Translate this page into:
Ultrasound-Guided Glossopharyngeal Nerve Block at Pharyngeal Wall Level in a Patient with Carcinoma Tongue
Address for correspondence: Dr. Vinod Kumar, Department of Onco-Anaesthesia and Palliative Medicine, Dr. BRA IRCH, AIIMS, New Delhi, India. E-mail: vkchanpadia@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Glossopharyngeal nerve (GPN) block is used for pain management in patients' head and neck malignancy. The GPN is a mixed nerve containing both motor and sensory fibers. The usual approaches for GPN blocks are usually topical, intraoral, or peristyloid. Topical anesthesia may be difficult in patients with limited mouth opening or when there is inflammation in the area of interest. Intraoral and peristyloid approaches have risk of inadvertent neurovascular injection. The intraoral technique may lead to long-lasting oropharyngeal discomfort. Hence, GPN block is done at the pharyngeal wall level for pain relief.
Keywords
Glossopharyngeal nerve
pain
ultrasound
INTRODUCTION
Glossopharyngeal nerve (GPN) block is an interventional technique that has been used for pain management in patients with malignancies of head and neck.[1] The GPN is a mixed nerve containing both motor and sensory fibers. Its motor fibers innervate the stylopharyngeus muscle and sensory portion innervates the posterior third of the tongue, palatine tonsil, and mucous membranes of the mouth and pharynx.[2] Usual approaches for GPN blocks are usually topical, intraoral, or peristyloid. Topical anesthesia may be difficult in patients with limited mouth opening or when there is inflammation in the area of interest, and also, it covers only the mucosa. Intraoral and peristyloid approaches have risk of inadvertent neurovascular injection. The intraoral technique is unpopular in clinical practice and it is associated with long-lasting oropharyngeal discomfort. Peristyloid GPN block may lead to an inadvertent block of adjacent vagus and hypoglossal nerve.[3] We report a case of carcinoma tongue who underwent ultrasound (US)-guided GPN blockade at the pharyngeal wall level.
CASE REPORT
A 65-year-old male was referred to the pain clinic with pain in the left side of the face and oral cavity radiating to left ear and head, which aggravates on deglutition. The patient had moderately differentiated squamous cell carcinoma of the left base of tongue, for which he had chemotherapy and radiation therapy. The patient reported pain score of 10/10 on numeric rating scale (NRS), where 0 represents no pain and 10 is worst imaginable pain. His pain was inadequately controlled on tablet morphine 120 mg/day, tablet paracetamol 3 g/day, tablet etoricoxib 120 mg/day, and tablet gabapentin 1800 mg/day. He had undergone diagnostic and therapeutic per-styloid GPN block by landmark approach 1 month ago, which provides him <25% pain relief for 8–10 days. We decided to perform distal GPN blockade at the pharyngeal wall level, as described by Ažman et al.[4] in their study on cadavers and healthy volunteers.
After obtaining informed consent, the patient was placed supine with their necks extended. US scan was performed using a high-frequency 15–6 MHz, 38-mm linear US transducer (Edge II; SonoSite, Inc., Bothell, Washington). The transducer was initially positioned over the lateral part of the hyoid bone in the transverse plane. The lateral tip of the probe was then rotated cephalad to keep in line with the mandibular angle [Figure 1]. In this position, the pharyngeal wall was identified [Figure 2]. In-plane approach was used, and 2 ml of 2% lignocaine for the diagnostic blockade was given just above the pharyngeal wall using 5 cm 21-G insulated needle (Stimuplex® A - B. Braun Melsungen AG, Germany). The patient reported a pain score of 1/10 on NRS after 30 min of the blockade.

- Position of ultrasound probe
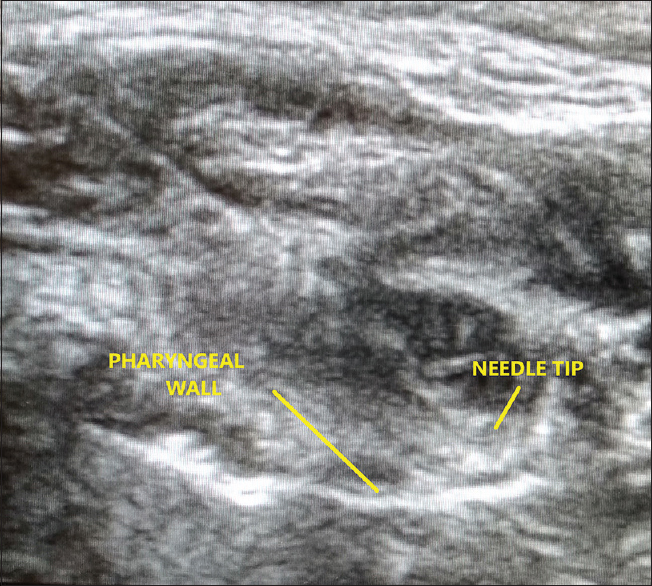
- Ultrasound image showing pharyngeal wall and needle tip
The next day using the same technique, at the same location as the diagnostic block, 1 mL of 2% lignocaine (neon) +2 ml (8 mg) of dexamethasone injected to the target site. No tachycardia, infection, or hematoma developed. No hoarseness and dysphagia developed. After this intervention, the patient scored his pain as 0/10 on NRS. Oral medicines were tapered off over 1 month on a weekly follow-up. The patient's NRS scores stayed at 0/10 after 2 months.
DISCUSSION
The GPN block at the pharyngeal level presented here provides less discomfort for the patients. Real-time US visualization of neurovascular structures makes the procedure safer, especially in patients with altered anatomy (i.e., postradiation therapy, previous surgeries). Bean-Lijewski[3] reported upper airway obstruction after per-styloid GPN blocks for pain control in pediatric tonsillectomies because of unintentional hypoglossal nerve blockade. Unintentional vagus and hypoglossal nerve blockade can cause tachycardia with secondary hypertension. Weakness of the trapezius muscle was also observed as a potential complication of GPN block caused by accessory nerve blockade.
To summarize, US-guided GPN block at the pharyngeal wall level may be an alternative to intraoral or peristyloid approach of GPN blockade. Further studies are needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Atlas of Interventional Pain Management (3rd ed). Philadelphia: Elsevier; 2009. p. :93-6.
- Glossopharyngeal nerve block for pain relief after pediatric tonsillectomy: Retrospective analysis and two cases of life-threatening upper airway obstruction from an interrupted trial. Anesth Analg. 1997;84:1232-8.
- [Google Scholar]
- Ultrasound-guided glossopharyngeal nerve block: A cadaver and a volunteer sonoanatomy study. Reg Anesth Pain Med. 2017;42:252-8.
- [Google Scholar]






