Translate this page into:
Barriers to the Provision and Utilization of Palliative Care in Africa: A Rapid Scoping Review
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Palliative care (PC) has continued to be less available, underutilized, and unintegrated in many of the healthcare systems, especially in Africa. This scoping review synthesized existing published papers on adult PC in Africa, to report the barriers to PC and to assess the methodologies used in these studies. Eight electronic databases and Google Scholar were searched to identify relevant studies published between 2005 and 2018. Overall, 42 publications (34 empirical studies and 9 reviews) that reported issues related to barriers to adult PC were selected. Three themes identified were individual-level, system-level, and relational barriers. The studies reviewed predominantly utilized cross-sectional and retrospective study design, underscoring the need for more studies employing qualitative design. Findings highlight the need for health education, training opportunities, more funding, communication, and timely referral. Future works could focus on underlying factors to these barriers and ethno-religious perspectives to PC in Africa.
Keywords
Africa
barriers
end-of-life care
Nigeria
palliative care
service provision
INTRODUCTION
The need for palliative care (PC) is rapidly increasing across the globe. This is due to the rising aging populations, successes in utilizing new technology to prolong lives of individuals with serious illnesses, globalization of unhealthy lifestyles, rapid unplanned urbanization, and increases in cancer and other noncommunicable diseases.[12] Yet, there is significant disparity in the provision of PC for individuals with serious and/or life-limiting illnesses.[3] The World Health Organization (WHO) speculates that of the 40 million people in need of PC worldwide, only 14% receive it,[4] implying that many people lack access to PC services, thereby limiting the quality of life they live. In addition, 78% of individuals in need of PC live in the Global South.[4]
The Economist Intelligence Unit (EIU) found that many low- and middle-income countries, particularly countries within Africa, were clustered down in the 2015 quality of death (QOD) index,[1] suggesting that provision of high-quality PC had not gained momentum in the region. There has been continued epidemiological transitioning in Africa to the extent that the incidence of deaths due to cancer as well as other noncommunicable diseases has risen over the past decade.[567] For instance, out of an estimated 9.6 million deaths related to cancer in 2018, Africa accounts for 7.3% as a result of limited access to timely diagnosis and treatment.[6] Furthermore, at the end of 2017, 36.9 million people were living with HIV virus globally, with 940,000 deaths recorded.[78] Yet, Africa remains the most severely affected, accounting for two-thirds of people living with HIV worldwide.[78] Given the low ranking of many African countries in the QOD index and other indices pointing to continued poor PC development in this region, there is need to synthesize studies that explored barriers to PC. This scoping review sought to address this aim.
METHODS
The study design was a scoping review of literature related to adult PC in Africa. Given the paucity of literature about PC in Africa, scoping review was deemed necessary because it is particularly useful in assessing the breadth and depth of literature to map out key themes and help to identify gaps in existing body of knowledge to provide foundation for future research.[91011] The Arksey and O'Malley[12] methodological framework for conducting scoping reviews which consists of a six-step process (identifying the research question, identifying the relevant studies, study selection, charting the data, collating, and summarizing and reporting the data) was utilized. In addition, some recommendations for enhancing scoping study methodology proposed by Levac et al.[10] were utilized in this current study.
Identifying the research question and relevant studies
The specific questions guiding this review are: what is known about barriers to provision and use of adult PC in Africa and how have the questions relating to this been studied? Since no study has broadly captured and summarized barriers to adult PC in Africa, a scoping review was deemed appropriate. Answering these questions involved searching various sources to identify relevant studies. The lead author searched electronic databases (AMED, MEDLINE, PubMed Central, Internurse, Science direct, PsychINFO, Webs of science, CINAL) and Google Scholar to retrieve articles published in English between January 2005 and December 2018. An initial search was conducted in 2017 and was repeated in January 2019. The search terms and the strategy are illustrated below.
Keywords
Palliative care, terminal care, hospice care, end-of-life care, supportive care, chronic disease (s), terminal disease, terminally ill, terminal illness, progressive disease, palliation, death and dying, pain, nursing, hospice, critical care, end of life, Africa, critically ill patients, social support, cancer, non-cancer. The name of individual countries within WHO classification of African region was also used.
Search strategy
-
The electronic search across different databases used the key terms as a single search and combination of the key terms with Boolean operators and truncation (“OR” “AND”). The results were combined with each other as a single search to yield a broader result
-
Citation tracking and hand searching of the articles identified on the reference lists
-
Google and Google Scholar were also searched.
Study selection
The selection of studies was based on the inclusion and exclusion criteria outlined below, while the selection process is shown in Figure 1.
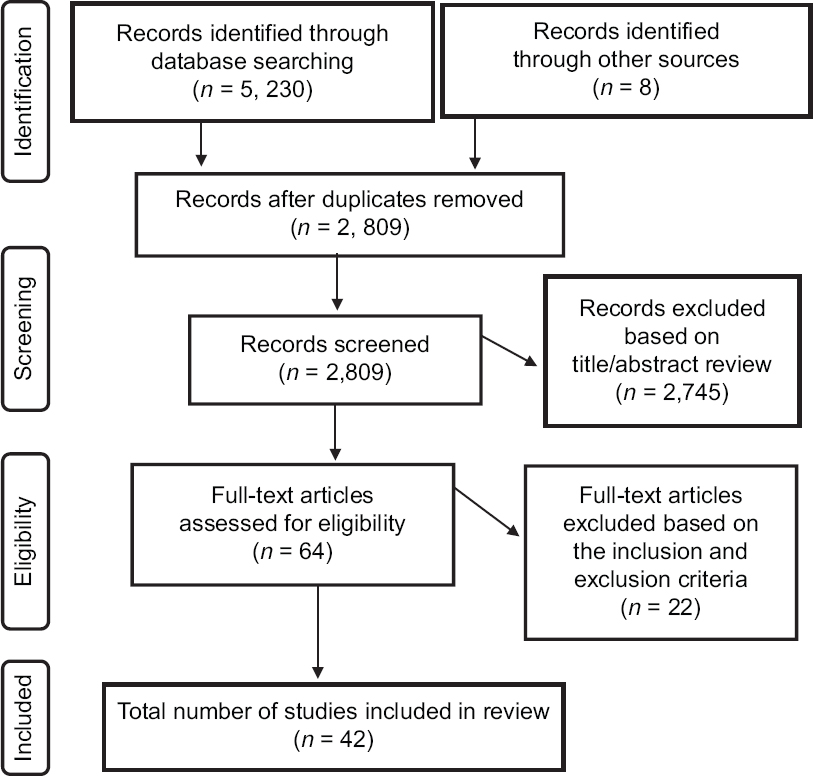
- Flowchart showing literature identification and selection process
Inclusion criteria
-
Written in English language
-
Empirical studies that utilized qualitative, quantitative, and mixed-method published between January 2005 and December 2018
-
Retrospective studies
-
Scoping, systematic, integrated reviewed articles
-
Focused on the provision and use of PC/end-of-life care for adults in Africa.
Exclusion criteria
-
Not written in English
-
Focused on PC for children
-
Published before 2005.
Charting, collating, and summarizing data
Using the data extraction table, the data from included articles were charted independently by all authors in relation to the author (s), publication year, country, title, methodology, aim/objectives, and key findings. All the dissimilarities were then discussed by all authors until consensus was reached [Table 1].
| Authors(s); Year of publication | Country | Title | Study methodology | Study aims/objectives | Relevant key findings |
|---|---|---|---|---|---|
| Elumelu et al., 2013 | Nigeria | Palliative care experiences in breast and uterine cancer in Ibadan, Nigeria | Retrospective review (case file review) | To assess palliative care in a day-care hospice center from June 2008 to December, 2010 | 178 patients with advanced cancer accessed palliative care services within 30 months of its establishment All the patients were glad to have been introduced to palliative care service of the hospital 25 of the patients lived around the hospital environs while 83 (46.6%) of the patients who accessed the services regretted nonavailability of similar services at their home base for continuum of care 100 (56.2%) of the patients who accessed the PC were referred to different parts of the country All the patients accepted PC services Pains and other symptoms presented by the patients were controlled before their discharge |
| Fadare et al., 2014a | Nigeria | Health workers’ knowledge and attitude toward palliative care in an emerging tertiary centre in South-West Nigeria | Cross-sectional study using adapted questionnaire from previous similar study to collect data from 225 healthcare workers (nurses, doctors, pharmacists, social workers, and clinical psychologist) Questions pretested in another healthcare facility before it was used |
To investigate the knowledge and attitude of healthcare workers in a tertiary level hospital in Nigeria where a palliative care unit is being established | Majority of participants (70%) understood PC to be about pain medicine 49.9% considered PC to be geriatric care while 82.3% felt PC is about active care of the dying. Majority of the participants had good understanding about philosophy of PC. Majority also recommended PC for all dying patients and disclosure of the prognosis |
| Kolawole et al., 2013 | Nigeria | Palliative care in developing countries: University of Ilorin Teaching Hospital experiences | Review of 113 patients’ case notes with various forms of malignancy | To investigate experiences over a period of 20 months (May 2009 to December 2010) and highlight the challenges of providing palliative care in a hospital primarily setup to provide curative and preventive healthcare | Pain was the most common indication among all the 113 patients referred for PC Pain and symptom controls, psychotherapy, counseling, spiritual support, home care, and bereavement support were services provided to the patients Inadequate awareness of the services, patient drop-out due to financial constraints to pay for care, and lack of vehicle for home visit were the challenges |
| Fadare et al., 2014b | Nigeria | Perception of nurses about palliative care: experience from South-West Nigeria | Cross-sectional study using adapted questionnaire administered to 100 different cadre of nurses (NO, SNO, PNO, ACNO, CNO, and DDN) | To investigate the knowledge and attitude of nurses toward palliative care in a tertiary hospital in Nigeria | Majority of participants (71.8%) understood PC to be about pain medicine 55% considered PC to be geriatric care while 90.2% felt that PC is about active care of the dying. Majority of the participants had good understanding about philosophy of PC |
| Otegbayo et al., 2010 | Nigeria | Palliative care needs evaluation in untreated patients with hepatocellular carcinoma in Ibadan, Nigeria | Modified needs questionnaires on pain and psychological assessment, thoughts and feelings, and spiritual concerns were administered by one of the authors for 205 patients between February 2007 and May 2009 | To evaluate the physical, psychosocial, and spiritual needs of untreated patients with hepatocellular carcinoma, to determine effective palliative care approach and therefore improve their quality of life when curative therapy is elusive | 71 (35%) of patients were satisfied with pain relief while 117 (57%) were dissatisfied Some patients felt frustrated, incapacitated, and could not cope well with the illness 129 (63%) knew their diagnosis, while 37% did not know what they were being treated for, 95% had no problem with communication with healthcare providers 70% was afraid of death while 89% hoped for healing Some patients believed that God is a doer and could heal them |
| Omoyeni et al., 2014 | Nigeria | Home-based palliative care for adult cancer patients in Ibadan- A 3 years’ review | Retrospective review | To review the spectrum of adult cancer patients involved in homebased palliative care, the services provided, outcome, and benefits | 60 adult cancer patients enrolled for home-based care out of total 787 adult patients enrolled for palliative care between March 2009 and January 2013 Pain was a major compliant for most of the patients (86.3%) Pain relieved within 2 weeks of treatment Services provided are symptoms management, psychosocial counseling, drug administration, safe patient handling, provision of fund, and comfort pack for indigent patients |
| Gurp et al., 2015 | Nigeria | Telemedicine’s potential to support good dying in Nigeria: A qualitative study | Qualitative study using FGD and interview for data collection | To explore Nigerian healthcare professionals’ concepts of good dying/death and how telemedicine technology and services would fit the current Nigeria palliative care practice | Reported barriers to palliative care provision were socioeconomic consequences of being seriously ill, taboos on dying and being ill, equation of religion to medicine, poor implementation of palliative care policy, and restricted access to adequate medical–technical care |
| Akinyemiju et al., 2015 | Nigeria | Palliative care awareness among health care professionals in Nigeria | Cross-sectional study (questionnaires distributed to 100 participants) | To assess the awareness of palliative care among some healthcare professionals in Lagos, Nigeria | 98% has heard of palliative care 72% had learned some aspects of palliative care job without any formal training, but 90% desired training |
| Badru and Kanmodi (2017) | Nigeria | Palliative care awareness among religious leaders and seminarian: A Nigerian study | Cross-sectional study (questionnaires distributed to 302 religious leaders and seminarians) | To determine the level of awareness of religious leaders and seminarians in Ibadan, Nigeria | Only 31.8% have heard of palliative care 12.6% knew hospitals where palliative care is provided 21.6% knew that chaplains are members of palliative care team |
| Downing et al., 2014 | Kenya | Public preferences and priorities for end-of-life care in Kenya: A populationbased street survey | Cross-sectional study (questionnaires distributed to 201 participants) | To explore public preferences and priorities for end-of-life care in Nairobi, Kenya | Majority (56.7%) said that would want to be informed if they had time left The participants preferred that their friends and family’s needs for worry met over their personal need for pain relief Home was the most preferred place for death |
| Harding et al., 2011 | South Africa and Uganda | The prevalence and burden of symptoms amongst cancer patients attending palliative care in two African countries | Survey using The Memorial Symptoms Assessment Schedule Short Form | To determine the symptom prevalence and burden among advanced cancer patients in two African countries | The five most prevalent symptoms among the 112 patients recruited for this study were pain, feeling drowsy, sad, worrying and lack of energy with pain, weight loss, sexual problems, lack of energy, and I do not like myself being the most severe symptoms |
| Selman et al., 2011 | South Africa And Uganda | Quality of life among patients receiving palliative care in South Africa and Uganda: a multicentered study | Cross-sectional survey using the Missoula Vitas Quality of Life Index (questionnaire) | To describe QOL among patients with incurable, progressive disease receiving palliative care | Out of the 285 who were recruited, patients scored most poorly on function, well-being, symptoms, transcendent, and interpersonal. These patients exhibited significantly poor QOL |
| Grant et al., 2011 | Uganda, Kenya and Malawi | Palliative care making a difference in rural Uganda, Kenya and Malawi: Three rapid evaluation field study | Field study using interview, observation, and documentary review to collect data | To describe the patient, family and local community perspectives on the impact of three communitybased palliative care intervention | Patient valued being treated with dignity and respect, being supported at home which reduced physical, emotional, and financial burden of travel to, and care at the health facilities. Mobile phone facilitated rapid access to clinical and social support network |
| Downing et al., 2015 | Kenya and Malawi | Understanding models of palliative care delivery in sub-Saharan Africa: Leaning from programs in Kenya and Malawi | Case study evaluation | To define the models used, contextualize them, and identify challenges, best practices, and transferable lessons scale-up | Specialist, district hospital level, and community level were the three identified models of palliative care delivery Models closely associated with physical settings of services |
| Ndiok and Ncama (2018) | Nigeria | Assessment of palliative care needs of patients/ families living with cancer in a developing country | Descriptive study using questionnaire to collect data from 455 patients from two teaching hospitals in Nigeria | To assess palliative care needs of patients with cancer from the perspectives of the patients themselves | The most commonly needs of patients were information on possibilities of treatment and side effects, diagnosis, testing, and physical symptoms Psychological, spiritual, and financial needs were identified as a stressor for patients and their families. |
| Olaitan et al., 2016 | Nigeria | Palliative care: Supporting adult cancer patients in Ibadan, Nigeria | Retrospective study (reviewed case notes for patients enrolled from January to December 2013) | To describe activities of the Ibadan palliative care group and review 1-year holistic care program offered by the team to support patients and their families | Hospital-based care, daycare center, and home-based care commenced in 2008, being the first in Nigeria 189 patients were provided with palliative care in 1 year Pain and symptoms control, financial and spiritual support, counseling, education for patients and families were offered despite the major challenge of late referral and financial constraint |
| Rhee et al., 2017 | African countries | Palliative care in Africa: A scoping review from 2005-2016 | Scoping review | To gain a broad overview of the medical literature regarding palliative care development in Africa and to provide an analysis of this literature alongside the WHO Public Health Strategy Dimensions (services, education, policies and medicine availability, and the activities of professionals and advocates) | Service provision and implementation Medicine availability Policies Education |
| Tapsfields and Bate 2011 | Malawi | Hospital based palliative care in Sub-Saharan Africa; a sixmonth review from Malawi | Retrospective review of the case note (April–September 2009) | To review the 6 months of in-patient palliative care services at Tiyanjane clinic | 137 out 177 patients’ case notes were retrieved and reviewed Pain was the most commonly reported symptoms, followed with others such as unable to walk, shortness of breath, weakness, anxiety, and depression Analgesic drugs were prescribed to 117 patients 89 (65%) of the patients were discharged home but follow up planned for only 45 (51%) patients, while 26% died during hospital admission The palliative care team was involved with provision of care for the average of 6.3 days (between 1 and 39 days) |
| Katumbo et al., 2017 | Congo | The nurses’ knowledge and attitude towards the palliative care in Lubumbashi Hospital | A cross-sectional descriptive study (questionnaires administered to 112 nurses) | To assess the nurses’ knowledge and attitude toward PC among nurses working in selected hospitals in Lubumbashi | 69 (70.5%) out of 112 had poor knowledge level of palliative care. Only 33% had good knowledge Most of the nurses’ attitude toward palliative care was favorable |
| Agodirin et al., 2017 | Nigeria | Pattern of breast cancer referral to palliative care and the complimentary role of a palliative care unit in a resource limited country | Retrospective review of breast cancer patients referred to pain and palliative care unit between May 2009 and June 2014 Interview by the nursing staff to shed light on some of the record and clarify the findings |
To describe the pattern of referral and the complimentary role of palliative care | 94% of 101 patients reviewed was found to have presented to PAPU in advanced stage most at stage 3 and 4 Communication and counseling, pain control, home visitation, telephone contact, and sourcing for financial aid were the services provided by the palliative care team |
| Lakew et al., 2015 | Ethiopia | Assessment of knowledge, accessibility and utilisation of palliative care services among adults’ cancer patients at Tikur Anbesa specialised hospital, Addis Ababa, Ethopia, 2014; a cross-sectional institution based study | Survey (crosssectional institutionbased study using questionnaire to collect data from 384 patients with cancer) | To assess the knowledge, accessibility, and utilization of palliative care services for adults’ cancer patients by their perspective at Tikur Anbesa Specialised Hospital (TASH), Addis Ababa, Ethiopia | 62.2% of 384 had previous knowledge for cancer PC services 89% reported problem with accessibility of PC services |
| Kassa et al., 2014 | Ethiopia | Assessment of knowledge, attitude and practice and associated factors towards palliative care among nurses working in selected hospital, Addis Ababa, Ethiopia | Survey (a crosssectional quantitative study design using questionnaires to collect data from 341 nurses) | To assess knowledge, skills, attitudes, and associated factors with PC in nurses working in selected hospitals in Addis Ababa, Ethiopia | 104 (30.5%) of 341 nurses had good knowledge while 259 (76%) had favorable attitude toward PC Working in medical and surgical wards, individual’s level of knowledge, and participation in PC training were positively associated with knowledge and attitude of the nurses 76.2% of the nurses had poor knowledge toward PC Only 54.2% of them initiated PC discussion during diagnosis, while 285 (83.6%) reported hiding truth from patients |
| Allsop et al., 2018 | 21 countries in African region | A survey of mobile phone use in the provision of palliative care services in the African region and priorities for future development | Survey | To identify the current mHealth use in PC service delivery, potential barriers to mHealth use, and provider priorities for research development | mHealth approaches were reported across 71.4% of services in which respondents were based Barriers to mHealth research include patients not having access to phones, mobile network access, and limited access to expertise and hardware required for mHealth Research priorities were identified which included exploring ways of incorporating mHealth into patient care and ensuring access and relevance of mHealth for patients and health professionals |
| Harding et al., 2014 | Kenya and Uganda | Palliative care-related self-reported problems among cancer patients in East Africa: A two-country study | Cross-sectional design (adults with advanced malignant disease gave self-reported data to the African POS) | To measure the 3-day period intensity of multidimensional problems (physical, psychological, social, and spiritual) among advanced cancer patients in Kenya and Uganda | The worst ranked POS items were pain and information |
| Clark et al., 2007 | 26 African countries | Hospice and palliative care development in Africa: A multimethod review of services and experiences | Review of literature, in-depth qualitative interview with key personnel Field visit to Uganda, South Africa, Zimbabwe, Tanzania, Kenya, Malawi, and Botswana |
To provide a Fuller evidence-based concerning what palliative care provision presently exists in the countries of Africa and to generate intelligence on barriers to development and how they may be overcome | Opioid availability Categorization of development |
| Opoku (2014) | Ghana | Health and care development: An exploration of factors that hamper better palliative care in sub-Sahara Africa | Mix-method design using interview and questionnaires to collect data from 65 healthcare professionals and 50 members of the general public | To identify the factors that are impeding palliative care development in Ghana | Many respondents from general public had little knowledge about PC Religio-cultural attitudes toward death and dying, high cost of care, and lack of fund for the provision of palliative care were identified as hampering palliative care in Ghana |
| Mkwinda et al., 2016 | Malawi | Palliative care needs in Malawi: Care received by people living with HIV | A qualitative explorative design, using interview to collect data from 18 patients across three healthcare facilities | To explore the needs of PLWHA concerning care received from primary caregivers and palliative care nurses in Malawi | PLWHA needed knowledge from nurses in several areas which affected decisionmaking and also need proper care, financial and nutritional support from the nurses |
| Uwimana and Struther, 2007 | Rwanda | Met and unmet palliative care needs of people living with HIV/AIDS in Rwanada | Descriptive crosssectional study using questionnaire and interview to collect data from 306 participants | To identify palliative care needs of PLWHA in selected areas of Rwanda | Over 50% of PLWHA reported particularly the need for pain relief, symptom management, nutritional support, financial assistance Inadequate policy and resources were the main obstacles to the provision of optimal palliative care Over 50 of the professionals reported that they were not trained in palliative care |
| Harding and Higginson 2005 | Sub- Sahara Africa | Palliative care in sub-Sahara Africa | Review of paper from 1966 to 2003 | To describe the African context for palliative care, identify factors that lead to sustainability, maximum coverage, and efficient referral systems, and highlight examples of good practice through analysis of models of palliative care and evaluation findings | Home and community-based care has been successful, but community capacity and resources and clinical supervision necessary to sustain care are lacking Opioid availability is a barrier Service model Policy |
| Sharket et al., 2018 | Around the world | National palliative care capacities around the works: Results from the World Health Organisation noncommunicable diseases country capacity survey | Survey | To monitor the global status of palliative care and evaluate the progress | Findings related to African region are: There was 40% funding for palliative care in AFR 54% OF AFR have national policy for NCD includes palliative care and policy is operational Only 14% of AFR have oral morphine in more than 50% pharmacies 9% of AFR have home-based or community palliative care |
| Rhee et al., 2018 | 7 African countries | Factors affecting palliative care development in Africa: in country experts’ perceptions in seven countries | Qualitative design using interview to collect data from 16 palliative care experts | To identify key factors affecting PC development in African countries from in-country PC experts’ perspective | Lack of palliative care education, limited availability/accessibility to morphine, lack OF standardization in implementation, lack of funding, poverty and disease burden were the identified challenges |
| Lynch et al., 2013 | 40 countries of the world | Mapping levels of palliative care development: A global update | Multi-method approach (review, in-country experts were asked to provide information | To categorize palliative care development, county by country, throughout the world, showing changes over time | In Africa, no palliative care services could be identified in 28 countries Uganda was only African country in Group 4b while other African countries were categorized in Group 4a, 3a, 3b, 2, and 1 |
| Nwabuko et al., 2017 | Nigeria | Multiple myeloma in Niger Delta, Nigeria: complications and the outcome of palliative interventions | Retrospective study (a 10-year multicenter review) | To bring to the fore the complications experienced by people living with MM in the Nigeria-Delta region of Nigeria and the outcome of various palliative intervention | Majority (61.5%) presented in Durie- Salmon stage III Pain, anemia, nephropathy, and hemiplegia were the complications presented by the patient Inadequate PC accounts for major complication (their conclusion) |
| Wright et al., 2008 | 234 countries around the world | Mapping levels of palliative care development: A global view | Multi-method approach (reviews, grey literature, opinion of experts) | To categorize palliative care development, county by country, throughout the world, and then depict this development in a series of world and region map | Palliative care was found to be unavailable in most of the African countries though there some evidence of capacity building and localized palliative care provision is some African countries |
| Adenipekun et al., 2005 | Nigeria | Knowledge and attitudes of terminally ill patients and their families to palliative care and hospice services in Nigeria | Survey (questionnaires administered to 130 participants) | To assess the knowledge and attitudes of patients and their relations to palliative care and hospice services and to fashion out appropriate services for the patients | 94 (72.2%) had no knowledge of palliative care regardless of level of education and social status 106 (83%) desired to have hospice established in every community, this again was regardless of tribe |
| Omipidam et al., 2013 | Nigeria | Palliative care: An alternative to euthanasia | Qualitative design using interview to elicit data from terminally ill patients | To show case palliative care as an efficient alternative to euthanasia for terminally ill patients | The request for euthanasia and/or assisted suicide are largely due to the fear of being a burden and abandoned by families and relatives |
| Lewington et al., 2012 | Uganda | Provision of palliative care for life-limiting disease in a lowincome country national hospital setting: How much is needed | Qualitative design using interview to elicit data from 78 lifelimiting patients | To measure the magnitude of palliative care needs among hospital inpatients | Social problems included an inability to work, having unaffordable medical expenses, limited access to food, and need to increase faith support that were the needs expressed by the patients |
| Fraser et al., 2017 | Uganda and Kenya | Palliative care development in Africa: Lesson from Uganda and Kenya | Review | To examine and compare strategies used to promote the development of palliative care in Uganda and Kenya in relation to five domains (education and training, access to opioids, public and professional attitude, integration into national healthcare systems and research) | Both countries have implemented all five domains to develop palliative care Both countries have integrated palliative care into the national healthcare system and educational curricula, the training of health care providers in opioid treatment, and the inclusion of community providers in palliative care planning and implementation. Research in palliative care is the least well-developed domain in both countries |
| Hannon et al., 2016 | Lowand middleincome countries | Provision of palliative care in low- and middleincome countries: Overcoming obstacles for effective treatment delivery | Review | To examine approaches to overcome barriers that continued to affect the availability of palliative care low- and middleincome countries | Healthcare delivery and integration into National health systems Access to opioids medications Research Education and training Attitude toward palliative care |
| Nnadi and Singh, 2016 | Nigeria | Knowledge of palliative care among medical interns in a tertiary health institution in North-western Nigeria | Quasi-experimental interventional study | To ascertain the existing knowledge of palliative care among medical interns and determine the effect of a structured educational intervention on improvement of their knowledge level | 11 participants out of 49 had poor knowledge level of palliative care in the pretest but this improved with only 2 medical interns still with poor knowledge after postintervention Good knowledge appreciates from 18.4% to 28.6%, while very good knowledge rise from 20.4% to 38.9% after intervention 57% had had poor knowledge of the constituents of terminal care They exist positive relationship between the number of sources of information and the knowledge level of palliative care |
| Eke et al., 2016 | Nigeria | Knowledge and perception of healthcare providers towards palliative care in Rivers State, Nigeria | Cross-sectional study | To evaluate the knowledge and perceptions toward palliative care among healthcare providers in Rivers State | 88% had previously heard of palliative care but less than 47.4% were aware of the interdisciplinary facet of this service 83.3% believed that terminally ill patients should benefit from palliative care, whereas some believed that everyone should benefit from palliative care |
WHO: World Health Organization, POS: Palliative Outcome Scale, NO: Nursing Officer, SNO: Senior Nursing Officer, PNO: Principal Nursing Officer, ACNO: Assistant Chief Nursing Officer, CNO: Chief Nursing Officer, DDN:Deputy Director of Nursing, PLWHA: People Living With HIV/AIDS, AFR: African Region, PC: Palliative Care
Data analysis and synthesis
Descriptive thematic content analysis of the various sources was undertaken to identify reoccurring themes that provide an overview of the breadth of the literature as recommended by Arksey and O'Malley.[12] Specifically, each paper that met the inclusion criteria was read in full; subthemes were identified and recorded in a data extraction sheet created by the lead author. All the co-authors reviewed and grouped the subthemes independently to broader generic themes. Ambiguity and differences in individual analysis were discussed by the research team to arrive at a consensus. In addition, key methodological limitations identified from all the included papers were recorded in the data extraction sheet, but full-quality assessment was not conducted because it is not consistent with scoping review methodology.[13] The three themes with subthemes that emerged are presented next.
RESULTS
There were various categories of eligible studies among the 42 papers included in this review: retrospective study (n = 7), quantitative study (n = 21), qualitative study (n = 6), reviews (n = 8), and mixed-method study (n = 1). The empirical studies originated from nine African countries (Nigeria, Uganda, Ghana, Kenya, South Africa, Malawi, Congo, Ethiopia, and Rwanda). The findings from the three themes are reported below.
Theme one Individual-level factors influencing palliative care
This theme is presented in two subthemes: first, factors specific to healthcare professionals and second, factors related to patients and their families.
Knowledge and attitude of healthcare providers
The knowledge and attitude of the healthcare providers (physicians, nurses, pharmacists, social workers, medical interns, medical students, and the clergymen) were one of the dominant issues featuring in nine empirical studies and four reviews. Majority of nurses, doctors, and other medical staff were reported to be aware of PC,[141516] contrary to 61.8% of religious leaders and seminarians who had not heard of it.[17] Two studies conducted in Nigeria utilized questionnaires for data collection and concluded that healthcare professionals had good knowledge about PC because most the nurses and doctors understood PC to be active care for the dying, thought that PC was about pain or geriatric medicine, and felt that PC recognizes death as a normal process and affirms life.[1819] However, a similar study conducted in a different region of Nigeria reported that healthcare professionals had insufficient knowledge on the interdisciplinary nature of PC, service users who could benefit from palliation, and components of PC.[1516] These findings corroborate with studies which reported that only a few nurses selected from some hospitals in Congo and Ethiopia had good knowledge of PC.[2021]
The study by Kass et al.[20] acknowledged that nurses who had formal training in PC had greater knowledge than others who had no such training, while other sociodemographic variables had no association with level of knowledge. Nnadi and Singh[16] reported positive relationship between the number of sources of information and knowledge level about PC. In addition, they also stated that medical interns' PC knowledge level improved the following analysis of postintervention questionnaires from posteducational intervention lectures.[16] The authors report that their findings underscore the need for inclusion of PC into the school curriculum at both undergraduate and postgraduate medical and nursing education.[16]
In the three studies mapping the level of PC development across several countries of the world, Kenya, Uganda, and South Africa were three out of 47 African countries that were consistently placed in the group of countries with a broad awareness of PC by healthcare professionals and local communities.[222324] In contrast, 12 African countries (Botswana, Congo, Egypt, Malawi, Zambia, Zimbabwe, Nigeria, Morocco, Gambia, Tanzania, Sierra Leone, and Swaziland) were grouped among countries that had partial/local awareness of PC.[2223] The 2015 QOD Index conducted by the EIU reported that Uganda and Zimbabwe were the only two countries in the African region that ranked topmost in the category of community engagement. This implies that there were African countries where healthcare providers and nonmedical members of the society had some awareness and understanding of PC.[1] The countries where the public and healthcare professionals were reported to have limited understanding and awareness of PC included Malawi, Morocco, Nigeria, Egypt, Ethiopia, Ghana, Kenya, South Africa, and Zambia, while Botswana was the only country which was reported that healthcare professionals and other members of the public had no awareness or understanding of PC.[1] Regardless, four studies reported that all participants (healthcare professionals) had favorable/positive attitudes about PC.[19202125] Positive attitude toward PC shown by nurses was found to be associated with higher levels of education, working in medical wards, and PC training, but age, gender, and work experience had no significant association with attitude toward PC.[20]
Factors related to patients and caregivers
Nineteen papers explicitly discussed awareness of PC, knowledge and attitude, poverty, late presentation, and religion as the factors peculiar to the patients and their families which impacted on the use of PC. Substantial differences in the awareness of PC existed among patients and their families in 47 African countries.[122232426] Uganda, Kenya, and South Africa were three countries where local communities and society, in general, had a broad awareness of PC, whereas local communities in other African countries had only partial awareness of PC.[222324] These findings lend credence to findings reported by Opoku,[25] where 79 out of 115 respondents in Ghana indicated their awareness and knowledge about PC, although the majority of these participants were neither aware of the healthcare settings that provided PC services, nor were they aware of persons who had received PC in Ghana. Conversely, three studies found that majority of patients and their family members had no knowledge of, and were inadequately aware of, PC and hospice care services.[272829] However, it was reported in the 2015 QOD that no public awareness or understanding of PC exists in Botswana.[1] Two studies provided insights that the level of education impacted on whether respondents had, or had no knowledge of PC,[2729] indicating that higher educational level was associated with higher level of awareness/knowledge. Remarkably, there was consensus in the literature that patients desired knowledge about PC, particularly in respect to the causes of cancer, treatment options,[30] as well as aspects of PC, which would require decision-making.[31] Although agreement existed in the literature about poor public knowledge of PC in many of the African countries, most of the patients from Nigeria, Ghana, Uganda, and Zimbabwe demonstrated a positive attitude toward PC through their expression of acceptance and willingness to receive PC.[252627]
Overall, the reviewed evidence indicated that the public (patients and their families) were unlikely to seek PC because of their inadequate knowledge of it. It could also be for reasons related to cultural acceptance of spiritual and traditional care practices since they were keen to seek care from churches, mosques, spiritual homes, and traditional medicine people.[2526] The few patients and their families who were knowledgeable about PC, as well as those without knowledge of PC, often presented themselves for PC in the healthcare setting at the advanced stage of their illness, and this accounted for complications and poor quality of life.[263233] Late presentation of illness was further complicated by poverty and the religious beliefs of the patients and their families. Specifically, most of the patients perceived that PC was expensive, and therefore, they were reportedly unable to pay due to poverty and lack of health insurance coverage, leading to a high rate of patient drop-out, stoppage, or restricted access to PC.[25283435]
Notably, Lewington et al.[34] reported that majority of patients and their families had faith in God, while other articles also showed that patients and their families had inclinations to religious beliefs.[25] The study by Opoku mentioned that religious belief system and sociocultural background were cited in the minority among listed factors that Ghanaians indicated to be obstacles which affect the provision of PC.[25] The study conducted in Nigeria which used a modified needs questionnaire, identified some spirituality concerns in which 86% of the cancer patients felt that “God is a doer,” with few patients of the opinion that God was a supporter and could heal them.[30] Further, an impression about religious belief as a barrier to PC was made in another study conducted in Nigeria where it was reported that most of the patients and their families resorted to an attempt to reconcile hope with religion,[36] leading to hopes for miraculous cures, healing, and recovery.[3036]
Theme two: System-level barriers
Thirty papers reported a range of system barriers at both hospital- and national-level hindering provision and use of PC. These factors (availability and accessibility of PC services, symptoms prevalence, burden and control, education and training for healthcare professional in PC, and political factors impacting on PC) are reported as follows:
Availability and accessibility of palliative care services
Thirteen primary studies reported limited availability of PC, with poor access for the service users in various countries, including Nigeria, Ghana, Kenya, Malawi, and Ethiopia.[25272829303236373839404142] Of these countries, Malawi and Kenya seemed to have the most comprehensive PC services delivered across specialist, district hospital, and community levels.[38] A survey about national PC capacities around the world found that only 20% of the African countries had PC available in primary healthcare for patients with noncommunicable diseases.[42]
A review mapping the level of PC development in Africa reported that as of 2005, PC services were unavailable in 21 out of the 47 countries included in this study,[22] with no progress made by the time 2006 global mapping of PC development was conducted.[24] However, progress was made in 2011, as six countries (Libya, Ethiopia, Namibia, Sudan, Cote d'Ivoire, and Rwanda) had established PC services, although there was still an absence of PC services in 28 of the 54 countries in the African region.[23] Additional progress had been made since 2011 whereby 14 countries increased the number of PC services they provided, of which there were the greatest increases in South Africa (from 120 to 210), Kenya (from 8 to 44), Uganda (from 8 to 34), Tanzania (from 4 to 20), and Nigeria (from 5 to 7).[2324] This trend was also reported in another scoping and narrative review.[2643] Other countries that have also made progress include Mali, Botswana, and Egypt.[23242643] These studies provided useful insights into the extent of the availability of PC services in African countries, showing its lack in some African countries, consistent with the findings in the review by Harding and Higginson,[44] conducted over a decade ago. This suggests lack of PC development over a 12-year period. Similarly, the most current QOD index which assessed the quality and availability of PC services for adults in 80 countries around the world showed that the majority of the African countries were clustered at the lowest part of the index, with Nigeria at the bottom of the index.[1] Nevertheless, the African PC Association (APCA) Atlas of PC in Africa shows that some African countries have made some improvement, with Uganda and South Africa still having the highest number (229 and 160, respectively) of hospice or PC services.[45] Rwanda, Kenya, and Nigeria, have 54, 70, and 17 hospice or PC services, respectively, while Republic of Congo, Equatorial Guinea, and Madagascar have only one hospice or PC services.[45]
Generally, evidence from the literature has shown that availability and provision of PC across African countries are still patchy and its access is limited to seriously and/or terminally ill and dying patients and that it has not been integrated into the mainstream of healthcare systems in almost all the African countries, with the except of Uganda, Kenya, Malawi, Zambia, Tanzania, and Zimbabwe.[232646] Other potential key factors accounting for the limited access include late presentation, inadequate referral systems, client's previous knowledge of PC, and service users' incomes.[282932] Efforts are being made to improve access through the use of mobile phones to deliver PC and home visits by professionals.[324147] However, barriers (patients not having access to phones, limited mobile networks, and access to expertise and hardware) required for the use of mobile phone for PC delivery[28] and lack of vehicles for home visits[47] have made access to PC ineffective.
Symptoms prevalence, burden, and control
Twelve articles examined symptom prevalence for patients and families who had received PC and their experiences in relation to symptom burden and control. The most prevalent symptoms reported by patients and their families included worrying, feeling sad, lack of energy, pain, sexual problems, weight loss, nausea, coughing, constipation, information, family burden, unable to walk, shortness of breath, anxiety, depression, spiritual issues, inability to share feelings, family burden, need for financial assistance, nutritional support, home-based care, and counseling.[283034394041484950515253] The general public, particularly those with chronic and/or terminal illness, were motivated to seek PC so that these symptoms and needs (physical, social, emotional, spiritual, and information) could be addressed.[25] Unfortunately, patients and their families across all these studies were dissatisfied with symptom control as demonstrated by poor scores in all questions contained in the APCA Palliative Outcome Scale (POS)[3451] and the Memorial Symptom Assessment Schedule Short Form (MSAS-SF).[50]
Overall, pain was the most reported complaint and the lowest ranked item in POS and MSAS-SF in terms of satisfaction with care, reflecting high levels of dissatisfaction with PC. Other highly prioritized needs of the patients and their families were information need, family burden, dying at home, and home-based care. These needs were unmet, resulting in poor quality of life,[4853] which had contributed to the request for euthanasia made by some patients, for fear of being a burden to their families or relatives.[54]
Education and training for healthcare professionals in palliative care
Three primary research papers found that healthcare professionals from Rwanda and Nigeria complained that they lacked formal training in PC, although they had learned about some aspects of PC while providing care to service users,[143648] confirming what has been reported in the literature about the development of PC in Africa.[222324] Findings across the previous review papers about PC consistently reported that countries such as South Africa, Uganda, Botswana, Kenya, Zambia, Swaziland, Malawi, Rwanda, Namibia, Nigeria, Ethiopia, Egypt, Cote d'Ivoire, and Tanzania had developed national PC programs which were either being implemented in collaboration with local universities or were planned to be implemented.[2223242643] Uganda and South Africa were the two countries in the African continent recognized to have developed educational centers and academic links forged within universities.[2326] This finding revealed that there is a complete lack of PC education or training institutions for healthcare professionals in most African countries, despite the desire among healthcare professionals across many countries, such as Nigeria, to be trained in PC.[14]
The lack of education or training institutions for healthcare professionals in most African countries was recognized as a possible factor explaining the lack of knowledge of PC among the professionals, which leads to misunderstanding of what PC is, and impacting on care provision.[35] In addition, this shortfall may possibly have contributed to the shortage of staffing for the provision of PC. The finding from the 2015 QOD index showed that many African countries belonged to the category of countries that had a shortage of specialized PC professionals, with the exception of countries such as Uganda, Morocco, and Egypt, which had specialized PC professionals, although specialist PC training is generally not accredited by national professional boards in these countries.[1]
Political factors
The political factors that were described in the 16 included articles as hindering the provision of PC include limited availability/accessibility to opioids, funding, and policy for PC. While three empirical research studies reported on the unavailability of and/or limited accessibility to opioids in countries such as Malawi, Nigeria, Kenya, Namibia, and Cote d'Ivoire,[353649] the survey, which involved 75% of countries in the African region, found that 14% of them had oral morphine available in most of their pharmacies.[42] The likely factors explaining the limited availability/accessibility to opioids included opiophobia, lack of knowledge, inadequate trained workforce for opioid prescription, lack of nurse-prescribing laws/policy, and lack of infrastructure to store and distribute them.[22263555] This limited availability/accessibility to opioids contributed to unmet pain needs for the terminally ill and dying patients.[28404849505152] Although there was limited availability/accessibility of opioids in most African countries, countries such as Uganda, Kenya, Malawi, Zambia, Tanzania, Ethiopia, and Zimbabwe were reportedly making great progress to improve their availability and accessibility.[232655] Only South Africa belonged to the countries in which opioid analgesic were available, but access was restricted by bureaucratic forces.[1]
Another identified political factors hindering PC were funding and policies. The multi-method review that mapped the level of PC development in 2007 showed that 26 out of 47 African countries with a known PC activity hugely depend on external funding for PC.[2224] The similar review conducted 4 years later showed there was no significant improvement in the commitment by the government for funding PC because majority of African countries were still reliant on the external financial aid to fund PC except Cote d'Ivoire that has established multiple sources of funding for PC.[23] Poor funding of PC has continued to exist in most of the African countries as shown in the 2015 QOD index and other reviews[1] and as also acknowledged in a narrative and scoping reviews.[2643] The availability of public funding for PC which is one of the three indicators assessed on the category of affordability of care among other five categories in the QOD index showed that few African countries such as Uganda, Ghana, and Kenya had government funding for PC though funds were difficult to access.[1] Nigeria ranked last in this category among other 80 countries assessed in this index, though countries such Malawi, Tanzania, and Egypt also had total absence of government subsidies for individuals accessing PC, unlike other countries (Botswana, Ethiopia, Morocco, South Africa, Zambia, and Zimbabwe) that had a limited number of government subsidies.[1] This could be an indication that most governments in Africa seemed to be generally reluctant in the internal funding of PC.
Furthermore, the healthcare professionals that participated in the empirical study conducted in Nigeria reiterated lack of government funding for PC.[36] Likewise, the in-country experts in PC from Ghana, Kenya, Mozambique, Nambia, and South Africa unanimously reported that their countries have continued to depend largely on external funding for PC.[35] For instance, they reported that the withdrawal of external funding for HIV/AIDS in South Africa caused closure of many hospices.[35] Concordant with previous findings, a survey about countries' capacities for the prevention and control of noncommunicable diseases which included questions on a number of PC development metrics among WHO member states reported that a small proportion of countries in the African region had funding available for PC.[42] This implies that funding of PC may still be one barrier to PC development in African countries. However, these studies did not capture the underlying reasons for this poor funding, suggesting a need for a more comprehensive and in-depth study.
Lack of and/or inadequate policy implementation for PC were revealed as a barrier to provision of optimal PC in the empirical research conducted in Rwanda and Nigeria.[3648] However, these two studies did not provide explanations as to why there was lack/inadequate policy for PC. Other African countries appear to be in a similar situation because only 54% of 35 countries in the African region that participated in the survey conducted by Sharkey et al.[42] had a national policy for noncommunicable diseases, including an operational policy for PC. Other previous reviews have also shown that most of African countries lacked policies for PC.[22232426] However, countries such as Uganda, Kenya, Zimbabwe, South Africa,[222324] Cote d'Ivoire, Rwanda, and Tanzania[2643] were reported to either have integrated PC into healthcare policy or are gaining wider PC policy recognition.
Theme three: Relational factors
Relational barriers pertained to issues related to communication between healthcare professionals and terminally ill patients/families and the referral interprofessional relationships among providers. These were reported in nine studies. In countries such as Malawi, Kenya, and Uganda, some studies reported that terminally ill patients and their families desired advice, information, guidance, and support through regular communication with PC nurses and other healthcare professionals when in the hospital or at home,[3151] but there was limited access to counseling, information, and support.[29] Similarly, the population-based survey of public preferences and priorities in end-of-life care conducted in Kenya found that the public prioritized having information higher than choosing who makes decisions about care at the end-of-life.[52] However, despite the importance placed on the need for communication/information, majority (83.6%) of nurses preferred to hide the truth from the patients, with few nurses providing counseling to the service users in Ethiopia.[20] Most nurses felt uncomfortable holding end-of-life discussions with dying patients,[20] because such a discussion was said to be complicated by taboos about dying of a life-threatening illness in Nigeria.[36] Consequently, some cancer patients were reportedly unaware of what they were being treated for.[30] The review by Hannon et al. also reported that talking about the possibility of death in the presence of a sick person is considered taboo in some African cultures,[26] while bearing bad news is sometimes believed to have caused the terminal illness.[44]
The second relational barrier concerned referral relationships that existed among the providers. It was found that the average length of involvement by the PC team was about 6 days,[49] suggesting that PC was not integrated early into the care of cancer and HIV/AIDS patients in Malawi, possibly due to lack of referral. More clearly, the case notes review of the patients referred to the pain and PC unit (PPCU) of the University of Ilorin Teaching Hospital, Nigeria, from May 2009 to June 2014 found a steady decline between 2010 and 2013 in the number of patients referred to PPCU.[32] This study revealed a lack of commitment to referral of patients for PC by non-PC clinicians. The reasons for the lack of commitment or any underlying referral complexities were not identified in these studies. A prospective study is required for a more in-depth understanding of the PC referral practices among African clinicians.
DISCUSSION
This scoping review provides evidence regarding the multilevel factors influencing the provision and use of PC in Africa and has uncovered the research designs used in these studies. Three articles reported spirituality and existential problems as the barriers to PC in Nigeria and Ghana, though detailed explanation was not provided possibly due to methodological limitations. Still, on individual-level factors, broad awareness of PC existed among healthcare professionals unlike members of the public who had partial awareness of PC across many African countries. Notably, knowledge regarding the meaning and philosophy of PC, team composition, beneficiaries of PC, communication issues, and opioids analgesic remains inadequate among both the healthcare professionals and the public. However, despite the poor knowledge of PC, both the professionals and the pubic have largely shown acceptance of, and a positive attitude toward, it. The research design used in the papers that reported knowledge and attitude implies that their questionnaires elicited information on aspects of knowledge and attitudes that the researcher considered to be a priority, rather than providing an opportunity for the participants to explain and demonstrate their knowledge of PC. Thus, these findings portray a limited understanding of the overall knowledge and attitude of PC among both professionals and the public.
The inadequate knowledge of PC seems to impact on both the system-level factors and relational barriers, thereby influencing the provision and utilization of PC. In this scoping review, it was found that formal education in PC or training institutions for healthcare professionals was lacking in most African countries, thus explaining the inadequate knowledge of PC held by healthcare professionals. Most of the professionals across many African countries (such as Nigeria, Congo, Egypt, South Africa, and Ethiopia) were found to lack competence, and skills, in engaging in end-of-life discussions,[32021] which can be seen as evidence of the lack of aspects of PC knowledge. Arguably, lack/inadequate could have affected the relational factors by making healthcare professionals incompetent in communication with patients and even among themselves. However, a few African countries have been shown to be making efforts to develop national PC program to bridge the gap in knowledge and skills required for the practice of PC.[2223265657] In addition, it appears that dissatisfaction with symptom management, especially pain control, experienced by the patients can also be attributable to inadequate knowledge and skill about PC,[223555] although other bureaucratic challenges, such as policy and funding, were the factors implicated in patients' satisfaction with PC.
Furthermore, this scoping review has revealed that PC services were either unavailable or patchy in many of the African countries. Nevertheless, there had been an increase in the number of PC services available on the continent of Africa, with countries such as Uganda, Kenya, Malawi, Zambia, Tanzania, and Zimbabwe having integrated PC into the mainstream of their healthcare systems.[234356] This review has also identified other potential factors that continue to contribute to limited access and use of PC, such as late presentation of the patients with cancer or other serious illness to the hospital, high cost of care, poverty, and inadequate referral system. The methodology used in most of the articles reported, in this review, suggest that in-depth examination of factors influencing PC using rigorous methods that would include evidence from observed realities is needed in Africa.
CONCLUSIONS
This scoping review revealed barriers to PC in African continent, specifically that millions of people lack access to PC due to issues such as its unavailability, isolated services, poor funding, lack or inadequate policy, and inadequate referral practice. While a few African countries have made good progress, more effort is required to improve the coverage of, and quality services available to service-users. The first scoping review of PC in Africa by Rhee et al.,[43] which included 49 publications, aimed to improve the understanding of the progress of PC between 2005 and 2016, provided findings on medication availability, education, policies, vitality, service provision, and implementation. This scoping review has provided additional findings on relational barriers, and knowledge of, and attitude to PC, and thus has contributed to further advancing the understanding of PC in Africa.
Finally, this review is not without limitations. For instance, the papers included in this review may not have represented the true picture of countries included in this review about the status of PC because of the nonrepresentative sample as well as small sample size in most of the papers included. Thus, the themes generated should be interpreted with caution. We acknowledged that due to the broad scope of the inclusion criteria and the confusion related the interchangeable use of PC with concepts such supportive care, terminal care, end-of-life care, hospice care, best supportive care and comfort care,[58] it is possible that some of articles may have been missed. Despite these limitations, the scoping review has provided useful insights and extended on what is known about PC in Africa.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Economist Intelligence Unit. The 2015 Quality of Death Index Ranking Palliative Care across the World. Available from: http://www.eiuperspectives.economist.com/healthcare/2015-quality-death-index
- [Google Scholar]
- Global Atlas of Palliative Care at end-of-Life. 2014. Available from: http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
- [Google Scholar]
- The worldwide hospice palliative care alliance. J Pain Symptom Manage. 2018;55:S112-6.
- [Google Scholar]
- World Health Organization Palliative Care. 2018. Fact sheet. Available from: http://www.who.int/news-room/fact-sheets/detail/palliative-care
- [Google Scholar]
- World Health Organization. Press Release: Latest Global Cancer data: Cancer Burden Rises to 18.1 Million New Cases and 9.6 Million Cancer Deaths in 2018. 2018. World Health Organization. Available from: https://www.who.int/cancer/PRGlobocanFinal.pdf
- [Google Scholar]
- UNAIDS. Global HIV & AIDS statistcs.2018Fact Sheet. 2019. UNAIDS. Available from: https://www.unaids.org/en/resources/fact-sheet
- [Google Scholar]
- World Health Organisation. 2018. HIV/AIDS. Available from: http://www.who.int/gho/hiv/en/
- [Google Scholar]
- Overview of a formal scoping review on health system report cards. Implement Sci. 2010;5:2.
- [Google Scholar]
- A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5:371-85.
- [Google Scholar]
- Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32.
- [Google Scholar]
- The use of flipped classrooms in higher education: A scoping review. Internet Higher Educ. 2015;25:85-95.
- [Google Scholar]
- Palliative care awareness among health care professionals in Nigeria. 2015. Journal of Clinical Oncology. 33:20548. https://doi.org/10.1200/jco.2015.33.15_suppl.e20548
- [Google Scholar]
- Knowledge and perception of healthcare providers towards palliative care in Rivers State, Nigeria. Port Harcourt Med J. 2015;11:156-60.
- [Google Scholar]
- Knowledge of palliative care among medical interns in a tertiary health institution in North-western Nigeria. Indian J Palliative Care. 2016;22:343-7.
- [Google Scholar]
- Palliative care awareness amongst religious leaders and seminarians: A Nigerian study. Pan Afr Med J. 2017;28:259.
- [Google Scholar]
- Perception of nurses about palliative care: Experience from South-West Nigeria. Ann Med Health Sci Res. 2014;4:723-7.
- [Google Scholar]
- Healthcare workers knowledge and attitude toward palliative care in an emerging tertiary centre in South-west Nigeria. Indian J Palliat Care. 2014;20:1-5.
- [Google Scholar]
- Assessment of knowledge, attitude and practice and associated factors towards palliative care among nurses working in selected hospitals, Addis Ababa, Ethiopia. BMC Palliat Care. 2014;13:6.
- [Google Scholar]
- The nurses' knowledge and attitudes towards the palliative care in Lubumbashi Hospital. Am Int J Res Humanities Arts Soc Sci. 2017;18:114-9.
- [Google Scholar]
- Hospice and palliative care development in Africa: A multi-method review of services and experiences. J Pain Symptom Manage. 2007;33:698-710.
- [Google Scholar]
- Mapping levels of palliative care development: A global update. J Pain Symptom Manage. 2013;45:1094-106.
- [Google Scholar]
- Mapping levels of palliative care development: A global view. J Pain Symptom Manage. 2008;35:469-85.
- [Google Scholar]
- Health and care development: An exploration of factors that hamper better palliative care in Sub-Saharan Africa. Europ J Biol Med Sci Res. 2014;2:1-16.
- [Google Scholar]
- Provision of palliative care in low- and middle-income countries: Overcoming obstacle for effective treatment delivery. J Clin Oncol. 2016;34:62-8.
- [Google Scholar]
- Knowledge and attitudes of terminally ill patients and their family to palliative care and hospice services in Nigeria. Niger J Clin Pract. 2005;8:19-22.
- [Google Scholar]
- Palliative care in developing countries: University of Ilorin Teaching Hospital Experience. BMJ Support Palliative Care. 2013;3:222.
- [Google Scholar]
- Assessment of knowledge, accessibility and utilisation of palliative care services among adult cancer patients at Tikur Anbesa Specialised Hospital, Addis Ababa, Ethiopia, 2014: A cross-sectional institutional based study. BMC Res Note. 2015;8:657.
- [Google Scholar]
- Palliative care needs evaluation in untreated patients with hepatocellular carcinoma in Ibadan, Nigeria. Afr J Haematol Oncol. 2010;1:48-53.
- [Google Scholar]
- Palliative care needs in Malawi; care received by people living with HIV. Curationis. 2016;39:a1664.
- [Google Scholar]
- Pattern of breast cancer referral to palliative care and the complimentary role of a palliative care unit in a resource-limited country. Postgrad Med J Ghana. 2017;6:42-6.
- [Google Scholar]
- Multiple myeloma in Niger Delta, Nigeria: Complications and the outcome of palliative interventions. Cancer Manag Res. 2017;9:189-96.
- [Google Scholar]
- Provision of palliative care for life-limiting disease in a low-income country national hospital setting: How much is needed? BMJ Support Palliative Care. 2012;2:140-4.
- [Google Scholar]
- Factors affecting palliative care development in Africa: In-country experts' perceptions in seven countries. J Pain Symptom Manage. 2018;55:1313-2000.
- [Google Scholar]
- Telemedicine's potential to support good dying in Nigeria: A qualitative study. PLoS One. 2015;10:e0126820.
- [Google Scholar]
- Palliative care experience in breast and uterine cervical cancer patients in Ibadan, Nigeria. Int J Pain Sympt Control Palliative Care. 2013;10:1-7.
- [Google Scholar]
- Understanding models of palliative care delivery in sub-Saharan Africa: Learning from programs in Kenya and Malawi. J Pain Symptom Manage. 2015;50:362-70.
- [Google Scholar]
- Assessment of palliative care needs of patients/families living with cancer in a developing country. Scand J Caring Sci. 2018;32:1215-26.
- [Google Scholar]
- Palliative care: Supporting adult cancer patients in Ibadan, Nigeria. J Palliat Care Med. 2016;6:258.
- [Google Scholar]
- Home-based palliative care for adult cancer patients in Ibadan-a three year review. Ecancer. 2014;8:490.
- [Google Scholar]
- National palliative care capacities around the world: Results from the World Health Organization Noncommunicable Disease Country Capacity Survey. Palliat Med. 2018;32:106-13.
- [Google Scholar]
- Palliative care making a difference in rural Uganda, Kenya and Malawi: Three rapid evaluation field studies. BMC Palliat Care. 2011;10:8.
- [Google Scholar]
- A survey of mobile phone use in the provision of palliative care services in the African region and priorities for future development. J Telemed Telecare. 2019;25:230-40.
- [Google Scholar]
- Met and unmet palliative care needs of people living with HIV/AIDS in Rwanda. SAHARAJ. 2007;4:575-85.
- [Google Scholar]
- Hospital based palliative care in Sub-Saharan Africa; a six-month review from Malawi. BMC Palliative Care. 2011;10:12.
- [Google Scholar]
- The prevalence and burden of symptoms amongst cancer patients attending palliative care in two African countries. Eur J Cancer. 2011;47:51-6.
- [Google Scholar]
- Palliative care-related self-report problems among cancer patients in East Africa: A two-country study. Supportive Care in Cancer. 2014;22:3185-92.
- [Google Scholar]
- Public preferences and priorities for end-of-life care in Kenya: A population-based street survey. BMC Palliat Care. 2014;13:4.
- [Google Scholar]
- Quality of life among patients receiving palliative care in South Africa and Uganda: A multi-centred study. Health Qual Life Outcomes. 2011;9:21.
- [Google Scholar]
- Palliative care: An alternative to euthanasia. BMJ Support Palliative Care. 2013;3:229.
- [Google Scholar]
- Palliative care development in Africa: Lessons from Uganda and Kenya. J Glob Oncol. 2018;4:1-0.
- [Google Scholar]
- Global Atlas of Palliative Care at end-of-Life. 2014. London: Worldwide Palliative Care Alliance; Available from: http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
- [Google Scholar]
- The current situation in education and training of health-care professionals across Africa to optimise the delivery of palliative care for cancer patients. Ecancermedicalscience. 2014;8:492.
- [Google Scholar]
- Concepts and definitions for “supportive care,” best supportive care, palliative care,” and “hospice care” in the published literature, dictionaries, and textbooks. Support Care Cancer. 2013;21:659-85.
- [Google Scholar]






