Translate this page into:
Hospital Workers' Confidence for End-of-Life Decisions in their Family: A Multicenter Study
Address for correspondence: Prof. Joseph Varon, 2219, Dorrington Street, Houston, TX 77030, USA. E-mail: joseph.varon@uth.tmc.edu
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
To study whether health-care workers feel capable of making resuscitation decisions for their own families, the confidence in their family to represent their own preferences, and if some health-care workers feel greater confidence in their ability to undertake such decisions for their family than others.
Methods:
An anonymous survey conducted among health-care workers of nine institutions in North and Central America. The self-administered questionnaire included demographic and professional characteristics, attitudes, personal preferences, and value judgments on the topic of resuscitation.
Results:
Eight hundred and fifty-eight surveys were completed; 21.1% by physicians, 37.2% by nurses, and 41.7% by other health-care. Most of the health-care workers (83.5%) stated that they should be unable to determine their own code status and they would allow their family or spouse/significant other to make this decision for themselves. Physicians felt significantly more capable of making a decision regarding the code status of a close family member than other hospital workers (P = 0.019). Professionals who chose to not undergo cardiopulmonary resuscitation were less likely to feel capable of determining the code status of their family.
Conclusions:
Most of the health-care workers feel capable of making code status decisions for a close family member and most feel equally comfortable having their family or spouse/significant other represent their code status preference should they be incapacitated. There is considerable reciprocity between the two situations. Physicians feel more confident in their ability to make code status decisions for their loved ones than other health-care workers. Regardless of profession, a personal preference for do not attempt resuscitation status is related to less confidence.
Keywords
Decision-making
end-of-life preferences
health-care workers
surrogates
INTRODUCTION
When a person is incapable of making decisions regarding their own medical treatment, the order for decision will start with a health-care proxy, which is a written document or/and advance directive with an agent designated by the patient to carry out wishes; a living will with specific patient's wishes or a close family member which is often nominated as surrogate decision-maker unless otherwise specified by law.[1]
Regardless of their personal preferences, surrogates are expected to accurately reflect the preferences of the incapacitated patient. However, substitute judgment may not be achieved in situations where prior communication between the patient and their surrogate did not include patient preferences and when conflict arises between the two.[23] Cardiopulmonary resuscitation (CPR) constitutes the extreme example of both when sudden cardiac arrest usually does not preclude prior discussion of patient preferences, and there has been no preparation for loss.[4]
Potential surrogates from the general population usually reflect the value judgments of their loved ones regarding end-of-life treatment.[567] The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) and hospitalized elderly longitudinal project (HELP) studies demonstrated that family members implicitly believe they share similar value judgments; the data demonstrated that patients prefer to leave resuscitation decisions to their family.[89] Shif et al. also showed that surrogates feel comfortable in their ability to act as decision-makers.[10]
Health-care workers' attitudes toward end-of-life decisions often differ from those of the general public.[1112] By virtue of being both accessible and present on location, they often act as objective consultants for families seeking advice regarding provision of life-sustaining measures and resuscitation.[1314] Their impartiality, knowledge, and experience regarding potential outcomes make them highly trustworthy as consults from the perspective of the surrogate seeking to make an informed decision.[1516] However, these characteristics may lead to creation of a divide between the personal value judgments of a health-care worker and those of their family. Such differences would manifest when the health-care worker be required to act as surrogate or should they be required to nominate a family member as a potential surrogate for themselves.
In this multicenter survey, we studied whether health-care workers feel capable of making resuscitation decisions for their own families, the confidence in their family to represent their own preferences, and whether some health-care workers feel greater confidence in their ability to make resuscitation decisions for their loved ones than others.
METHODS
Following Institutional Review Board approval/waiver in accordance with local demands, a questionnaire-based survey was conducted in three countries among a convenience sample of health-care workers. The questionnaire lacked personal identifiers to ensure respondent confidentiality, and informed consent was implied by questionnaire completion.
Study population
All health-care workers in nine medical centers were approached with a request to complete a questionnaire on the topic of attitudes toward ethical medical issues, including CPR. In all centers, the hospital leadership first indicated their approval. Lists of employees were generated for the purpose of approaching a broad sample as possible since the study was intended to encompass all the health-care workers in each center rather than focusing solely on doctors and nurses. After applying the survey in each medical center, these lists were destroyed.
Survey tool
The questionnaire included questions regarding respondent demographics and training as well as personal preferences and opinions regarding CPR. The final version of the questionnaire was generated by a multidisciplinary group of intensive care physicians, nurses, palliative care specialist, hospital religious staff, and medical students. The accuracy and clarity of the questions was validated by intensive care physicians in two countries, and a Spanish version (validated through translation and back-translation) was prepared for application in the participant Hispanic countries.
Survey application
From March 2015 to April 2015, the staff of nine health-care institutions in North and Central America was surveyed. In North America, participants were from medical centers located in Houston and Corpus Christi. In Central America, responses were generated from the staff of medical centers located in Mexico (Puebla and Tijuana) and Panama (Panama City).
The survey was conducted using paper questionnaires that were handed out to the health-care staff by medical students. All the students distributing the survey underwent prior training together in survey techniques and were instructed that the survey was to be self-administered. During distribution, participants were instructed to select only one response per query. Surveys were completed on location and were collected by the same student shortly after distribution. There was no follow-up on nonresponders.
Outcome measures
The primary outcome measures were the responses to two questions: “Do you feel capable of making a decision regarding code status in a close family member?” and “Would you allow your family decide your code status if you were not able to?” Secondary outcome measures were the correlation of these responses with respondent characteristics.
Data management and statistical analysis
A code number was assigned to each questionnaire to ensure systematic data entry. The questionnaires from all the medical centers were collected. All data were entered to a designated SPSS (IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corporation, NY, USA) database. All completed questionnaires were included in data analysis.
Statistical analyses were performed using SPSS Statistics (IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corporation, NY, USA). In the first step, descriptive statistics were used to study the survey population. In the second step, Chi-square test was used to study the associations between the main outcome measures and profession and between the two main outcome measures themselves. Finally, logistic regression analysis was used to study the characteristics of the health-care provider that does not feel capable of making end-of-life decisions for their family members. First, a univariable analysis was performed to study the association of individual variables with this outcome measure. Then multivariable analysis was performed using all the variables that had been significant (P < 0.05) in univariable testing. In the descriptive statistics, the proportions were calculated from the population in its entirety. In the multivariate logistic regression, cases without data on the included variables were excluded from the analysis. The results of both analyses were tabulated.
RESULTS
Questionnaires were completed by 858 health-care workers. Among the respondents, 37.3% (n = 320) were males and 62.7% (n = 538) were females. Physicians accounted for 21.1% (n = 180), nurses 37.2% (n = 317), and other hospital workers 41.7% (n = 356). Among the physicians (n = 180), the largest number of respondents was from internal medicine (n = 42), emergency medicine (n = 26), general practitioners (n = 25), and anesthesiologists (n = 8). Almost half (47.3%, n = 150) of nurse respondents were either currently working or had previous experience working in an intensive care unit. One-third of the respondents (32.6%, n = 280) had <5 years of experience in the medical field.
Response to the main study questions
Responses were provided to the main study questions in 99.4% (852/858) of the surveys. Most health-care workers (88.3%, n = 758) felt capable of making code decisions for a close family member. Most of the health-care workers also stated that they would feel comfortable having their family (83.8%, n = 719) or spouse/significant other (81.2%, n = 697) determine their personal code status if they were unable to do so themselves.
Physicians, nurses, and other health-care workers felt similarly comfortable letting their family (P = 0.224) or spouse/significant other (P = 0.413) determine their own code status. However, physicians felt significantly more capable of making such decisions for their family than did nurses and other hospital workers (P = 0.019) [Figure 1].

- Decision-making for family members
Regardless of profession, there was a significant association between a health-care workers' feeling capable of making a decision for their close family member, and their willingness to trust their family/spouse/significant other to make a decision regarding their personal code status (P < 0.001).
Who does not feel capable making resuscitation decisions for their family?
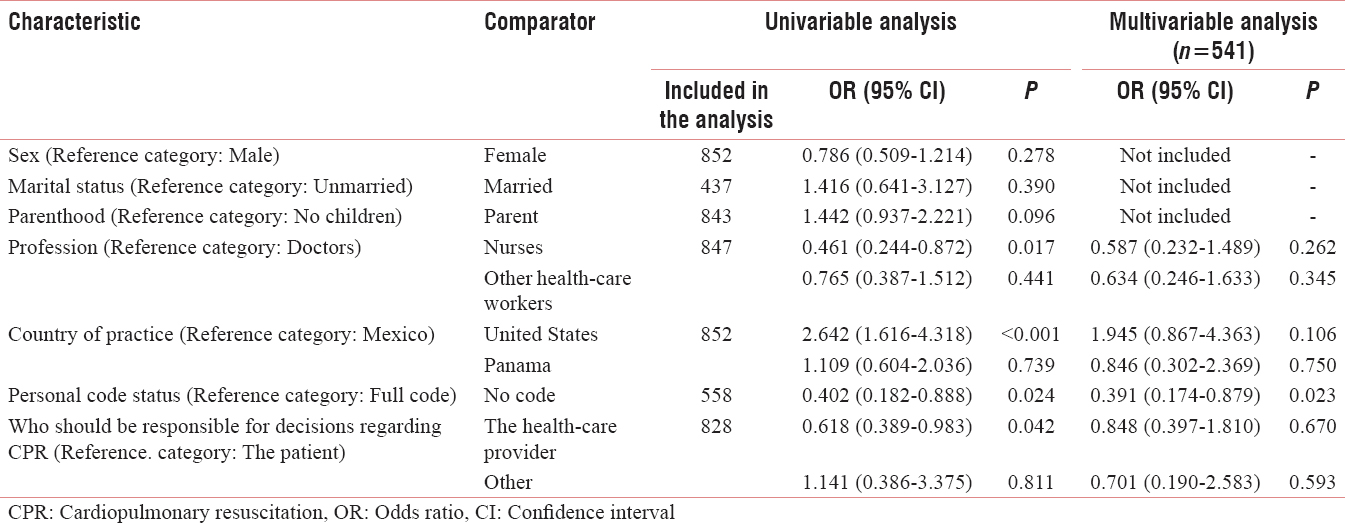
Several variables were found to be significant in the univariable analysis. Nurses were twice more likely to feel incapable of making this decision than doctors or other health-care workers. Health-care professionals practicing in the United States were almost three times more likely to feel incapable than their colleagues in Mexico or Panama. Health-care professionals that would prefer “No code” for themselves were only half as confident in their ability to make decisions for their family than their colleagues who would like to undergo a full code. Finally, health-care professionals who generally believe that the health-care provider should be responsible for decisions regarding CPR were only half as confident in their own capacity to act as surrogate for their family than their colleagues who believe the patient should be responsible for this decision.
In the multivariable analysis, only one variable remained strongly significant: those professionals who would prefer to not undergo CPR themselves were significantly less likely to feel capable of acting as surrogates for their family regarding resuscitation decisions [Table 1].
DISCUSSION
Most of the health-care workers surveyed in the current study felt capable of determining the code status of a close family member and most felt comfortable having their family or spouse/significant other determine their own resuscitation status should they be incapacitated. A greater proportion of physicians felt capable of making such decisions for their family than did nurses and other hospital workers. Regardless of profession, trusting that family or spouse/significant other can represent the health-care professional's resuscitation preferences, was closely associated with confidence in being able to make similar decisions for their own family (i.e., reciprocity). However, the most remarkable finding was that the characteristic most strongly associated with health-care workers' lack of confidence regarding their ability to represent their family was their preference for “do not attempt resuscitation” (DNAR) status for themselves.
Quite a few studies have addressed the ability of family members to act as surrogates for end-of-life decision-making[271017] and the ability of health-care workers to assist surrogates to make such decisions.[18] However, to the best of our knowledge, no study has examined health-care workers as family members themselves. The current study also explores the association between making decisions for your family and trusting they can make decisions for you, i.e. reciprocity in end-of-life decision-making. Most other studies ascribe only one role to their study participants – either surrogate or patient.[910] We included participants from several centers across three countries, which lend the results of this study greater cross-cultural validity than studies conducted in one center or one country.[91017] Culture is strongly associated with end-of-life preferences and attitudes toward patient autonomy.[192021] The two populations included in this study (United States and Latin America) differ on these matters; Hispanics tend toward greater involvement of family in end-of-life decisions but are also less inclined to discuss end-of-life preferences with the family.[1921] Both of these characteristics may affect surrogate accuracy.[217]
Similar differences have been identified among Western and non-Western cultures. End-of-life decisions in non-Western population tend toward a more family collective decision-making or even a patriarch-centered decision, as compared to the patient individual autonomy seek in Western cultures. Non-Western cultures may delay end-of-life care planning based on a sense of inappropriateness or fear toward this subject.[2223]
The proportion of respondents stating that they are confident in their ability to determine the code status of a family member, regardless of their training, was much higher among the health-care workers we surveyed than the proportion of confident responses found among people from the general public that were asked this question at the time their loved one was critically ill. Shif et al. described a 68% rate of positive responses among surrogates of critically ill patients (n = 50).[10] Majesko et al. found a 72.6% rate of confident responders (n = 223).[17] Hospital workers are more familiar with resuscitation terminology and usually have a better understanding regarding the possible outcomes of CPR, both of which may instill a sense of confidence. Laypersons may have misguided perceptions of resuscitation and its possible outcomes.[101424] Some may also balk at terms such as “do not resuscitate” if they mistakenly believe this means ceasing all life support measures.[1025] Our study sample consisted of hospital staff who is most highly educated and yet physicians were significantly more confident than other health-care workers in their ability to make code status decisions for their family. A higher level of education has been associated with increased surrogate accuracy.[4] Furthermore, constant professional exposure to the end of life provides ample opportunity to raise this topic during family gatherings, potentially giving platform to opinions that would otherwise never have been voiced.
More than four-fifths (83.8%) of our respondents were confident in their family are capable of representing their code status preferences. Kim and Kjervik conducted a secondary analysis of the SUPPORT II data; from the 4804 inpatients of the mean data set, they included 362 seriously ill patients with documented clear preferences about resuscitation. They reported an almost similar rate of patient reliance on family and physician's surrogates (77%).[9] Puchalski et al. also analyzed data from two studies in elderly (HELP) and seriously ill patients (SUPPORT) and found that 70.8% of the former patients and 78% of the latter would prefer their family wishes to be followed rather than their own.[8]
Our study also found that most health-care workers with DNAR preferences did not felt capable of deciding for their families. In most developed countries, resuscitation is culturally accepted as the default procedure in case of death. A DNAR choice only perceived as reasonable when ongoing care seems futile. However, health-care workers often adopt a more cynical view toward resuscitation. In fact, a recent study conducted in California showed that 88.3% of surveyed doctors chose DNAR status for themselves.[12] The conflict between culturally acceptable value judgments and their personal value judgments is embodied not only in the feeling that they are incapable of representing the preferences of others but also in that others cannot represent them. This could be a real cause of concern for themselves and their families since families naturally defer to the health-care worker in the family to lead most medical decisions.
Our study has several limitations. We used a convenience sample, and questionnaire completion was entirely voluntary. This may have biased our results. Although our sample population was relatively multicultural, our results may not be applicable to other regions of the world. Because we wanted to study health-care workers, a hypothetical scenario was created. Ideally, confidence in decision-making should have been studied in actual surrogates similarly to the general population.[1026] We did not ask the respondents whether they have had prior experience with decision-making as a surrogate for a family member; family members with no prior experience as surrogates will struggle more with this role.[17]
CONCLUSION
Most of the health-care workers feel capable of making code status decisions for a close family member and most feel comfortable having their family or spouse/significant other make their code status decisions should they themselves be incapacitated. There is considerable reciprocity between being confident in making a decision for others and being confident that others can make a similar decision for oneself. Physicians feel more confident in their ability to make code status decisions for their loved ones than other health-care workers. Regardless of profession, a personal preference for DNAR status is related to a decrease in confidence. Further research should be conducted regarding the reasons; some health-care workers opt for a DNAR status while others do not, and how this relates to their interactions with their families and their patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Myth of substituted judgment. Surrogate decision making regarding life support is unreliable. Arch Intern Med. 1994;154:90-6.
- [Google Scholar]
- Physicians' and spouses' predictions of elderly patients' resuscitation preferences. J Gerontol. 1988;43:M115-21.
- [Google Scholar]
- Knowing loved ones' end-of-life health care wishes: Attachment security predicts caregivers' accuracy. Health Psychol. 2011;30:814-8.
- [Google Scholar]
- The accuracy of substituted judgments in patients with terminal diagnoses. Ann Intern Med. 1998;128:621-9.
- [Google Scholar]
- The accuracy of surrogate decision makers: A systematic review. Arch Intern Med. 2006;166:493-7.
- [Google Scholar]
- Spouses' effectiveness as end-of-life health care surrogates: Accuracy, uncertainty, and errors of overtreatment or undertreatment. Gerontologist. 2008;48:811-9.
- [Google Scholar]
- Patients who want their family and physician to make resuscitation decisions for them: Observations from SUPPORT and HELP. Study to understand prognoses and preferences for outcomes and risks of treatment. Hospitalized Elderly Longitudinal Project. J Am Geriatr Soc. 2000;48(5 Suppl):S84-90.
- [Google Scholar]
- Deferred decision making: Patients' reliance on family and physicians for CPR decisions in critical care. Nurs Ethics. 2005;12:493-506.
- [Google Scholar]
- What CPR means to surrogate decision makers of ICU patients. Resuscitation. 2015;90:73-8.
- [Google Scholar]
- Respiratory support withdrawal in Intensive Care Units: Families, physicians and nurses views on two hypothetical clinical scenarios. Crit Care. 2010;14:R235.
- [Google Scholar]
- Do unto others: Doctors' personal end-of-life resuscitation preferences and their attitudes toward advance directives. PLoS One. 2014;9:e98246.
- [Google Scholar]
- Withholding and withdrawing life-sustaining treatment. Am Fam Physician. 2000;62:1555-60, 1562, 1564.
- [Google Scholar]
- Understanding cardiopulmonary resuscitation decision making: Perspectives of seriously ill hospitalized patients and family members. Chest. 2006;130:419-28.
- [Google Scholar]
- Physician-related barriers to communication and patient- and family-centred decision-making towards the end of life in intensive care: A systematic review. Crit Care. 2014;18:604.
- [Google Scholar]
- Family communication and decision making at the end of life: A literature review. Palliat Support Care. 2015;13:815-25.
- [Google Scholar]
- Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40:2281-6.
- [Google Scholar]
- Decisions about life-sustaining treatment. Impact of physicians' behaviors on the family. Arch Intern Med. 1995;155:633-8.
- [Google Scholar]
- Barriers to optimum end-of-life care for minority patients. J Am Geriatr Soc. 2002;50:182-90.
- [Google Scholar]
- Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634-41.
- [Google Scholar]
- Communication with relatives and collusion in palliative care: A cross-cultural perspective. Indian J Palliat Care. 2009;15:2-9.
- [Google Scholar]
- End-of-life care in the Indian context: The need for cultural sensitivity. Indian J Palliat Care. 2007;13:59-64.
- [Google Scholar]
- Cardiopulmonary resuscitation: Knowledge and opinions among the U.S. general public. State of the science-fiction. Resuscitation. 2008;79:490-8.
- [Google Scholar]
- Empowering family members in end-of-life care decision making in the Intensive Care Unit. Dimens Crit Care Nurs. 2009;28:18-23.
- [Google Scholar]
- Beyond substituted judgment: How surrogates navigate end-of-life decision-making. J Am Geriatr Soc. 2006;54:1688-93.
- [Google Scholar]






