Translate this page into:
Symptom Prevalence in Patients with Advanced, Incurable Illness in Bangladesh
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
There is a significant need for palliative care for patients living in low- and middle-income countries. The presence and intensity of physical symptoms is a major factor influencing the suffering of patients at the end of life.
Objectives:
The primary aim of this study was to determine the prevalence and characteristics of common physical symptoms experienced by patients with advanced, incurable illness in a developing country.
Method:
This study used semi-structured interviews in patients with advanced cancer or HIV/AIDS in Bangladesh.
Results:
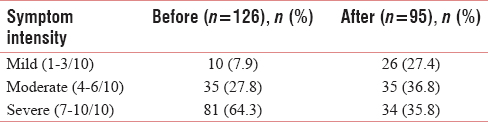
Pain was the most common symptom (70.6%) and was frequently reported to be severe (62.6%). Very few patients received strong opioids to treat their pain (13.7%). Other frequent symptoms included loss of appetite (23.5%) and fever (19.9%). The average number of physical symptoms reported was 3 (range: 0–23). The majority of patients rated their most recent symptom (excluding pain) as severe (64.3%), with 35.8% continuing to have severe symptom intensity despite treatment.
Conclusions:
This study reveals the significant burden of symptoms, and the associated suffering for patients living with incurable illness, in a developing country. Very few patients received strong opioids, despite frequently having severe pain. Frequently, the treatments that patients received did not alleviate their symptoms. Palliative care is vital for the relief of suffering for patients with advanced and incurable diseases, especially in low- and middle-income countries where access to curative treatments may be limited and patients often present to medical personnel when their illness is in an advanced stage or incurable.
Keywords
Cancer
HIV/AIDS
pain
symptoms and symptom management
INTRODUCTION
Palliative care is focused on providing relief of physical, psychological, social, and spiritual symptoms for patients with life-limiting illness and their families. There are 159 million people in Bangladesh, and the gross national income per capita is US$1080.[1] Annual health expenditure per capita is US$16.20, 64% of this spending is out of pocket.[2] In the past 20 years, Bangladesh has made remarkable progress in the field of maternal and child health, and in 2014, the majority (59%) of deaths were due to noncommunicable diseases.[3]
Bangladesh is estimated to have more than 600,000 people in need of palliative care at any point in time.[4] Annually, there are 140,000–200,000 patients newly diagnosed with cancer and 100,000 deaths attributable to cancer.[256] Experience from a local cancer hospital (National Institute of Cancer Research and Hospital) found that 80%–90% of patients with cancer present to oncologists with incurable disease.[4]
Palliative care remains in a very early stage of development in Bangladesh. A recent global mapping exercise found that there are seven palliative care services (public and private) operating in Bangladesh.[7] There is one specialized palliative care institution, the Centre for Palliative Care (CPC) at Bangabandhu Sheikh Mujib Medical University (BSMMU), which provides outpatient consultations, inpatient services, and home care.
Sustained-release oral morphine tablets have been available in Bangladesh since 2006. More recently, immediate-release oral morphine has become available. Restrictive drug control policies; a lack of training among doctors; and myths regarding morphine among health professionals, patients, and the general public prevent many patients from accessing this essential medication.[89]
The WHO has highlighted the importance of improving access to palliative care in low- and middle-income countries.[10] Providing palliative care early in the course of illness is a key public health measure as it can reduce health-care spending on unnecessary care and avoids needless hospitalizations.[11] Understanding the needs of patients with advanced, incurable illness will assist with planning for the provision of palliative care services.
Existing studies have primarily focused on the symptom burden of patients living in high-income countries, and recent systematic reviews found that fatigue, pain, dyspnea, lack of energy, weakness, and loss of appetite were frequent in patients with incurable cancer and other incurable illnesses.[1213] Existing studies from Kerala, India, and Dhaka, Bangladesh, have found that pain, anorexia, insomnia, anxiety, constipation, weakness, and dyspnea were the most common symptoms in patients referred for palliative care services in these settings.[141516]
The primary aim of this study was to better understand the symptom burden of patients with advanced, incurable illness living in Bangladesh. This information will assist in planning of palliative care services in Bangladesh. Our secondary aims were to study the types of treatments which patients received to address their symptoms and their efficacy.
METHODS
Patients
This study is based on data collected from interviews with 221 patients in public hospitals in the seven administrative divisions of Bangladesh. All interviews were completed between May and June 2014. The study was approved by the Directorate General of Health Services (DGHS) of Bangladesh as well as all the institutions and programs involved in the study. Ethical approval was granted by the Institutional Review Board of BSMMU and the Research Review Board of the DGHS, Ministry of Health and Family Welfare. A participant information sheet was given to each participant and all participants provided written informed consent prior to participation.
Patients were invited to participate if they had a confirmed diagnosis of advanced cancer or HIV/AIDS. Additionally, the patient was required to be aware of his or her diagnosis. It is common in Bangladesh for family members to insist that health-care providers do not tell patients their diagnosis. Patients were excluded from the study if they had evidence of cognitive impairment or did not give consent. Patients were informed that they were free to discontinue the interview at any time. No patient requested this and many showed a keen interest to share their experiences with interviewers.
Interviews took place in each of the seven administrative divisions of Bangladesh. Participants were invited to participate from the major city for each division as well as one smaller city in an Upazila (subdistrict of the division). This sample is intended to be representative of patients from across the country. Participants with cancer were recruited from the oncology departments (inpatient and outpatient areas) of the respective hospitals in each division and participants with HIV/AIDS were recruited from local HIV/AIDS support organizations.
Study method
Participants were interviewed using a standardized interview questionnaire. The initial interview questions were developed from the protocol for rapid situational analysis of palliative care in Vietnam and were adapted to be culturally sensitive and translated into Bengali language.[17] The initial interview questionnaire was piloted with ten individuals and further refined. The interview format was semi structured. Interviews were 20–45 min in duration. All interviews were conducted with a trained member of the research team. Interviews were audio recorded and transcribed verbatim.
Demographic information, including age, gender, occupation, religion, and marital status, was collected. Each participant was asked about the type of treatment he or she had received and the health facility where treatment was obtained. Patients were asked about the presence, severity, duration, and frequency of pain as well as pain treatments and their efficacy. Symptom severity was assessed using a numerical rating scale. Participants were also asked about the presence of other physical symptoms, their severity, treatments, and the efficacy of treatment.
Statistical analysis
Data were expressed as either mean or as a percentage of the total number of patients who provided a response.
RESULTS
Patient characteristics
A total of 221 patients with incurable illness were interviewed, 119 females and 102 males. There were 181 patients with cancer and 40 with HIV. The average age of the study participants was 45.5 years (range: 7–95 years). The average number of family members in the patients' household was 5.9 (range: 1–18). The majority of patients (66.8%) reported that the main place they had received medical care was from a publically funded hospital, while a small minority primarily visited a community clinic or subdistrict (Upazila) health center. All the HIV/AIDS patients reported receiving care from one of the several local charitable organizations which exclusively helps patients with HIV/AIDS. Table 1 shows the characteristics of the patients.
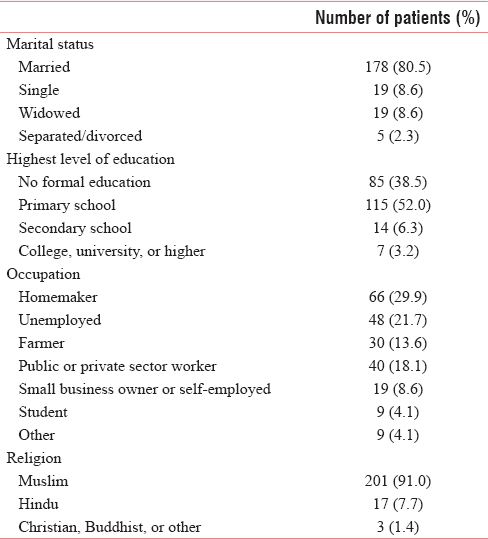
Treatment for the primary disease
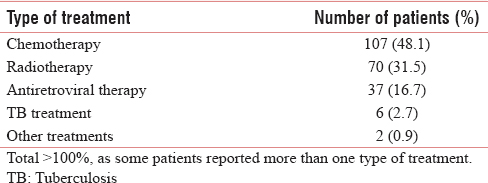
Ninety-eight percent of patients received some treatment for their disease. Patients reported that they were using Western medicine (80.9%), traditional medicine (5.9%), or both (3.2%). The remainder of patients (10.0%) did not know which type of treatment they were receiving. Table 2 shows the common treatments which patients reported that they had received.
Pain frequency and intensity
One hundred and fifty-six patients (70.3%) reported that they had experienced pain during their illness. About half of these patients (51.3%) reported that they had constant pain, while an additional 27.9% reported feeling pain almost every day. Pain which occurred less than daily, but at least once a week (14.9%) or once a month (4.5%), was less common.
Pain treatment
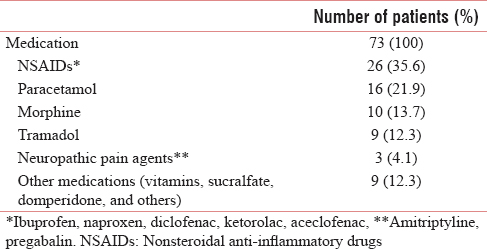
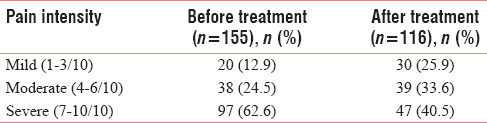
The majority (94.2%) of patients received some treatment for their pain; however, most (57.1%) could not remember the names of the medications that they had received. The types of medications which patients reported receiving are listed in Table 3. Patients were asked to rate the intensity of the pain, using the numerical rating scale: mild (1–3/10), moderate (4–6/10), and severe (7–10/10). Table 4 shows the change in pain intensity with treatment.
Other symptoms
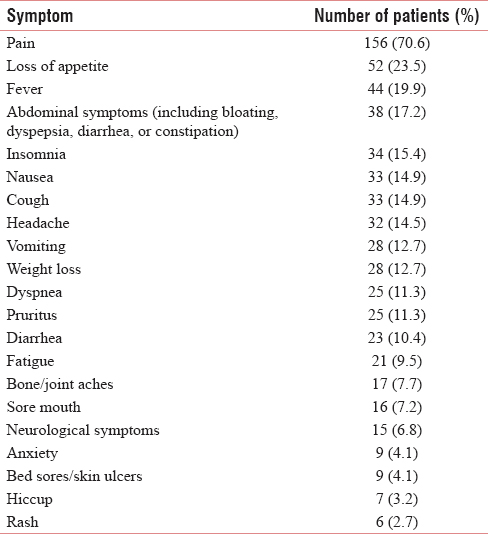
Pain was the most commonly reported symptom. The frequency of common physical symptoms is shown in Table 5. The average number of physical symptoms reported was 3 (range: 0–23). There were 31 patients (14.0%) who reported no physical symptoms. The change in symptom intensity with treatment is shown in Table 6.
DISCUSSION
A number of studies have investigated the symptom prevalence in patients with advanced cancer and other incurable illnesses. However, the vast majority of these studies have focused on the symptoms of patients in high-income countries where access to health care is generally relatively affordable, and there is a relatively comprehensive social security system, and basic needs such as running water, adequate food, sanitation facilities, and electricity are available for all. Providing palliative care in low- and middle-income countries is much more challenging, as poverty limits treatment options, and in addition to medical care, patients often have more basic needs for food and shelter. This study demonstrates the high burden of symptoms of patients with incurable illness in Bangladesh.
Financial problems
In Bangladesh, where almost half of the population lives on <$2/day, health-care expenses can be financially devastating for a patient and his/her family.[1] Health-care costs are a major reason for a family to fall back into poverty due to the high cost of care and the loss of livelihood.[1819] The majority (66.8%) of patients reported using public hospitals, which are the main health service provider in Bangladesh. Bangladesh provides an extensive range of free or low-cost medical services at the community level; however, despite being publicly funded, health care from public hospitals is not free of cost; patients must often pay for medical tests and medications, leading to a substantial financial burden for most patients.[2021] Lack of money often prevents patients from taking regular treatment and many patients simply cannot afford the medications which they are prescribed. The financial situation of most patients is further worsened by the fact that many undergo expensive treatments, such as radiation and chemotherapy, which, given their advanced stage of disease, will not be curative.
Cure-focused health care
Almost all patients (98%) we surveyed were receiving treatment for their primary disease, and the use of cure-oriented treatments such as chemotherapy (48.1%) and radiotherapy (31.5%) was frequent. This finding highlights our own observations in Bangladesh that medical professionals do not consider symptom management and palliative care as important aspects of care, even for patients with incurable illness. Doctors also give little consideration to the financial impacts of their medical recommendations and often recommend invasive and expensive treatments that will not be curative.
Indeed, our previous work has shown that oncologists may perceive the provision of palliative care and pain management as a threat to their career and income.[8] This highlights the urgent need for palliative care training, especially in sensitizing professionals to the importance of palliative care, emphasizing that relief of suffering is a professional responsibility.
Pain treatment
Pain was the most commonly reported symptom in our study, with 62.6% of patients reporting that their pain was severe. Even after treatment, 40.5% continued to have severe pain. Despite the frequency of moderate or severe pain, very few patients we surveyed had received strong opioids (13.7%).
In Bangladesh, knowledge among physicians of how to appropriately prescribe opioids is limited. Our previous work reveals that concerns about addiction and the potential side effects of morphine persist, even among health professionals.[8] Most professionals are unaware of the therapeutic potential of morphine, and many physicians do not know that morphine is available in an oral form and can be used for pain management outside of anesthesiology.[89] Even at a tertiary-level hospital in Bangladesh, the majority of faculty did not feel adequately trained to prescribe oral morphine for cancer pain.[8] A recent study showed that 92% of doctors did not have any prior training in pain management, despite the fact that 47% stated that they would see five or more incurably ill patients a month.[9]
Education and training
In Bangladesh, none of the undergraduate medical colleges have incorporated palliative care into their curriculum.[22] A comprehensive approach to pain management and the important role of opioids in palliative care must be included in medical education to reduce the suffering of patients. Additional efforts are needed to include palliative care in the training of nurses and other health-care workers. Recently, the CPC at BSMMU has started providing introductory palliative care education courses for doctors, nurses, social workers, pharmacists, and volunteers. In addition, a program has been developed to train palliative care assistants to address the critical shortage of trained basic health-care workers. A 5-year residency program in palliative medicine has also been recently started at BSMMU.
Local opioid availability
Adequate pain treatment is also affected by difficulties in accessing opioids due to problems with drug availability. Although morphine is listed on the Bangladesh Essential Drug List, morphine is only available in Dhaka, the capital city. Even within Dhaka, there are only a few hospitals and retail pharmacies where morphine is readily available. For many patients residing outside of Dhaka, the patient or a family member must travel long distances to purchase morphine. Transdermal fentanyl is available, but is prohibitively expensive for most patients. Tramadol, which 12% of patients reported using, is not a restricted drug and is widely available in most areas of Bangladesh without a doctor's prescription. Despite this, few patients reported taking tramadol.
Cultural and societal barriers
Cultural and societal expectations about pain, suffering, and illness mean that patients are unaware that relief of pain is possible and that advanced illness should not mean a life filled with intolerable suffering. Our previous work showed that patients were often concerned about addiction and other potential side effects from morphine, and in many cases, patients view death as a respite from their pain.[8] We found that paracetamol (21.9%) and nonsteroidal anti-inflammatory drugs (35.6%) were the most frequently used analgesic medications. This may be because these medications can be obtained from local pharmacies without a doctor's prescription. Patients may choose to use these medications when they are unable to access medical care due to financial and logistical barriers. On the other hand, these findings also support a previous study which showed that more than 90% of physicians in Bangladesh do not have any training in pain management.[9]
Symptoms
In this study, we evaluated the presence of 21 core symptoms which are common in patients with advanced illness. Pain, followed by loss of appetite, fever, abdominal complaints, and nausea, was the most frequent complaint. Several other studies have examined the symptoms of patients with advanced cancer in South Asia.[141516] Seventy-one percent of patients in our study reported pain, similar to these studies where pain was present in 87%–100% of cases.
Loss of appetite is a common symptom across all studies, occurring in 23.5% of patients in our study, compared with 42%–53% in other studies.[121415] As in many cultures, food and nourishment are very significant for patients in Bangladesh, families often feel that it is vital to feed the patients as their food intake decreases. As the appetite diminishes, family members can become preoccupied with this, spending large amounts of time and energy devoted to preparing food and coaxing the patient to eat. When a patient develops cachexia, families often express feelings of frustration and powerlessness in the face of advancing illness.
Overall, the majority of symptoms were much less common in our study, compared to other studies of patients in South Asia. Our patients had an average of three symptoms, with 14% reporting zero symptoms, compared with an average of seven symptoms in a previous study in Bangladesh.[14] The lower rates of pain and other symptoms observed in our study may be due to the way study participants were selected. In our study, we recruited patients with advanced illness from across the country, not restricting our study to those presenting to a palliative care service. Many of our patients may have been at an earlier stage of illness, when the symptom burden is lower. Additionally, variation in assessment methods and difficulties in defining symptoms may also lead to this observation.[12]
CONCLUSION
This study reveals the significant burden of symptoms and their lack of adequate treatment for those living with incurable illness, across Bangladesh. Our study provides data which can be used to advocate with policymakers about the critical need for palliative care and relief of suffering for patients with advance and incurable illnesses. A comprehensive analysis of the palliative care needs of patients is a valuable tool which can support the development and implementation of national policies for palliative care within a country.
Financial support and sponsorship
This study was funded by the National Institute of Population Research and Training of Bangladesh.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The World Bank Group. 2016. The World Bank Website. Available from: http://www.data.worldbank.org/country/bangladesh
- [Google Scholar]
- World Health Organization: Regional Office For The Western Pacific. In: Bangladesh health system review. Geneva, Switzerland: World Health Organization; 2015.
- [Google Scholar]
- Cancer. 2014. Noncommunicable Diseases (NCD) Country Profiles. Available from: http://www.who.int/nmh/countries/bgd_en.pdf
- [Google Scholar]
- National Institute of Population Research and Training. In: Assessment of palliative care in Bangladesh. Dhaka, Bangladesh: National Institute of Population Research and Training; 2014. p. :177.
- [Google Scholar]
- Comprehensive update on cancer scenario of Bangladesh. South Asian J Cancer. 2013;2:279-84.
- [Google Scholar]
- A fresh look at oncology facts on South central Asia and SAARC countries. South Asian J Cancer. 2012;1:1-4.
- [Google Scholar]
- Mapping levels of palliative care development: A global update. J Pain Symptom Manage. 2013;45:1094-106.
- [Google Scholar]
- The use of morphine to control pain in advanced cancer: An investigation of clinical usage in Bangladesh. Palliat Med. 2010;24:707-14.
- [Google Scholar]
- Physicians knowledge and attitude of opioid availability, accessibility and use in pain management in Bangladesh. Bangladesh Med Res Counc Bull. 2014;40:18-24.
- [Google Scholar]
- Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: Key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387:2133-44.
- [Google Scholar]
- Palliative Care. Fact Sheet No. 402. Available from: http://www.who.int/mediacentre/factsheets/fs402/en/
- [Google Scholar]
- A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58-69.
- [Google Scholar]
- Symptom prevalence in patients with incurable cancer: A systematic review. J Pain Symptom Manage. 2007;34:94-104.
- [Google Scholar]
- Needs of terminally ill patients and their families: An experience with fifty-three patients attending a newly organized palliative care service in Bangladesh. J Bangladesh Soc Anaesthesiol. 2006;19:38-43.
- [Google Scholar]
- Palliative care in Kerala. Problems at presentation in 440 patients with advanced cancer in a South Indian state. Palliat Med. 1996;10:293-8.
- [Google Scholar]
- Palliative care out patient consultation service in a teaching hospital in Bangladesh. Mymensingh Med J. 2011;20:98-103.
- [Google Scholar]
- Findings from a Rapid Situational Analysis in Vietnam. 2006. Publishing Department. Available from: Http://www.thewhpca.org/resources/item/palliative-care-in-vietnam-findings-from-a-rapid-situation-analysis
- [Google Scholar]
- The Impact of Out-of-Pocket Expenditures on Poverty and Inequalities in Use of Maternal and Child Health Services in Bangladesh: Evidence from the Household Income and Expenditure Surveys 2000-2010 RETA-6515 Country Brief. 2012. Manila: Asian Development Bank. Asian Development Bank. Available from: http://www.adb.org/sites/default/files/publication/30152/impact-out-pocket-spending-bangladesh.pdf
- [Google Scholar]
- Paying out of pocket for healthcare in Bangladesh – A burden on poor? Iran J Public Health. 2015;44:1024-5.
- [Google Scholar]
- Community-based approaches and partnerships: Innovations in health-service delivery in Bangladesh. Lancet. 2013;382:2012-26.
- [Google Scholar]
- Health Bulletin, 2015. 2015. Directorate General of Health Services (DGHS), Bangladesh. Available from: http://www.dghs.gov.bd/images/docs/Publicaations/HB%202015_1st_edition_31122015.pdf
- [Google Scholar]
- Conceptual prevalence in palliative care amongst the physicians of Bangabandhu Sheikh Mujib Medical University: A comparison between the post-graduate trainees and the trainers. J Bangladesh Soc Anaesthesiol. 2014;22:26-31.
- [Google Scholar]






