Translate this page into:
Benefit or Harm? A Study on Impact of Collusion on the Quality of Life among Palliative Care Patients
Address for correspondence: Dr. Carolin Elizabeth George, Department of Community Health Family Medicine and Palliative Care, Bangalore Baptist Hospital, Hebbal, Bellary Road, Bengaluru - 560 024, Karnataka, India. E-mail: carolinelizabethj@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
In India, roughly one-half of patients undergoing cancer treatment are unaware of their diagnosis or treatment. The intention of this study is to determine the prevalence of collusion and its influence on quality of life (QOL) among patients in palliative care settings.
Methodology:
A cross-sectional study was conducted among 100 palliative care patients to assess the extent of knowledge about their diagnosis and prognosis. The caretakers and the treating doctors were interviewed using a semi-structured questionnaire to assess if diagnosis was revealed to a patient. QOL of the patients was assessed using the European Organisation for Research and Treatment of Cancer QOL Questionnaire-C30 questionnaire.
Results:
The prevalence of collusion was 37%, i.e., in more than one-third of the palliative care patients; caregivers restrained doctors from disclosing the diagnosis. The prevalence of collusion was less among patients with higher educational qualification (P = 0.027) and professionals (P = 0.025). Collusion was not associated with gender, type of family, place of residence, and socioeconomic status (SES). In multivariate regression, collusion (odds ratio = 10.53) was independently associated with poor QOL when adjusted for age, gender, place of residence, religion, educational status, family type, and SES.
Conclusion:
Collusion is fairly prevalent and it worsens the QOL among cancer patients. Since the main driver for collusion is the strong desire among caregivers to protect the physical and psychological well-being, the findings of the study could motivate the caregiver for a more open and honest communication.
Keywords
Collusion
communication
palliative care
INTRODUCTION
The term collusion is defined as a secret agreement or cooperation between two or more people who are trying to deceive.[1] In healthcare, collusion implies any information about the diagnosis, prognosis, and medical details about a person who is ill-being withheld or not shared among individuals involved.[2]
In India, roughly one-half of patients undergoing cancer treatment are unaware of their diagnosis or treatment.[34] Many a time, the treating doctor finds it easier to reveal the diagnosis and prognosis to the family rather than to the patient. Being driven by affection for the patient and fear of distressing him or her, family members refrain from revealing the truth to the patient. Further, the family also requests the treating doctor not to disclose the facts to the patient.[2]
Collusion can have many disadvantages. It can lead to poor doctor–patient relationship, poor symptom control, and suspicion and mistrust leading to sour relationship with close relatives.[25]
On the other hand, an honest, open, and compassionate communication with the patient and the relatives may often be beneficial to both. Although the short-term effects may include emotional outbursts, despair, guilt, and depression, it is often more beneficial in the long term, offering an opportunity for the patient to discuss any unfinished business, future plans, and acceptance which may improve the overall quality of life (QOL) and death.[2]
Although physicians would prefer to reveal the diagnosis to the patient, they succumb to extreme pressure from the relatives.[2] The physician also finds it hard to decide whether collusion is better for the patient or not. Although family members collude with doctors with the intention of preventing deterioration of the overall quality of daily life of the patient (involving his/her emotional, physical, environmental, and social factors), the actual influence it has on the patient's QOL has not been explored in the Indian context.
The intention of this study is to determine how widespread collusion is in palliative care settings and its influence on the QOL of cancer patients in South India.
METHODOLOGY
A hospital-based cross-sectional study was conducted among 100 cancer patients under the palliative care program at Bangalore Baptist Hospital. The hospital runs home-based palliative care program in both rural and urban area. The study was conducted from March 2013 to May 2014. Patients who were >18 years old of both gender and who were under palliative care for at least 2 months were invited to participate in the study. A minimum period of 2 months was considered for better discernment of the effect of collusion. Patients with impaired comprehension and those with psychiatric illness were excluded. The sample size was calculated as 100 assuming 50%[34] as prevalence of collusion at 95% confidence interval with 10% precision. Convenience sampling was done and patients were recruited 3 days/week on average, until the target sample size was attained. The study was approved by the Institutional Ethics Committee of Bangalore Baptist Hospital. The study was registered in Clinical Trial Registry of India (REF/2015/02/008470).
Tool
Patients were interviewed with a semi-structured questionnaire to assess the extent of knowledge about the diagnosis and prognosis. The caretakers were interviewed to assess if diagnosis was known to them and whether it was revealed to the patient. Collusion was considered if the relatives had asked the health-care provider to hide the diagnosis when the patient wants to know.
The duration since the diagnosis of cancer, stage of cancer, and details of treatment were obtained from the history or hospital records.
The questionnaire consisted of two parts. The first part comprised patient demographics (name, age, sex, place, education, and occupation) along with questions exploring existent collusion and the second part comprised questions assessing the QOL, adopted from the European Organisation for Research and Treatment of Cancer QOL Questionnaire-C30 (EORTC QLQ-C30) questionnaire version 3.[6]
The EORTC QLQ-C30 is one of the most widely used health-related QOL questionnaires in oncology, for palliative care research, and is validated in all South Indian languages. The tool comprises five functional scales, three symptom scales, a global health status/QOL, and six single items. Validated Kannada and Hindi version were obtained from the official website with necessary permissions.
Three questions were added from the Functional Assessment of Chronic Illness Therapy-Palliative Care Subscale (FACIT-PAL version 4)[7] and QOL questionnaire for cancer patients as it was relevant to the context of collusion. The statements were as follows:
-
Am I able to openly discuss my concerns with the people closest to me?
-
Was the doctor cooperative and given you all information you need?
-
Does your personal faith and religious belief give you strength to face difficulties?
Scoring of the questionnaire
For the first 28 questions, four responses (1 = not at all to 4 = very much) were possible depending on the severity of the problem as felt by the patient. Two questions regarding overall health status and QOL had a range of values from 1 to 7, with 1 indicating worst and 7 indicating excellent. Based on the responses marked, scores were calculated for overall health/QOL, functional scales covering – physical, emotional, role, social, cognitive aspects – and symptom scale as per the formula given below.
-
First, the raw score (RS) was calculated
-
RS= (I1 + I2 + I3+……In)/n
-
R = range (difference between possible maximum and minimum response to individual item)
-
For functional scales, S (score) = (1− [RS − 1]/range) × 100
-
For symptom scales/items and global health status/QOL, S = ([S − 1/range]) × 100.
The overall scores were calculated without any deviation from the original scale.
A high score for a functional scale represents a high/healthy level of functioning, a high score for the global health status/QOL represents a high QOL, but a high score for a symptom scale/item represents a high level of symptomatology/problems.
From FACIT-PAL (version 4)[7] and QOL questionnaire for cancer patients, the questions were marked from 1 = not at all to 4 = very much as patient experienced. FACIT items were asked separately and just expressed as percentages. It was not used in any calculations.
Statistical methods
Descriptive and inferential statistical analysis was carried out. The prevalence of collusion was calculated in percentages. Univariate analysis was carried out to assess the association between age, gender, place of residence, educational status, and socioeconomic status (SES) with collusion. Student's t-test (two-tailed, independent) was to find the significance of study parameters on continuous scale (age) between collusion and noncollusion group (intergroup analysis). Chi-square/Fisher's exact test was used for categorical data.
The QOL is expressed as mean ± standard deviation (min–max).
Multiple linear regression was used to characterize the relationship between the QOL and independent variables (collusion, age, gender, educational status, and SES) and to adjust for confounders. R2 was used to check the goodness of fit. Significance of the model was assessed by ANOVA. A P < 0.05 was considered statistically significant. The statistical software Statistical Package for Social Sciences (SPSS for Windows, Version 16.0. Chicago, SPSS Inc.) was used for the analysis.
RESULTS
The baseline characteristics of the population studied are summarized in Table 1. The prevalence of collusion was 37%, i.e., in more than one-third of cases; the relatives had asked the health-care provider to hide the diagnosis when the patient wanted to know.

The prevalence of collusion was lower among people with high educational qualification (P = 0.027). Occupation was classified as agriculture, professionals (engineers, teachers, information technology professionals, managers, etc.), no occupation, and others (shopkeepers, carpenters, painters, tailors, clerks, etc.). All people who belonged to professional group had no collusion which was statistically significant (P = 0.025). Collusion was not associated with gender, type of family, place of residence, and SES [Table 2].

Collusion was significantly associated with poorer QOL (mean global QOL 38.28 ± 24.3 vs. 50.52 ± 23.08, P = 0.014). Pain and fatigue scores were worse among patients when there was collusion [Table 3].
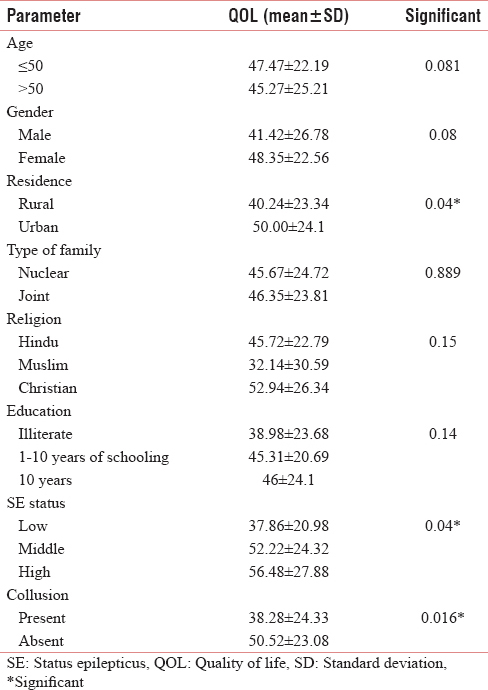
In multivariate regression, collusion (odds ratio [OR] =10.53) was independently associated with QOL when adjusted for age, gender, place of residence, religion, educational status, family type, and SES [Table 4].
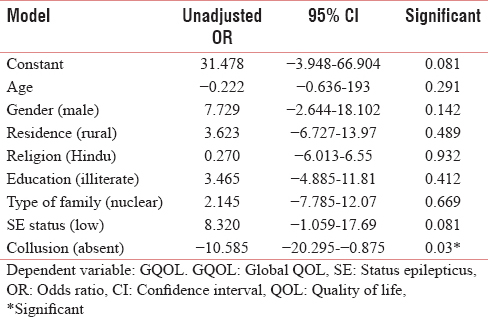
Physical functioning (OR = 16.8) and cognitive functioning (OR = 14.3) domains were significantly lower in patients with collusion, whereas collusion had no effect on role functioning, emotional, and social functioning domain [Table 5].

Those under collusion had significantly less satisfaction with the information provided by the doctor (2.9 ± 1.01 vs. 3.6 ± 0.78, P = 0.000). Both groups equally found it difficult to discuss their concerns with family members (P = 0.823).
DISCUSSION
Assessing collusion was a complex phenomenon which included chart review and multiple interviews with the health provider, patients, and relatives. This was possible because we have a home-based palliative care program, the health providers knew the families very well and collusion was assessed and reported in the chart as a part of routine assessment.
There are only a handful of studies in India that have explored the prevalence of collusion. A study from Kerala in 2003 reported 38%[8] collusion and another in 2008 reported 55%.[9] Other countries[101112] reported a prevalence ranging from 40%. Regardless the region, almost all studies reported that at least one-third of the patients were not aware that they had cancer. In our study, collusion was considered if the relatives had asked the health-care provider to hide the diagnosis when the patient wanted to know. In most of the studies, there were no discretion between nondisclosure and collusion.
In our study, it was also noticed that most of the people who knew their diagnosis were kept in the dark regarding the prognosis. Literature also points out that there are many layers and faces of collusion. The physician may disclose the diagnosis but withhold information about prognosis and may not reveal the transition from curative to palliative care, and the topic of death and dying is not discussed however close it might be.[2]
The most common reasons for collusion in western societies is the physician's lack of confidence in their own communication skills in dealing with sensitive patient issues and the need to sustain hope. A qualitative study from the Netherlands reported that patients also contributed to collusion by focusing exclusively on recovery in their communication with doctors which posed a considerable barrier for straightforward communication.[13] However, in nonwestern societies such as in India, the most common reason for collusion is the caregiver's urge to protect their loved one from psychological trauma and stigma.[2]
In a study conducted in India, most cancer patients wanted to know about their disease condition.[14] Contrary to common belief,[15] <2% of 988 terminally ill patients interviewed saidthat talking about death causes distress. Evidence suggests that most elderly people wish to be informed and do not experience any more psychological distress than the younger patients.[16]
In the recent study conducted in South India, 95% patients said that they preferred to know about their disease condition and prognosis.[17] Majority of the patients prefer to be informed of the diagnosis by their physicians and patients’ preference were similar all over the world from middle and far East to America and Europe.[18] A survey in Nepal showed that 80% of the respondents wanted to be informed if they were diagnosed with cancer.[19] Arguments that cancer patients from Asian cultures have different preferences regarding being informed of their cancer diagnosis and that family members have legitimate superior power in decision-making could not be supported from studies compiling data from these countries. Usually, patients are quite aware of the severity of the disease and many often prefer honest communication.[20] Evidence suggests that sensible disclosure of diagnosis and prognosis is important and is associated with a better QOL.[21]
Women are considered weaker compared to men in Indian culture, and hence, collusion is expected more when the patient is a woman. In a study conducted by Muckaden et al.,[22] more than two-thirds of the women who had cervical cancer were kept in the dark regarding their diagnosis by their spouses. Compared to experience in western culture, which is more individualistic, collectivism in Indian culture promotes hiding of the facts to promote psychological well-being.[23] However, in this study, collusion was equally prevalent in both genders.
In this study, collusion was significantly lower among professionals and those with higher educational status. They are perceived as less emotionally vulnerable which may be reason for honest disclosure. Furthermore, individuals with higher education more actively seek information than an illiterate person. Although it is perceived that people with low educational status and those belonging to low SES do not want to know about their disease, a study in North India found out that the majority of the illiterate and patients belonging to low socioeconomic class opined that they needed to know about their disease.[15]
Collusion was independently associated with QOL, when adjusted for age, sex, place of residence, family type, educational status, and SES. We have used modified Kuppuswamy scale for assessing SES. Since educational qualification and professional status are predictors of SES, one would expect SES to be significant as well. However, it was different in our case. Reasons for this discrepancy may be due to following factors:
-
Occupation and education are easy to assess, however getting the correct family income is a challenge. Final SES calculation can go wrong because of this
-
Though not significant, collusion was more prevalent among low socioeconomic class as compared to others. Small numbers of high SES and convenience sampling can be the reasons for it.
Physical and cognitive functioning significantly decreased in patients with collusion. Patients with collusion also expressed extreme dissatisfaction in their communication with doctors.
To our best of our knowledge, there are no Indian studies that have explored the effect of collusion on QOL among cancer patients.
An Italian study[20] done on 175 cancer patients reported that QOL improved if the patients were satisfied with level of information received during counseling. Another study conducted in Turkey among 100 cancer patients reported that the honest disclosure of the truth about diagnosis or prognosis did not worsen any dimension of QOL in general or emotional functioning in particular.[18] The present study showed that honest disclosure improves the cognitive functioning, physical functioning, and overall QOL by 10 times.
CONCLUSION AND RECOMMENDATIONS
Collusion is fairly widespread among cancer patients in Karnataka. Collusion was less prevalent among professionals and those with higher educational status.
Collusion worsens the QOL and quality of death among cancer patients. Physicians should discuss the problems associated with collusion to the patient's family members and alleviate their anxiety. Since the main driver for collusion in our culture is the strong desire among caregivers to protect the physical and psychological well-being of their loved one, the findings of the study could motivate the caregiver for a more open and honest communication.
Adequate training on breaking bad news may help health professionals promote an enabling environment for the patient. An empathetic honest communication in culturally and ethically acceptable ways would be the best option in ensuring a good QOL and death among cancer patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge the support provided by Dr. Amy, Sr. Anu, Sr. Sabitha and Sr. Honey in the conduct of the study.
REFERENCES
- The Oxford Dictionary of Philosophy (2nd ed). New York: Oxford Press; 1990. p. :251.
- Communication with relatives and collusion in palliative care: A cross-cultural perspective. Indian J Palliat Care. 2009;15:2-9.
- [Google Scholar]
- Awareness of diagnosis and psychiatric morbidity among cancer patients – A study from South India. J Psychosom Res. 1998;45:257-61.
- [Google Scholar]
- Sexual issues in cancer. In: Chandra PS, Chaturvedi SK, eds. Psycho Oncology: Current Issues. Bangalore: NIMHANS; 1998. p. :79-90.
- [Google Scholar]
- Communication Skills in Palliative Care. New Delhi: Voluntary Health Association of India; 2008.
- The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365-76.
- [Google Scholar]
- 2007. FACIT-Pal (Version 4) Physical Well-Being Social/Family. Available from: http://www.facit.org/LiteratureRetrieve.aspx?ID=42310
- Are oncology patients aware of their diagnosis? A survey from Calicut. Indian J Palliat Care. 2004;10:39.
- [Google Scholar]
- Palliative care in advanced gynecological cancers: Institute of palliative medicine experience. Indian J Palliat Care. 2008;14:86.
- [Google Scholar]
- Reducing collusion between family members and clinicians of patients referred to the palliative care team. Perm J. 2009;13:11-5.
- [Google Scholar]
- Questioning diagnosis disclosure in terminal cancer patients: A prospective study evaluating patients’ responses. Palliat Med. 1994;8:39-44.
- [Google Scholar]
- Does awareness of diagnosis make any difference to quality of life. Determinants of emotional functioning in a group of cancer patients in Turkey? Support Care Cancer. 2002;10:51-7.
- [Google Scholar]
- Collusion in doctor-patient communication about imminent death: An ethnographic study. BMJ. 2000;321:1376-81.
- [Google Scholar]
- Talking with terminally ill patients and their caregivers about death, dying, and bereavement: Is it stressful? Is it helpful? Arch Intern Med. 2004;164:1999-2004.
- [Google Scholar]
- Diagnosis and prognosis disclosure among cancer patients. Results from an Italian mortality follow-back survey. Ann Oncol. 2006;17:853-9.
- [Google Scholar]
- Awareness of diagnosis among cancer patients and its outcome. J Evid Based Med. 2017;4:1108-13.
- [Google Scholar]
- Informing patients about cancer in Nepal: What do people prefer? Palliat Med. 2006;20:471-6.
- [Google Scholar]
- Anxiety and depression in patients with gastrointestinal cancer: Does knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007;7:28.
- [Google Scholar]
- Psychosocial issues faced by women with incurable cervical cancer in India-how can we help? Indian J Palliat Care. 2005;11:94.
- [Google Scholar]
- Individualism and Collectivism. San Francisco, CA: Westview Press; 1995. p. :259.






