone was found in 590 (51.9%) prescriptions. Multivitamins were found in 330 (29.1%) prescriptions [Table 5].
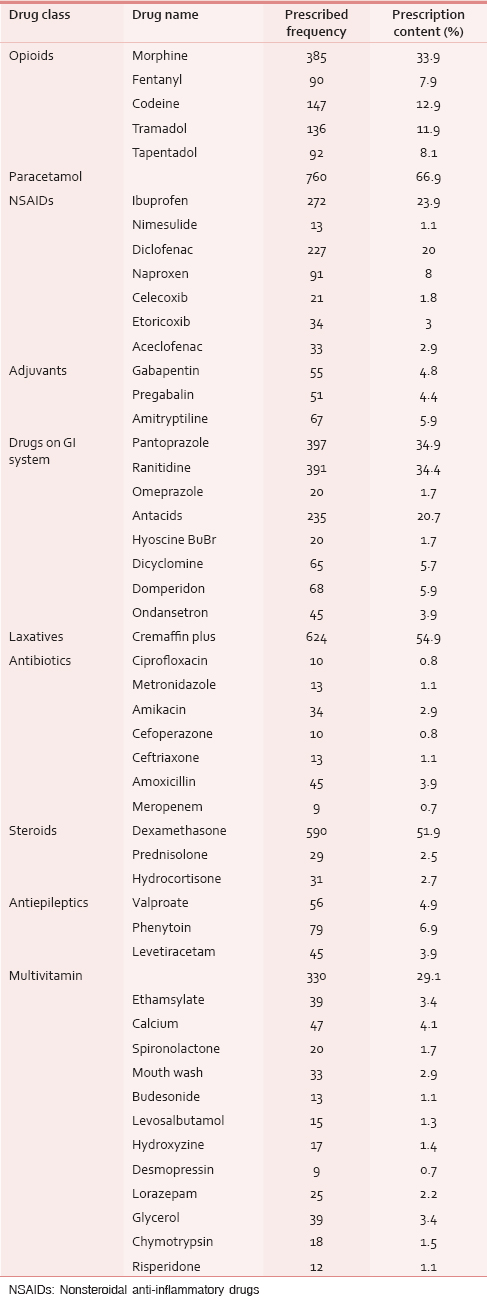
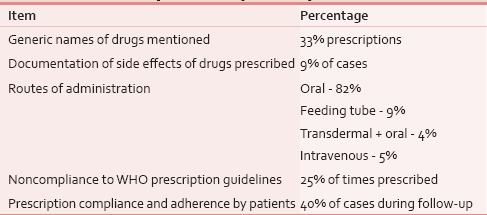
Average number of medications was 4.2 drugs per prescription. This was in addition to ongoing oral cancer medicines. Generic names of drugs were used in only 33% of the prescriptions. Adverse effects of symptom control drugs prescribed were only documented in 9% of cases. Oral route (82%) was the most preferred route of administration. Noncompliance to WHO prescription guidelines was seen in 25% of cases. During follow-up, it was found that prescription compliance and adherence was seen only in 40% of the cases [Table 6].
DISCUSSION
Specialist pediatric palliative care service was initiated in our institute in 2002. However, we could gather data of only last 5 years (2010-2014) as previous records were not available from the archives. This is the first study in India to evaluate specialist pediatric palliative care prescribing practices.
Our findings provide evidence that standard palliative care consultation for children with advanced cancer improves symptoms such as pain, loss of appetite, loss of well-being, and loss of sleep. Pain was the most common symptom in children. 850 (74.7%) were on either weak or strong opioids. Morphine was prescribed in 385 (33.9%) patients. These findings are supported by a study done by Curtis and Walsh on adults with advanced cancer where strong opioids were used for pain control.[18] The service strictly adheres to palliative care prescribing principles such as “by mouth,” “by the clock,” “by the ladder,” “for the individual,” and “attention to detail.”[19] Oral route was the most preferred route for medications. In patients where it was not possible to give orally, such as in intestinal obstruction and dysphagia, other routes of administration such as transdermal, subcutaneous, and intravenous routes were considered. Laxatives were given to 624 (54.9%) of children due to our routine practice of prescribing a laxative regimen along with the opioid analgesics. Along with opioids prescriptions, paracetamol was the most commonly used step I analgesic. This is in accordance to WHO analgesic ladder.[14]
Other than conventional symptom control drugs, dexamethasone was prescribed for more than 50% of patients. Dexamethasone has multiple mechanisms of action such as anti-inflammatory, appetite stimulation, anti-edema effect, antiemetic, and anti-neuropathic pain actions. Its role as an adjuvant analgesic reduces the need for multiple medications.[20] Many children seen in the clinic were undernourished and had features of vitamin deficiency warranting the use of use of multivitamins.[21]
Antibiotics were used in 134 (11.3%) children. The prescribing prevalence of antibiotics was low compared to other studies done in general pediatric patients.[22] Antimicrobial resistance is a common clinical problem in Indian pediatrics practice.[23] The widespread use of antimicrobials, whether appropriate or inappropriate, has driven the emergence and spread of resistant organism.[2425] Most of the children referred to palliative care had received broad-spectrum antibiotics prior for infective complications of chemotherapy. The most common infection in children is bacterial upper respiratory tract infection caused by Streptococcus pneumoniae, which is sensitive to penicillin group of antibiotics.[24] Amoxicillin was the most commonly prescribed antibiotic in our service. Ciprofloxacin was prescribed to only 0.8% of patients with upper respiratory tract infection. It is generally avoided due to its toxic effects in children which is similar to the reports from other studies.[26] Average number of drugs per prescription in our service was 4.2. This is comparable to WHO data.[27]
Little comparative information is available in the literature concerning palliative care prescribing practices in children. This is the first study that has examined a large data from a tertiary cancer care institute from India, which has examined the pediatric palliative care prescription patterns for children with advanced life-limiting illness. The data were sourced from both manual and electronic medical records to minimize errors and avoid missing data.
Limitations to the audit can be ascribed to its retrospective nature. Furthermore, in this study, only 33% of the prescriptions were by generic names of drugs which, according to WHO and National Health Policy of India is inappropriate. Formal cost analysis could not be done due to inadequate data on quantity of medicines issued. Future studies need to focus on formulating a set of criteria, which can facilitate creation of a robust prescribing system. This audit may provide some insights that can assist in creation of a pediatric palliative care pharmacopeia.
CONCLUSIONS
Audit of the prescribing practices in specialist pediatric palliative care service shows that knowledge of pediatric palliative care formulary, rational drug use, dosing, and prescribing guidelines is essential for symptom control in children with advanced life-limiting illness. Noncompliance to WHO prescribing guidelines in one-fourth of cases and using nongeneric names in two-thirds of prescription indicates poor prescribing practices and warrants prescriber education. Prescription noncompliance by almost two-thirds of patients is alarming and necessitates intense patient, family, and caregiver education and empowerment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Pediatric palliative care patients: A prospective multicenter cohort study. Pediatrics. 2011;127:1094-101.
- [Google Scholar]
- Childhood cancer incidence in India: A review of population-based cancer registries. Indian Pediatr. 2014;51:218-20.
- [Google Scholar]
- Global child health priorities: What role for paediatric oncologists? Eur J Cancer. 2008;44:2388-96.
- [Google Scholar]
- Recognizing a global need for high quality pediatric palliative care. Pediatr Blood Cancer. 2011;57:187-8.
- [Google Scholar]
- Reporting of pediatric palliative care: A systematic review and quantitative analysis of research publications in palliative care journals. Indian J Palliat Care. 2011;17:202-9.
- [Google Scholar]
- Assessment of drug use pattern using WHO prescribing indicators at Hawassa University Teaching and Referral Hospital, South Ethiopia: A cross-sectional study. BMC Health Serv Res. 2013;13:170.
- [Google Scholar]
- 2006. National Health Programs of India. (6th ed). New Delhi: Century Publications; :370. Available from: https://www.openlibrary.org/books/OL16254320M/National_health_programs_of_India
- Update-victorian medical postgraduate foundation group. Aust J Hosp Pharm. 1988;18:17-8.
- [Google Scholar]
- Medication errors: Prescribing faults and prescription errors. Br J Clin Pharmacol. 2009;67:624-8.
- [Google Scholar]
- Prescribing trends in internal medicine. Int J Clin Pharmacol Ther Toxicol. 1984;22:375-6.
- [Google Scholar]
- Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-55.
- [Google Scholar]
- Audit methods: The edmonton symptom assessment system. 1993. Clinical Audit in Palliative Care. Oxford, UK: Radcliffe Medical Press; :61-77. Available from: http://www.librarysearch.cf.ac.uk/primo_library/libweb/action/display.do?ct=display&fn=search&doc=CARDIFF_LMS694223&indx=1&recIds=CARDIFF_LMS694223&recIdxs=0&elementId=0&renderMode=poppedOut&displayMode=full&frbrVersion=&tabs=detailsTab&gathStatTab=true&fromBrowseShelf=true&dscnt=0&frbrVersion=&scp.scps=scope%3A%28CARDIFF_LMS%29%2Cscope%3A%28CARDIFF_DTL%29%2Cscope%3A%28DAWSON_PDA%29% 2Cscope%3A%28CARDIFF_EBA%29% 2Cscope%3A%28CARDIFF_DTL_DC%29&tab=librarycollections&dstmp=1420140835349&srt=rank&callNum
- [Google Scholar]
- Palliativedrugs.com. Essential Independent Drug Information for Palliative and Hospice Care. Available from: http://www.palliativedrugs.com/palliative-care-formulary.html
- [Google Scholar]
- Prescribing practices of a palliative care service. J Pain Symptom Manage. 1993;8:312-6.
- [Google Scholar]
- Scottish Palliative Care Guidelines. Available from: http://www.palliativecareguidelines.scot.nhs.uk/
- 19th WHO Model List of Essential Medicines (April 2015) 2015. WHO. Available from: http://www.who.int/medicines/publications/essentialmedicines/EML2015_8-May-15.pdf
- [Google Scholar]
- Prevalence of Vitamin D deficiency among Turkish, Moroccan, Indian and sub-Sahara African populations in Europe and their countries of origin: An overview. Osteoporos Int. 2011;22:1009-21.
- [Google Scholar]
- Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA. 1995;273:214-9.
- [Google Scholar]
- The problem of resistant bacteria for the management of acute otitis media. Pediatr Clin North Am. 1995;42:509-17.
- [Google Scholar]
- Antimicrobial resistance in hospital organisms and its relation to antibiotic use. Rev Infect Dis. 1983;5:1033-48.
- [Google Scholar]
- The spread of multiply resistant Streptococcus pneumoniae at a day care center in Ohio. J Infect Dis. 1992;166:1346-53.
- [Google Scholar]
- Drug utilization pattern in South Indian pediatric population: A prospective study. Perspect Clin Res. 2014;5:178-83.
- [Google Scholar]






