Translate this page into:
Hypercalcemia of Malignancy: An Incidental Finding in Carcinoma Cervix
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hypercalcemia occurs in 30% of patients of cancer at either as apart of paraneoplastic process or due to bone metastases. It is an uncommon finding in gynecological cancers. Most common in ovarian cancers and till date very few cancer cervix with hypercalcemia have been reported. We, hereby, report patient of carcinoma cervix who was found to have incidental hypercalcemia without any associated clinical symptoms.
Keywords
Calcium
carcinoma cervix
humoral
hypercalcemia
INTRODUCTION
About 20%–30% of all patients with malignancy may develop hypercalcemia at some time as a paraneoplastic process or as a result of bone metastases.[1] The risk of hypercalcemia depends on underlying malignancy and stage. Common malignancies associated with hypercalcemia include lung cancer, multiple myeloma, renal cell carcinoma, and breast and colorectal cancers. Lowest rates were reported in prostate cancer. Its occurrence in gynecological malignancies is rare. In a systematic review of humoral hypercalcemia-related to gynecologic malignancies, 34 cases were identified. Twenty-two ovarian, six uterine, four vulvar, and three cervical malignancies.[2] We here report a case of carcinoma cervix who presented with incidental hypercalcemia.
CASE REPORT
A 59-year-old female presented to our outpatient department with complaint of bleeding per vagina and white discharge per vagina for 1 month. She also had a dull ache in the lower abdomen. Her bowel and bladder habits were normal. On clinical examination, proliferative growth was present on the cervical os with obliteration of all fornices with the involvement of the upper one-third of the anterior vaginal wall. The finger was bloodstained. Bilateral parametrium was involved halfway of the pelvic wall, and rectal mucosa was free. Cervix biopsy reported nonkeratinizing squamous cell carcinoma. Contrast-enhanced computed tomography of the abdomen and pelvis reported 6.6 cm × 6.3 cm × 5 cm mass lesions on the cervix with bilateral parametrium involvement but not up to the pelvic wall. Furthermore, fat planes with the urinary bladder and rectum were effaced without any infiltration [Figure 1].
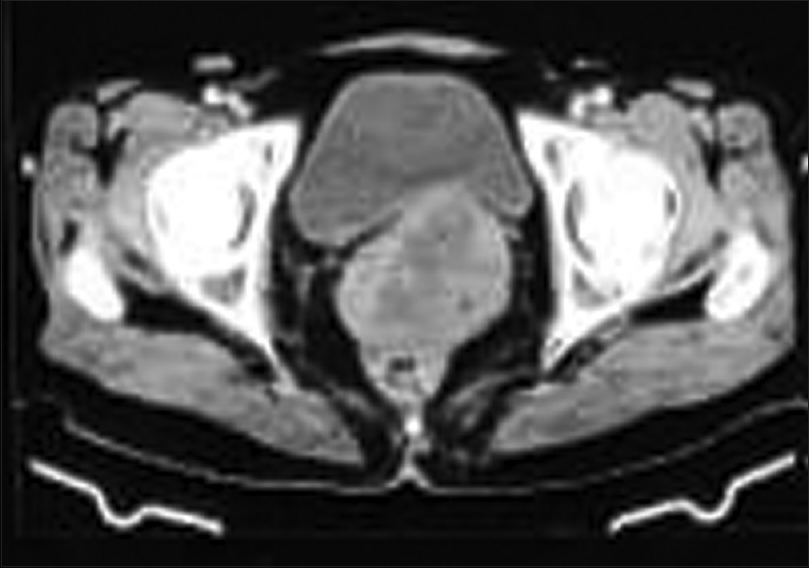
- Axial section of contrast extravasation computed tomography abdomen and pelvis showing heterogeneous mass lesion in cervix with effaced fat planes with the bladder and rectum
Chest X-ray was normal. Her blood investigations reported hemoglobin 8.9 g/dl, total leukocyte count of 19,600/uL, platelet count 297/uL, and red cell distribution width 22%. Her serum calcium was 13.9 mg/dl, blood urea 49 mg/dl, and serum creatinine 1.17 mg/dl. Her estimated glomerular filtration rate was 51 ml/min. Her other blood parameters were within the normal limits. Her Vitamin D was 28.04, and parathyroid hormone PTH was 11.9 pg/ml. Her blood phosphate levels were 1.6 mg/dl. Electrocardiogram done did not show any abnormalities related to hypercalcemia. In view of hypercalcemia, she was managed with intravenous hydration and zoledronate. After 48 h, her serum calcium decreased to 12.2 mg/dl and within the next 2 days was normal. A bone scan was done to rule out metastases, but it was normal [Figure 2].

- 99 technetium-99m bone scan showing no evidence of skeletal metastases
She was considered for definitive concurrent chemoradiation. She completed external radiotherapy but again presented with generalized weakness, drowsiness, and hypotension. She was admitted and blood investigations once again revealed hypercalcemia with serum calcium of 14 mg/dl. She was managed with intravenous hydration and supportive measures. She was considered for supportive care in view of poor general condition.
DISCUSSION
Hypercalcemia in malignancy is four times more common in Stage IV. The most common malignancies associated with hypercalcemia include humoral hypercalcemia of malignancy accounts for 80% of cases and is due to excessive parathyroid hormone-related protein (PTHrP) secretion by the tumor, for example, head-and-neck, esophageal, cervical, lung, and colon cancers.[345] About 20% are accredited to osteolytic hypercalcemia, in which bone metastases cause osteoclast-mediated resorption of the surrounding bone, for example, breast cancer and multiple myeloma. Less than 1% of malignancy-related hypercalcemia is due to the production of calcitriol by the tumor Hodgkin's and Non-Hodgkin's lymphoma.[1] Hypercalcemia typically manifests late in the course of malignancy and portends a poor prognosis. Hypercalcemia is categorized based on serum calcium levels: mild hypercalcemia – 10.5–11.9 mg/dL, moderate hypercalcemia – 12– 13.9 mg/dL, and severe hypercalcemia – >14 mg/dL.[67]
Biochemical investigations for hypercalcemia include serum calcium, serum albumin and if serum albumin is abnormal corrected serum calcium is to be calculated.[8] Hypercalcemia may be associated with both hyper- and hypo-phosphatemia, and hence, serum phosphorus should also be measured. PTH, PTHrP, 25 (OH) D, and 1, 25 (OH) 2D values also can aid in determining the cause of hypercalcemia. In our patient, PTHrp could not be done due to the nonavailability of the test. The primary goal of therapy is the management of the underlying malignancy. Therapy depends on the severity of the hypercalcemia and associated symptoms. It includes intravenous hydration, bisphosphonates, and supportive medication. In our patient, hypercalcemia was an incidental biochemical finding without any clinical manifestation related to increased calcium levels.
The possible mechanism of hypercalcemia in our patient could be humoral cause because of decreased Vitamin D3 levels, borderline normal PTH levels, and the absence of bone metastases.
To conclude, hypercalcemia is rare in gynecological malignancies with very few cases reported till date. Carcinoma cervix is rarely associated with hypercalcemia. The diagnosis includes biochemical investigations to ascertain the cause and radionuclide bone scan rule out metastases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Clinical practice.Hypercalcemia associated with cancer. N Engl J Med. 2005;352:373-9.
- [Google Scholar]
- Paraneoplastic humorally mediated hypercalcemia induced by parathyroid hormone-related protein in gynecologic malignancies: A systematic review. Onkologie. 2009;32:517-23.
- [Google Scholar]
- Hypercalcemia in patients with squamous cell carcinoma of the cervix. Gynecol Oncol. 1979;7:215-22.
- [Google Scholar]
- PTHrP-mediated hypercalcemia: Causes and survival in 138 patients. J Clin Endocrinol Metab. 2015;100:2024-9.
- [Google Scholar]
- Squamous cell carcinoma of the sigmoid colon presenting with severe hypercalcemia. Clin Colorectal Cancer. 2014;13:251-4.
- [Google Scholar]
- Hypercalcemia of malignancy: An update on pathogenesis and management. N Am J Med Sci. 2015;7:483-93.
- [Google Scholar]
- Hypercalcemia of malignancy. In: Jameson JL, de Groot LJ, de Kretser DM, eds. Endocrinology: Adult and Pediatric (7th ed). Philadelphia, PA: Elsevier Saunders; 2016. p. :1125-34.
- [Google Scholar]
- Laboratory approaches for the diagnosis and assessment of hypercalcemia. Crit Rev Clin Lab Sci. 2015;52:107-19.
- [Google Scholar]






