Translate this page into:
Opioid Dispensing Patterns from a Tertiary Care Cancer Hospital during the Nationwide Lockdown in COVID-19 Pandemic
Address for correspondence: Dr. Sushma Bhatnagar, Department of Onco-Anaesthesia and Palliative Medicine, BRAIRCH, AIIMS, New Delhi, India. E-mail: sushmabhatnagar1@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
During the current COVID-19 crisis, striking a balance between adequate pain relief in advanced malignancy patients and avoiding hospitals due to fear of contracting the infection has been the biggest challenge for patients as well as palliative care physicians. This study explored the trends in opioid dispensing for cancer pain before and during the lockdown.
Methods:
The trends were calculated based on an analysis of quantity of all opioids dispensed. March 24, 2020, was considered as a cutoff for analyzing before and during lockdown period dispensing trends. No information regarding individual patients was retrieved in the current study.
Results:
There was a decrease in total morphine, tramadol, and fentanyl patch dispensing parallel to decrease in total number of patients visiting the outpatient department. However, there was a statistically significant increase in per capita opioid dispensing during the lockdown period. There was also an increase in the proportion of cancer pain patients that were dispensed morphine during the lockdown.
Conclusion:
Despite the lockdown, the palliative care team at Institute Rotary Cancer Hospital has continued to provide adequate pain relief to patients that could manage to reach the center. Policy-makers need to be cognizant of the pain relief needs of cancer patients in times when accessing hospitals is becoming increasingly difficult. Cancer-related pain and mortality could well be the next pandemic once the current COVID-19 begins to reduce.
Keywords
Cancer pain
morphine
opioid dispensing
pain relief during lockdown
per capita opioid dispensing
INTRODUCTION
Palliative care is a fundamental right of each and every human being, both on humanitarian and medical grounds. Understanding its essentiality and grave necessity, the World Health Organization (WHO) passed a landmark resolution during the 67th World Health Assembly in 2014 recommending all its member states to incorporate and strengthen palliative care services in the public health care.[1] The new definition of palliative care is the active holistic care of individuals across all ages with serious health-related suffering due to severe illnesses, especially those near the end of life. It aims to improve the quality of life of patients, their families, and their caregivers.[2]
Opioid analgesics form the mainstay of pain management in care of patients with advanced malignancies suffering from moderate to severe pain. Tramadol, morphine, and fentanyl are the commonly prescribed opioid analgesics.[3] Unfortunately, the availability of opioids to the population that needs it the most has always been a matter of grave concern in our country. According to the WHO, 2015 report South East Asian Region lags behind the rest of the world as far as per capita equivalence of morphine is concerned, with a dismal 1.7 mg per capita compared to the global average of 61.5 mg.[4] The Lancet Commission's report of 2017 quantified the existing deep and ugly chiasm of inequalities in medicinal opioid availability access the globe. Overall, of the 298.5 metric tonnes of morphine-equivalent opioids distributed world over in 2012–2013, <0.1 metric tonne was distributed in low-income countries; equating to more than 99% of unmet need. India distributed 43 mg morphine equivalent which was enough to meet only 4% of the total palliative care needs.[5]
In the backdrop of an already compromised accessibility situation, this coronavirus pandemic has added insult to injury. Patients with advanced malignancies suffering with moderate-to-severe cancer pain have been grievously hurt at all levels.[67] With the announcement of a nationwide lockdown, the access to health care has been severely hampered. In compliance with the advisory by the Ministry of Health and Family Welfare, Government of India, and the indigenous hospital infection control guidelines, a large proportion of health-care facilities including workforce and resources have been allocated to dedicated COVID management areas, and all elective procedures have been temporarily withheld, including outpatient services, with the aim to reduce the total number of people exposed to the risk of infection and facilitate the deployment of resources to COVID facilities. With the complete cessation of public transport facilities, accessing a cancer hospital in itself is a major challenge for significant proportion of patients; considering many of them live across state borders and travel to distant cities to avail quality palliative care through general and opioid analgesics (especially morphine), given the poor availability in majority of the cities.[8] All these might substantially increase the cancer burden in terms of increased symptom load and increased human suffering due to increased unmet need.
A huge area of research during the panning out of pandemic will be regarding continued cancer care. This could affect the opioid chain at multiple levels including harvesting, synthesis, transport, distribution, prescription, and dispensing. It might take us a while to truly understand and assimilate the effects that this pandemic has had, how the life of a cancer patient is devastated, how despair is taking roots, how the fundamental right of staying pain-free is being violated.[9] Hence, we wanted to explore opioid dispensing trend during the current COVID-19-related lockdown. This study highlights the continued and uninterrupted dispensing of opioids in general and morphine in particular at our center despite the largest nationwide lockdown in human history, accounting the challenges and triumphs and presenting a comparative overview of per capita morphine prescription before and during lockdown.
METHODOLOGY
Study setting
In accordance with the advisory issued by the Ministry of Health and Family Welfare, Government of India, and the indigenous protocols and guidelines formulated by our institute for the management of non-COVID patients attending a non-COVID setup, all appropriate precautions and measures were undertaken for the safety of health-care professionals and patients. This included abiding by the principles of social distancing, allowing only the patient to enter the clinic, 2 m distancing between personnel, appropriate personal protective equipment donning by the doctors examining patients including a hood, N95 masks, head and shoe covers, nitrile gloves, and coveralls. All patients and attendants were expected to wear masks covering their nose and mouth at all times while they were inside the hospital premises. Regular hand hygiene with alcohol-based hand rub, counseling and educating the patients about the importance of these practices, and avoiding stigmatization were all standard operating procedures followed at the outpatient department (OPD). A digital database has been started recently for all patients attending the OPD with documentation of their telephone number and other details for ease of telemedicine. All patients were also given emergency contact numbers whereby they could tele-consult, avoiding the need to come back to the hospital for minor issues and clarifications; and maintaining the continuum of care both inside and outside the hospital. All medications were dispensed for a period of 1 month to ensure their needs were well covered and unnecessary travel and other logistic hassles averted during the difficult lockdown period; considering a substantial proportion of outpatients attending the pain clinic hail from distant cities and towns outside the National Capital Region.
Methods
This is a retrospective review of oral opioid analgesic prescription patterns during the period of nationwide lockdown, observed at the Pain and Palliative Care OPD, run by the Department of Onco-Anaesthesia and Palliative Medicine located in room number 60 ground floor of Dr. B. R. Ambedkar Institute Rotary Cancer Hospital, a dedicated cancer hospital in All India Institute of Medical Sciences, New Delhi. All opioid prescriptions were reviewed from January 1, 2019, to May 20, 2020. The data concerned the three most commonly prescribed opioids at our center, namely tramadol, morphine, and fentanyl that are prescribed for the management of moderate-to-severe cancer pain. Parameters retrieved from the hospital online records included total number of morphine tablets of strengths 10 mg plain, 10 mg controlled release (CR), 30 mg CR, 60 mg plain; fentanyl transdermal patch 25 μg/h (mcg), 50 mcg and tablet tramadol 50 mg. For the purpose of comparison, time frame from January 1, 2019, to March 23, 2020, was marked as prelockdown era and from March 24, 2020, to May 20, 2020, was marked as postlockdown era. Total number of patients attending the Pain OPD and number of patients receiving opioids was also noted. The annual amount of morphine dispensed, average monthly prescription, and the average per capita daily consumption data was calculated. This was compared to the present average during the lockdown period. The proportion of the total number of patients attending the Pain OPD that were prescribed opioids during the record retrieval period was also calculated and compared between the before and during lockdown periods.
The study included the opioid dispensing records of all patients who attended the pain clinic for pain and other symptom management and also the patents admitted to palliative care unit who were discharged on oral opioids. Patients whose prescriptions were not digitally entered on the online server were not included in the study.
Statistical analysis and ethical aspects
Data analysis was performed using the statistical package SPSS Statistic 20.0 (IBM SPSS Statistics, New York, USA). The significance level was set at α = 0.05, and all tests were two-tailed. Shapiro–Wilk test was used to assess the normal distribution of the data. The comparison of rates of opioid prescription and dispensing was done using an independent sample t-test. The records did not have any identifying information of any patient, and any such data was not retrieved from the hospital records. The data regarding opioid prescription patterns were kept in a password protected file and could only be accessed by study authors for the purpose of data analysis.
RESULTS
The hospital opioid dispensing records were retrieved from January 1, 2020, to May 20, 2020. The opioids that were prescribed and dispensed were tablet morphine (10 mg, 10 mg CR, 30 mg CR, and 60 mg), tablet tramadol 50 mg, and fentanyl patches (25 and 50 mcg). Since the month-wise number of patients' data was not available online for the year 2019, so total yearly dispensing and average monthly opioid quantity dispensed were retrieved. For the year 2020, month-wise dispensing data were available and were utilized for the purpose of analysis [Table 1].
| 2019 | Average monthly data | January 2020 | February 2020 | March 2020 | March 1-23, 2020 | March 24-31, 2020 | April 2020 | May 2020 | |
|---|---|---|---|---|---|---|---|---|---|
| Morphine 10 mg plain (tablets) | 743,302 | 61,942 | 50,906.5 | 39,485 | 46,588 | 39,005 | 7583 | 24,996 | 15,499 |
| Patients | - | - | 682 | 545 | 543 | 489 | 54 | 192 | 126 |
| 10 mg CR (tablets) | 3169 | 264 | 620 | 871 | 611 | 611 | - | 622 | 237 |
| Patients | 15 | 22 | 13 | 13 | - | 6 | 3 | ||
| 30 mg CR (tablets) | 5882 | 490 | 4058 | 4172 | 4295 | 3934 | 361 | 2507 | 1597 |
| Patients | 64 | 67 | 48 | 45 | 3 | 17 | 14 | ||
| 60 mg plain tablets | 56,890 | 4740 | 1695 | 2188 | 3586.5 | 2510 | 1076.5 | 1620 | 737 |
| Patients | - | - | 36 | 32 | 41 | 35 | 6 | 19 | 7 |
| Tramadol 50 mg tablets | 335,130 | 27,927 | 20,599 | 17,995 | 24,472 | 20,624 | 3848 | 15,564 | 10,883 |
| Patients | - | - | 507 | 427 | 448 | 408 | 40 | 177 | 114 |
| Fentanyl 25 mcg patches | 1555 | 1555 | 81 | 57 | 163 | 131 | 32 | 73 | 59 |
| Patients | - | - | 18 | 11 | 21 | 18 | 3 | 8 | 6 |
| 50 mcg patch | 774 | 774 | 205 | 191 | 209 | 179 | 30 | 107 | 191 |
| Patients | - | - | 34 | 27 | 22 | 19 | 3 | 9 | 14 |
| Total number of OPD patients | - | - | 5029 | 3512 | 1420 | 1298 | 122 | 497 | 360 |
OPD: Outpatient department, CR: Controlled release
A total of 743,302 tablets of 10 mg morphine were dispensed in the year 2019, with an average of 61,942 tablets dispensed every month. The same 10 mg tablets were being dispensed at 39,005–50,906 tablets per month before the lockdown period. During this period, the number of patients to which this was dispensed varied from 489 to 682. However, after the lockdown started, the total monthly tablets dispensed reduced (7583–24,996) as well as the number of patients to which it was dispensed. For morphine 10 mg CR tablets, a total number of 3169 tablets were dispensed in the year 2019 with an average monthly consumption of 264 per month. In 2020 before lockdown, a total of 620, 871, and 611 tablets were dispensed during January, February, and March (up to March 23). This number reduced to 622 in April and only 237 in May 2020 (up to May 20), with only 6 and 3 patients being dispensed the same, respectively. Similar reducing trends were observed in morphine 30 mg CR and 60 mg plain tablet dispensing before and during the lockdown [Table 1].
Tramadol tablets and fentanyl patch dispensing quantity
In the year 2019, a total of 335,130 tablets of tramadol were dispensed with an average monthly dispensing of 27,927 tablets. This had continued at a similar level before the lockdown in January (17,995) and February (24,772) to a total of 427 and 448 patients, respectively. However, during the lockdown, this number reduced to a mere 15,664 in April and 10,883 in May to 177 and 114 patients, respectively. Similarly, the amount of both 25 mcg and 50 mcg fentanyl patches reduced during the lockdown. The division of the same is mentioned in Table 1.
Comparison of dispensing before and during lockdown
An independent sample t-test was performed to compare mean dispensing quantity of each strength of the abovementioned opioids before and during lockdown. There was a significant increase in per person average dispensing of morphine 10 mg plain tablets (t = −10.11; P < 0.01) during the lockdown. The increase in average 10 mg CR preparation of morphine during lockdown did not reach statistical significance (P = 0.59). Similarly, all other opioids dispensing per person increased significantly during lockdown (morphine 30 mg CR, t = −4.28, P < 0.01; tramadol 50 mg, t = −12.01, P < 0.01; fentanyl 25 mcg patch, t = −4.46, P < 0.01; and fentanyl 50 mcg patch, t = −2.98, P = 0.04), except morphine 60 mg plain tablets which also increase but could not reach statistical significance (P = 0.11) [Table 2].
| Name of opioid | Mean number of tablets | Independent sample t-test | P | |||||
|---|---|---|---|---|---|---|---|---|
| Average consumption per patient before lockdown (before March 24) | Average consumption per patient during lockdown (after March 24) | |||||||
| Months | ||||||||
| January | February | March | March | April | May | |||
| Morphine 10 mg | 74.64 | 72.44 | 79.76 | 140.42 | 130.18 | 123.01 | −10.11 | <0.01 |
| Mean | 75.61 | 131.2 | ||||||
| Morphine 10 mg CR | 41.33 | 39.59 | 47.00 | - | 103.66 | 79.00 | −0.58 | 0.59 |
| Mean | 42.64 | 60.89 | ||||||
| Morphine 30 mg CR | 63.40 | 62.27 | 87.42 | 120.33 | 147.47 | 114.07 | −4.28 | <0.01 |
| Mean | 71.03 | 127.29 | ||||||
| Morphine 60 mg plain | 47.08 | 68.37 | 71.71 | 179.42 | 85.26 | 105.28 | −2.05 | 0.11 |
| Mean | 62.39 | 123.32 | ||||||
| Fentanyl 25 mcg patch | 4.50 | 5.18 | 7.28 | 10.67 | 9.13 | 9.83 | −4.46 | <0.01 |
| Mean | 5.65 | 9.87 | ||||||
| Fentanyl 50 mcg patch | 6.03 | 7.07 | 9.42 | 10.00 | 11.89 | 13.64 | −2.98 | 0.04 |
| Mean | 7.51 | 11.84 | ||||||
| Tramadol 50 mg | 40.63 | 42.14 | 50.55 | 96.20 | 87.93 | 95.46 | −12.01 | <0.01 |
| Mean | 44.44 | 93.2 | ||||||
CR: Controlled release
Trends in total morphine dispensing
As shown in Figure 1, the total morphine consumption (all strengths) decreased significantly during the lockdown period parallel to the reduced number of patients. However, when per person morphine dispensing was plotted, it was found to have increased during the lockdown period. Thus, there was a trend toward increased per-person consumption of morphine tablets during the lockdown period.
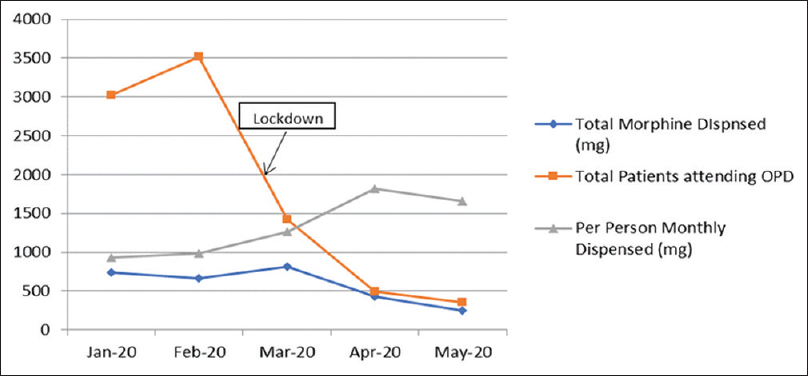
- Trends of morphine dispensing before and during the lockdown
CONCLUSION
Morphine is the drug of choice for the management of cancer-associated severe pain. It is the pillar over which palliative care rests. A huge gap exists between demand and supply in developing countries that account for 80% of the world's total population; yet receive only 6% of the available morphine.[410] Overcoming barriers to palliative care are a major global health agenda that needs immediate attention.[8]
Due to the scare of COVID-19, people with chronic pain and chronic illness are staying at home, practicing social distancing, and wearing masks to protect themselves from the coronavirus. Cancer patients stand to lose at various ends, as they churn between the fear of acquiring a novel virus on the one hand and fighting the (not so novel) menacing malignancy that has already housed their body on the other. Infection with coronavirus can be potentially lethal for them given their frail, emaciated built, poor nutritional status, and immunocompromised state either due to the underlying malignancy itself or due to therapy-induced cytopenia, mucositis, anorexia, or vomiting. Delays in quality and timely cancer care jeopardize their chances of cure by rendering a potentially curable malignancy metastatic and incurable and also adversely affects their quality of life by increasing the symptom burden as the disease load increases. This is often associated with anxiety and fear, fear of living with cancer that is multiplying exponentially with each passing breath, fear of not being able to access health care in general and essential drugs in particular, fear of putting their loved ones at risk of infection if they accompany them to a health-care facility, and fear of living in severe unbearable pain.
A recent publication by the Pain News Network, the International Pain Foundation, and the Chronic Pain Association of Canada mentioned an online survey with 2221 people with chronic pain or chronic illness and the vast majority of respondents from the United States or Canada. One of the biggest worries of respondents is having a health problem and needing to go to a hospital or doctor's office, where they risk exposure to people who may be infected with COVID-19. As a result, over 70% say they have canceled or postponed a medical appointment. About the same number was scared going to hospital and losing access to medications.[11] In this scenario, continuous pain relief for these patients is a huge challenge.
In spite of all the efforts that are being made, finding the ideal approach for care of cancer patients in the middle of the COVID-19 outbreak is a daunting task, presenting itself as a unique clinical challenge.[712] Health-care professionals, administrators, and bureaucrats alike are treading on a tight rope trying to balance adequate infection control with efficient and timely cancer care. As we are writing this study, the number of cancer patients tested positive is increasing, the capacity of some cancer centers is overwhelmed, and new guidelines are being issued by local and national authorities. The approach to handle cancer patients must be dynamic and tailored to every patient's condition, every hospital's resources, and every physician's experience.
Our study presents a unique perspective on this situation, highlighting the opioid dispensing trends during the lockdown period, analyzing the quantum of opioids prescribed and comparative overview to the trend before the lockdown began.
Dedicated and persistent efforts by our team of doctors, supporting staff, and administrators have resulted in a continuous and uninterrupted outpatient service providing patients suffering from pain and other distressing symptoms, adequate and optimum morphine, and other medications. After appropriate precautions and infection control strategies in place, morphine was dispensed in the Pain OPD to follow-up patients as demonstrated in the results. Despite the nationwide lockdown around 1000 patients were seen in the OPD (during the study period) and 447 were prescribed morphine, with a total of 827 grams being dispensed over the span of 2 months. Despite a dramatic decrease in the absolute number of patients visiting the OPD, 497 in April 2020 compared to 3512 in February 2020 the per capita consumption (total morphine dispensed in mg/total number of patients being prescribed) of morphine have increased significantly, 990 mg/person in February 2020 versus 1820 mg/person in April 2020. Considering the mean number of tablets dispensed per person per month, our results show 75.61 tablets of morphine 10 mg plain/month/person in the prelockdown era compared to 131.2 tablets/month/person in the postlockdown period. This could be because of multiple reasons including increased dispensing per person. Due to the COVID related commute crisis, each patient was being prescribed medications for 1 month as opposed to the routine prior practice of a fortnightly prescription, to minimize patients frequent visits to the hospital and at the same time ensure complete coverage of patients analgesic requirement. Another reason could be increased opioid needs during this period, as there were serious delays and interruptions in cancer-directed therapies such as chemotherapy, radiotherapy, and surgery, which were deferred or restricted to minimize the patient load and decrease the total number of patients present in the hospital at any given point of time to reduce the risk of infection, to facilitate social distancing, which led to increase in disease burden corresponding to an increase in pain and other symptoms. This could also be because only those patients are coming to the OPD who are in severe pain and their need of morphine is already high. There is also a prevalent fear and anxiety about how this pandemic will pan out amongst patients. They fear whether they will receive cancer-directed treatment; will they be able to come back again to procure morphine. These psychosocial factors might lead to an increased perception of pain and an increased requirement of morphine and other interventions (such as psycho-education and reassurance) by the palliative care physicians. These results also throw light on the absolute essentiality of morphine in the treatment of severe cancer pain that despite the logistical difficulties, patients are coming to the OPD and procuring morphine in incremental amounts.
Since the number of patients coming to the OPD has reduced drastically, we are assuming only those patients are coming, whose need for pain relief is an emergency, and not met by over-the-counter analgesics, so what about the vast proportion of cancer patients who are not coming to the OPD? A vast majority are not being able to avail any cancer-directed therapy; “are we waiting for another pandemic outbreak?”; only this one could possibly entail a higher quantum of human suffering and pain. It is about time we wake up to this reality and take corrective steps at legislative, policy, and administrative levels to streamline the availability of essential narcotics and palliative care services across the nation.
Limitation of the study was with the inherent nature of the study design that did not take into account individual patient data or any clinical variables such as relief in pain; these trends in dispensing could only at best be a proxy marker for adequate analgesia or symptom control in cancer patients. For the purpose of analysis, the data of preceding 2½ months were taken into consideration, and a larger time frame for comparison would have resulted in better reliability of the data. Parenteral routes of administration of opioids have not been taken into account. Despite the limitations, this is one of the first data discussing opioid dispensing trends in cancer patients during COVID-19-related lockdown. This provides ground for planning a prospective longitudinal analysis of opioid prescription trends for pain relief and guides policy-makers for planning and ensuring a sustainable supply chain of essential narcotics.
CONCLUSION
Opioid forms the mainstay of management for cancer pain, and during the current COVID-19-related lockdown, these patients are the worst hit. Our study was aimed to understand the opioid dispensing trends from a tertiary cancer care hospital. This provides a much-needed impetus toward generating more research and plans innovative solutions for adequate pain relief in cancer patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Strengthening of palliative care as a component of integrated treatment throughout the life course. J Pain Palliat Care Pharmacother. 2014;28:130-4.
- [Google Scholar]
- Redefining palliative care – A new consensus-based definition. J Pain Symptom Manage 2020 pii: S0885-3924(20)30247-5
- [Google Scholar]
- The Indian Society for Study of Pain, Cancer Pain Special Interest Group guidelines on pharmacological management of cancer pain (Part I) Indian J Pain. 2019;33:11.
- [Google Scholar]
- Access to pain relief and essential opioids in the WHO South-East Asia Region: Challenges in implementing drug reforms. WHO South East Asia J Public Health. 2018;7:67-72.
- [Google Scholar]
- Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: The Lancet Commission report. Lancet. 2018;391:1391-454.
- [Google Scholar]
- Cancer care after natural disaster: Different countries, similar problems. J Glob Oncol. 2019;5:1-2.
- [Google Scholar]
- Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335-7.
- [Google Scholar]
- Cancer pain management in developing countries. Indian J Palliat Care. 2016;22:373-7.
- [Google Scholar]
- The Pandemic's Hidden Victims: Sick or Dying, but Not from the Virus. 2020. The New York Times. Available from: https://wwwnytimescom/2020/04/20/health/treatment-delays-coronavirushtml
- [Google Scholar]
- Challenges on the provision of palliative care for patients with cancer in low- and middle-income countries: A systematic review of reviews. BMC Palliat Care. 2020;19:55.
- [Google Scholar]
- 2020. Chronic Pain Patients 'Hanging on by a Thread' During Coronavirus Lockdown Pain News Network. Available from: https://wwwpainnewsnetworkorg/stories/2020/4/21/covid-survey-1
- Cancer patients and research during COVID-19 pandemic: A systematic review of current evidence. Crit Rev Oncol Hematol. 2020;150:102972.
- [Google Scholar]






