Translate this page into:
Role of Integrative Oncology and Palliative Care Services in Improving Comfort Level and Compliance among Patients with Advanced Fungating Breast Cancer – Experience from a Rural Hospital of North Eastern India during the COVID-19 Pandemic
*Corresponding author: Samrat Dutta, Associate professor, Department of Radiotherapy North Bengal Medical College, Siliguri, West Bengal, India. drsamratdutta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dutta S, Ishore K, Ghoshal A. Role of integrative oncology and palliative care services in improving comfort level and compliance among patients with advanced fungating breast cancer – Experience from a rural hospital of North Eastern India during the COVID-19 pandemic. Indian J Palliat Care 2022;28:256-61.
Abstract
Objectives:
Malignant fungating breast cancers are a definite challenge to treatment due to limited knowledge and prevailing distressing symptoms. Various treatment protocols with regard to radiotherapy (RT) and chemotherapy have been reported in the literature but the knowledge of proper integration of these regimes with effective palliative care nursing care, particularly in resource poor settings, is not well understood. Hence, this study was undertaken to assess the change in the degree of comfort achieved before and after treatment of these fungating breast cancer wounds along with issues regarding compliance to such treatment in a peripheral rural medical college hospital.
Materials and Methods:
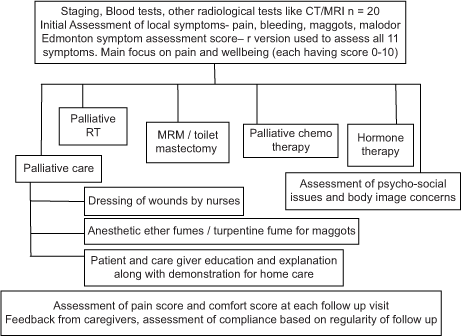
A total of 20 patients were selected from the medical records files of the RT department of North Bengal Medical College and Hospital who were registered and treated during the period 1 June 2019– 31 July 2021. Palliative care nursing of malodour, bleeding, maggots, pain and assessment of psychological parameters was done based on the 11-point revised Edmonton Symptom Assessment Scale at the beginning and at each subsequent follow-up visits. Patients were also individualised for receiving palliative RT, chemotherapy, surgery and hormone therapy based on their clinicodemographic profiles. Informed consent was taken from all patients and every treatment was in accordance with the ethical permissions as sought from the Institutional Ethics Committee. Statistical analysis was done based on descriptive statistics and SPSS version 22.
Results:
Median follow-up was 13 months. Overall, there was a significant improvement in comfort and well-being as assessed by paired t-test before and after treatment (paired t-test = 16.548; P = 0.000). However, there was no significant correlation with palliative radiation dose and schedule as per spearman’s correlation coefficient. The mean radiation dose was BED 48.56 Gy3 (EQD2 = 29.3 Gy3) and the median number of fractions used was 10. Almost 50% of patients were noncompliant to treatment and this might be attributed to the prevailing COVID-19 pandemic situation. There was maximum relief with regard to bleeding control (100%), malodour dissipation (76.9%) and control of maggots infestation (71%) and these results were also found to be strongly associated with treatment as per analysis done by Chi-square test of difference of proportions.
Conclusion:
Effective comfort can be achieved with proper judicious combination of palliative care nursing and other oncological treatment such as radiation, chemotherapy and surgery.
Keywords
Fungating
Breast
Palliative care
COVID-19
INTRODUCTION
Breast cancer is the most common diagnosed cancer in women and is the leading cause of cancer related deaths in both developed and developing countries across the globe. Under the network of Indian National Cancer Registry Program 2012–2016, 57.06% of the patients diagnosed with breast cancer had locally advanced cancer and approximately 5–10% of newly diagnosed patients with breast cancer are metastatic at diagnosis.[1] Nearly 2–5% of locally advanced breast cancers develop a fungating breast cancer.[2]
The problems of malignant advanced fungating breast cancer tumours are manifold and ultimately restrict the average life expectancy around 6 months–1 year.[3] The management of fungating breast cancers is complex and often poorly understood. However, there are limited resources to guide optimisation of such comprehensive care of these patients addressing both the locoregional controls along with social and psychological support.
During the ongoing COVID-19 pandemic globally, the problems of management of cancer have escalated and become more complicated than ever before. The pandemic situation has imposed travel restrictions, use of physical distancing norms and lots of psychological stress which has, in turn, resulted in issues of poor compliance to the management of these patients suffering from advanced cancer.
This study was conducted with primary aim of finding out the level of well-being and palliation achieved among patients with fungating breast cancer and secondary aim of determining the association between changes in comfort level and compliance with regards to the clinicotherapeutic and sociodemographic profile of these patients after managing through integrative oncology and palliative care services from this part of our country, especially during the ongoing COVID-19 pandemic.
MATERIALS AND METHODS
A observational study with cross-sectional design based on retrospective secondary data collection and analysis of medical records of newly diagnosed treatment naïve malignant advanced cancer of breast patients during a reference period of 1 year from 1 June 2019 to 31 July 2021 attending Radiotherapy (RT) Department in North Bengal Medical College and Hospital with the following inclusion criteria – biopsy/fine-needle aspiration cytology proven newly diagnosed treatment naïve Stage 3–4 breast cancer as per the American Joint Committee on Cancer 8th Edition and presence of fungating breast cancer with/ without bleeding, ulceration, maggots and pain. Subjects having pre-existing comorbid chronic conditions such as tuberculosis, hypertension, coronary artery disease, diabetes mellitus, autoimmune diseases, renal disease, neurological, other cancers apart from breast cancer, subjects taking long-term other immunosuppressive medications, pregnant and lactating women, bed ridden or unconscious patients and those who had a history of relapse, recurrences or persistence of breast or any other previously treated cancer were excluded from the study.
After initial workup of blood and radiological parameters assessment was done by multidisciplinary team from RT, General Surgery and Cardiology department (dept.).
Thus, the various treatment modalities were prioritised and individualised. All patients were taken care of palliative care dressing and nursing protocols with doctors and nurses in RT dept. and surgery dept., respectively, at initial and subsequent visits. Standard institutional treatment protocol was used for all patients after taking informed consent. All patients were deidentified. The method was cleared by the Institutional Review Board of North Bengal Medical College and waived for need of approval considering there will be no change of management and following standard of care.
The management of patients [Table 1] consisted of locoregional treatment by surgery (palliative toilet mastectomy/modified radical mastectomy (MRM) and RT). Those cases who came with severe pain and bleeding received palliative radiation by Theratron 780 c Cobalt therapy machine before surgery. Various palliative radiation protocols [Table 2] were undertaken as per individual patient’s clinical and logistical factors. Systemic chemotherapy and hormone therapy were also given to suitable patients based on their blood reports and oestrogen receptor and progesterone receptor status. Subjective and objective scores of pain, comfort was rated on a scale of 0–10 based on Revised Edmonton Self-Assessment Score (ESAS)[4] and documented at initial visit and at regular subsequent follow-up. Psychological assessment, societal issues regarding acceptance/rejection and feedback from family about overall status of response to treatment and well-being were noted on a subjective scale [Table 1].
|
| S. No. | Radiation dose fractionation schedule | Number of patients | BED Gy3 Mean=48.56 Gy3 (std. dev.=24.80) |
EQD2 Gy 3 Mean=29.30 Gy3 (std. dev=14.93) |
|---|---|---|---|---|
| 1. | 8 Gy/single fraction (SF) # | 2 | 29.33 | 17.60 |
| 2. | 20 Gy/5 #/1 week | 3 | 46.67 | 28 |
| 3. | 30 Gy/10 #/2 weeks | 3 | 60 | 36 |
| 4. | 35 Gy/10 #/2 weeks | 2 | 75.83 | 45.5 |
| 5. | 35 Gy/15 #/3 weeks | 1 | 60.95 | 36.57 |
| 6. | 50 Gy/25 #/5 weeks | 1 | 83.33 | 50 |
BED: Biologically effective dose, EQD2: Equivalent dose 2
Data were analysed using the principles of descriptive statistics in the form of frequency and percentage and also in tables and diagrams and Statistical Package for the Social Sciences version 22. To correlate comfort outcome after treatment with radiation dose, Spearman’s correlation coefficient was used. Paired t-test was used to calculate the significance of difference in comfort score before and after treatment. Chi-square test of difference of proportions was used to analyse the results of treatment to control various presenting symptoms.
RESULTS
Participants included 19 women and one man (total n = 20), all hailing from the northern districts of West Bengal, with a median distance to travel was 74.5 km (range 4–235 km).
The median age was 50.75 years (range 33–75). All but one was married. The primary caregiver was daughter for 3, husband for 11, son for 4 and son-in-law for 1. Median family income was 17,500 INR (range 5000–40,000 INR).
Clinical presentation
All patients presented with Stage 4 disease and were subjected to multimodality cancer therapy. All of them had fungating breast wound, and seven presented with maggots, 13 had foul odour, seven with wound bleeding and six presented with breast pain [Figure 1].

- Symptoms of patients.
Treatment modality
Even though multimodality treatment was planned, not all patients received all the different types of treatment. Twelve out of 20 patients received palliative radiation therapy, five patients received palliative toilet mastectomy, 17 cases received palliative chemotherapy and 14 cases received hormone therapy [Figure 2]. The most common radiation schedules were 30 Gy/10#/2 weeks and 20 Gy/5#/1 week received by 3 out of 12 (25%) patients, respectively [Table 2]. The mean radiation dose in biologically effective dose was 48.56 Gy3 (std. dev. = 24.80) and equivalent dose (EQD2) was 29.30 Gy3 (std. dev. = 14.93) [Figure 3]. The median fractionation for the whole cohort was 10 fractions.
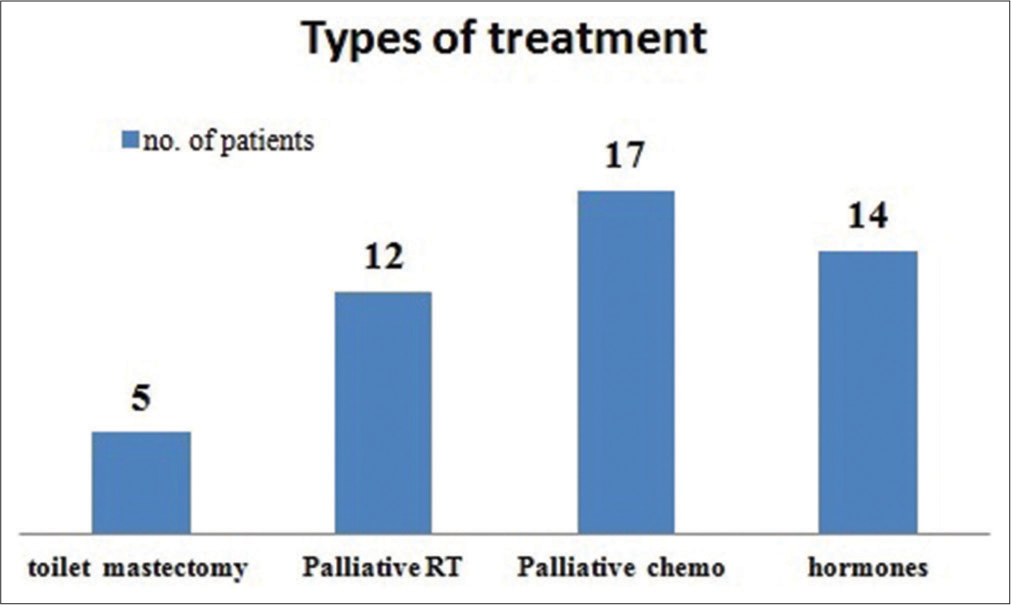
- Modalities of treatment.

- Radiation doses (EQD2Gy3) in various patients.
During the ongoing COVID-19 pandemic, only two patients had become COVID-19 positive but were of mild severity. No patients required admission or expired due to COVID-19 infection.
Outcome
The median follow-up was 13 months (range 4–24 months). Out of seven patients who had maggots, five patients were relieved and only two patients had some residual maggots during follow-up. The statistical analysis revealed Chi-square value was 1.51 and P = 0.06 [Figure 4]. Malodour was relieved in 10 out of 13 patients who presented with foul smell in the initial visit. Hence during follow-up, only three patients had persisting malodour (Chi-square = 2.90 and P = 0.001) [Figure 5]. Average cost of dressing materials was 300 INR (0–600 INR) for 1 month. Bleeding was arrested in all patients with dressing and palliative RT (Chi-square = 2.5 and P = 0.006).
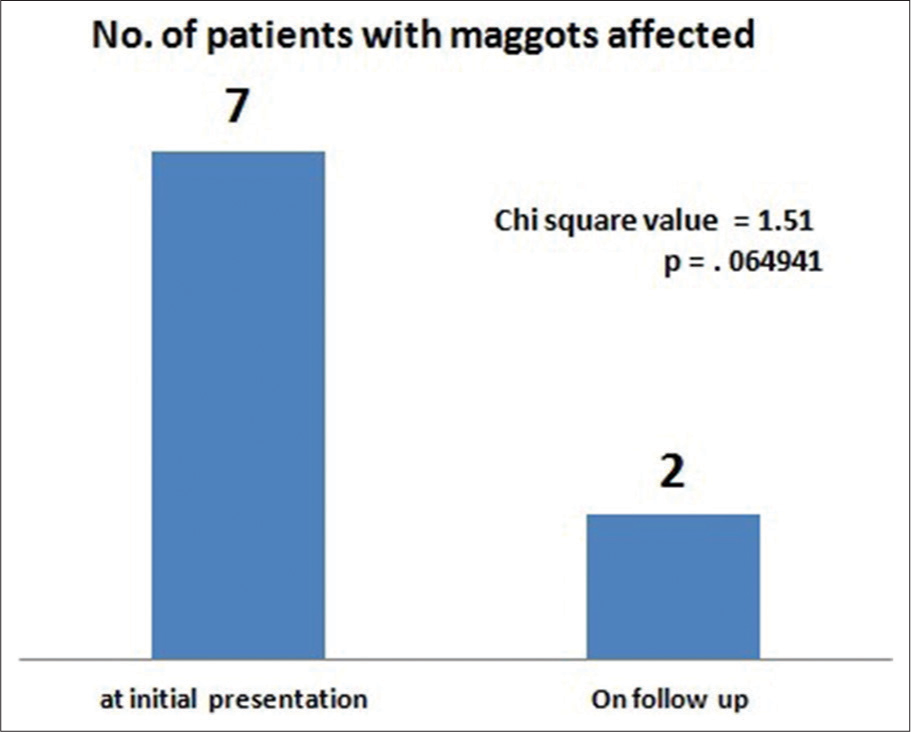
- Maggots in number of patients before and after treatment.
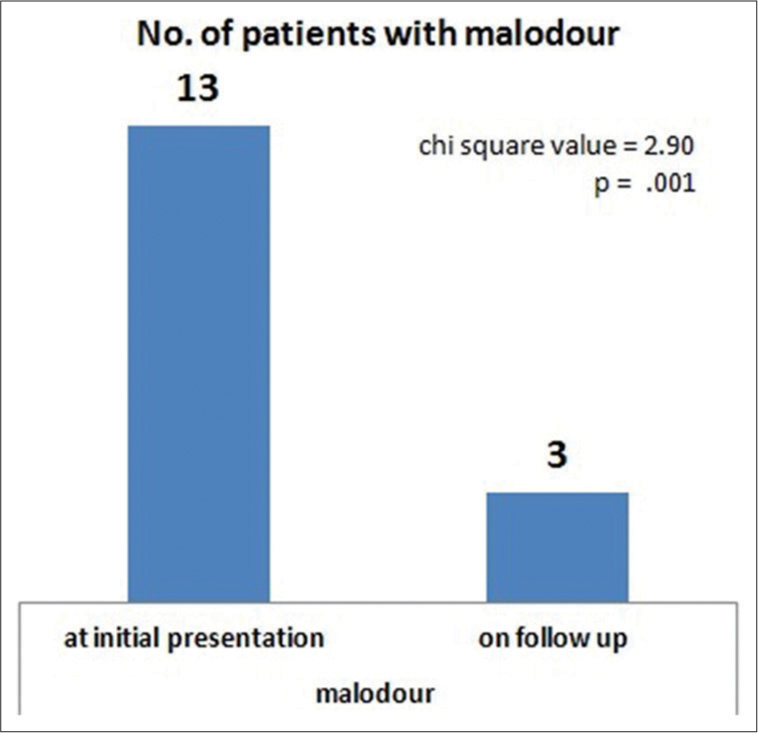
- Malodour in number of patients before and after treatment.
The median pain score was 6/10 in the r-ESAS score initially and at median follow-up of 13 months, it was 3/10 [Figure 6]. Morphine tablets or fentanyl patches could not be given due to non-availability.

- Median pain score (revised edmonton self-assessment score) before and after treatment.
There was a positive correlation of comfort/well-being score due to pain relief and the radiation dose (EQD2Gy3) received. The Spearman’s correlation coefficient was 0.029 but P = 0.9 and hence was not statistically significant [Figure 7]. However, there was a significant amount of improvement in comfort and well-being of the patients as assessed before and after treatment by the paired t-test (t-test = 16.548 and P = 0.000) [Table 3].
| Timeline | Mean value | Standard deviation | 95% confidence interval | Paired t-test=16.548 | |
|---|---|---|---|---|---|
| Before treatment | 3.50 | 0.946 | 3.06–3.94 | P=0.000 | |
| After treatment | 6.75 | 0.851 | 6.35–7.15 | ||
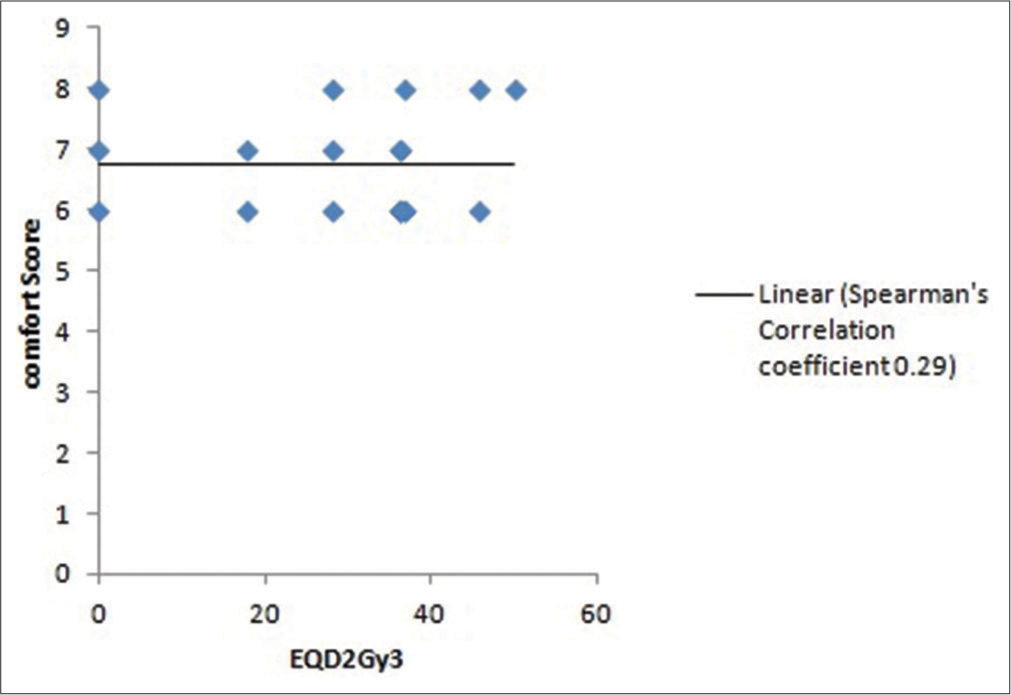
- Correlation of comfort and radiation dose (EQD2 Gy3).
Psychological assessment regarding issues of hopelessness, anxiety, sadness, shame and embarrassment was done taking into the account the most predominant distressing element in them [Table 4]. Overlap of multiple psychological disturbances was found around 3–7 patients. Moreover, the thoughts of persistent cosmetic disfigurement, distorted body image and difficulty in wearing clothes added to the distress level.
| S. No. | Parameters | Number of patients |
|---|---|---|
| Psychological issues | ||
| 4.1.1 | Sadness/depression | 8 |
| 4.1.2 | Anxiety | 4 |
| 4.1.3 | Hopelessness | 8 |
| 4.1.4 | Depression+anxiety | 7 |
| 4.1.5 | Hopelessness+anxiety | 6 |
| 4.1.6 | Depression+hopelessness+anxiety | 3 |
| Social issues | ||
| 4.2.1 | Poor acceptance | 9 |
| 4.2.2 | Moderate level of acceptance | 8 |
| 4.2.3 | No problems from society | 3 |
Subjective feedback
Assessment of compliance and comfort to treatment was assessed at 1 monthly initially for the first 3 months, thereafter at 2 monthly interval for the next 6 months, and then at 4 monthly. There was poor compliance to treatment with regard to dressing of fungating wounds based on home care treatment as guided from the hospital in 10 cases, good for seven and excellent for three cases at the end of 13 months [Figure 8]. Feedback from families was excellent in three cases, satisfactory in 14 cases and unsatisfied in three cases [Figure 9].

- Compliance results.
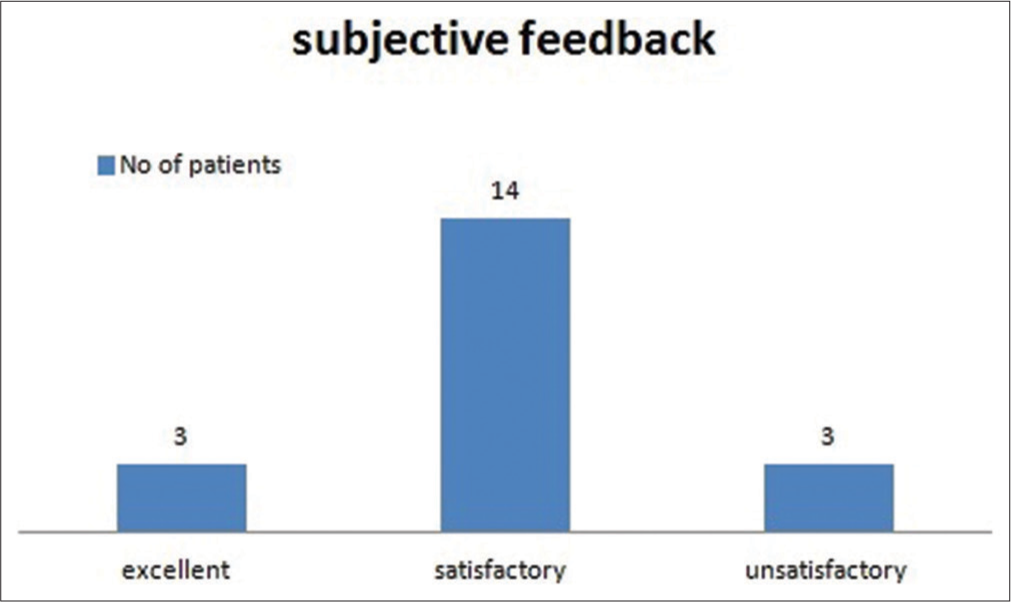
- Feedback from caregivers.
Some of the feedback comments were like:
“I was helpless before and now I am having good amount of relief as my wound is not bleeding anymore after treatment”
“The foul smell has gone totally and no maggots now” “My family has started accepting my condition and has understood how to do the dressing after your guidance”
“My wound has dried and the pain has reduced but I am not able to travel so far for treatment”
DISCUSSION
In this study, it was found out that there has been a considerable achievement to alleviate the distressing symptoms of pain, bleeding, foul smell and maggots with palliative care nursing and radiation, thus increasing the level of comfort and well-being. With the application of topical metronidazole powder and povidone-iodine soaked dressings, nearly 76.9% of patients had got relief from malodour. Even though palliative radiation could arrest bleeding in all patients, pain relief was not significantly correlated with the radiation dose and fractionation schedule as has been observed in the statistical analysis test of correlation. Thus, it implies that any type of palliative radiation dose and fractionation schedule is equi-effective for advanced breast cancer patients. In emergency situations, short course of radiation fractionation schedules can achieve optimum palliation. Along with palliative RT addition of medications such as tramadol, diclofenac tablets and buprenorphine patches can lead to increase in comfort scores.
In the literature, many studies have been reported regarding how to deal with malignant fungating wounds. Malodour is so disturbing that not only patients but also caregivers have vivid memories and recall the pervasive obnoxious experience years later. Hence, various treatment modalities such as use of topical metronidazole, activated charcoal dressings, medical honey, topical iodosorb gel, curcumin, essential oils and green tea extract have been studied.[5] Maggots infestation is a dreaded complication of malignant fungating wounds. There are no definite guidelines and recommendations in literature regarding management of maggots though experimental use of anaesthetic ether and turpentine fumes has proven useful. Pain is one of the common symptoms in many patients and is managed by following the World Health Organisation analgesic ladder, topical use of 2% lidocaine jelly, topical morphine mixed with hydrogel.[6] Palliative radiation is an imperative part of pain management as was observed in a study reported by Vempati et al.[7] that for palliation of pain in ulcerative breast lesions mean dose of 27.54 Gy and mean number of fractions 11 was useful.
Apart from the physical symptoms, patients are often distressed due to a negative impact on their body image which affects their sexual life as well. Caregivers are also stressed and experience burnt out.[8] In this study, 45% of patients had issues with social acceptance and there was hopelessness in 40% of them. PALCARE model approach has been described by Tilley et al.,[9] as a comprehensive approach to address the physical and psychological issues and also explaining them to the caregivers. The added burden of SARS COVID-19 pandemic along with the imposing of lockdown has made the management of cancer even more challenging and particularly for patients presenting with advanced cancer. Elghazawy et al. from Egypt had reported that there was huge impact on the continuum of care of breast cancer patients in middle- and low-income countries due to lots of economic constraints during the ongoing COVID-19 pandemic.[10] Similarly in this study, it was also observed that there was economic burden of bearing the daily cost of dressings at home around 300 INR/month, travelling almost average 74.5 km from respective home to hospital and this was aggravated during the prevailing lockdowns and restricted travel options because of pandemic situation due to COVID-19. As a result, 40% of patients were sad and anxiety was noted in 20% of them thus resulting in lack of compliance in 50% of patients to the treatment protocol and follow-up.
Limitations of the study
This study is the first reported study from a rural medical college hospital in North East India in managing advanced fungating breast cancer patients, particularly during the COVID-19 pandemic situation, and had some limitations. This study was done in a resource-poor centre which is situated in the rural part of North Bengal and hence accessibility to state of the art care in these patients was a challenge. There was non-availability of morphine and fentanyl patches, limited understanding of round the clock palliative nursing care, long distances to travel and prevalence of financial constraints were some of the important issues which made rendering an integrated comprehensive care difficult. Moreover, this study was based on treatment records of limited number of patients over a short period of time. Incorporating more number of patients preferably as a part of multi-institutional prospective study can prove useful in formulating more objective goals of care.
CONCLUSION
This study has shown that proper integration of essential palliative RT, chemotherapy and surgery along with proper palliative nursing care of the advanced fungating breast cancers is effective to bring significant comfort. Palliative radiation must be integrated in the treatment protocol with utmost importance in these patients and any kind of short course radiation dose fractionation schedule is effective to achieve comfort. Compliance to treatment has definitely been hampered particularly because of the prevailing COVID-19 pandemic situation.
In resource-poor centres, in low-income countries and in the midst of the ongoing COVID-19 pandemic, it is challenging and needs lots of triaging based on patient’s clinical symptomatology, sociodemographic profiles and proper assessment.
ACKNOWLEDGEMENT
To all the nursing staffs posted in the Dept. of Radiotherapy in North Bengal Medical College and Hospital.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
Author Dr. Arunangshu Ghoshal is on the Editorial Board of the journal.
References
- Cancer statistics, 2020: Report from national cancer registry programme, India. JCO Glob Oncol. 2020;6:1063-75.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant wounds in women with breast cancer: Feminine and sexual perspectives. J Clin Nurs. 2005;14:56-64.
- [CrossRef] [PubMed] [Google Scholar]
- Occurrence and management of neoplastic wounds in women with advanced breast cancer. Esc Anna Nery. 2014;18:270-6.
- [CrossRef] [Google Scholar]
- A multicenter study comparing two numerical versions of the Edmonton symptom assessment system in palliative care patients. J Pain Symptom Manage. 2011;41:456-68.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of topical treatments to control the odor of malignant fungating wounds. J Pain Symptom Manage. 2010;39:1065-76.
- [CrossRef] [PubMed] [Google Scholar]
- Management of malignant fungating wounds in advanced cancer. Semin Oncol Nurs. 2006;22:185-93.
- [CrossRef] [PubMed] [Google Scholar]
- Palliation of ulcerative breast lesions with radiation. Anticancer Res. 2016;36:4701-5.
- [CrossRef] [PubMed] [Google Scholar]
- An intense and unforgettable experience: The lived experience of malignant wounds from the perspectives of patients, caregivers and nurses. Int Wound J. 2010;6:456-65.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative wound care for malignant fungating wounds: Holistic considerations at endof-life. Nurs Clin. 2016;51:513-31.
- [CrossRef] [PubMed] [Google Scholar]
- Implementation of breast cancer continuum of care in low-and middle-income countries during the COVID-19 pandemic. Future Oncol. 2020;16:2551-67.
- [CrossRef] [PubMed] [Google Scholar]