Translate this page into:
Effects of a Yoga Program on Mood States, Quality of Life, and Toxicity in Breast Cancer Patients Receiving Conventional Treatment: A Randomized Controlled Trial
Address for correspondence: Dr. Nagarathna Raghuram, Department of Life Sciences, Swami Vivekananda Yoga Anusandhana Samsthana, No. 19, Eknath Bhavan, Gavipuram Circle, K.G Nagar, Bengaluru - 560 019, Karnataka, India. E-mail: rnagaratna@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
The aim of this study is to compare the effects of yoga program with supportive therapy counseling on mood states, treatment-related symptoms, toxicity, and quality of life in Stage II and III breast cancer patients on conventional treatment.
Methods:
Ninety-eight Stage II and III breast cancer patients underwent surgery followed by adjuvant radiotherapy (RT) or chemotherapy (CT) or both at a cancer center were randomly assigned to receive yoga (n = 45) and supportive therapy counseling (n = 53) over a 24-week period. Intervention consisted of 60-min yoga sessions, daily while the control group was imparted supportive therapy during their hospital visits. Assessments included state-trait anxiety inventory, Beck's depression inventory, symptom checklist, common toxicity criteria, and functional living index-cancer. Assessments were done at baseline, after surgery, before, during, and after RT and six cycles of CT.
Results:
Both groups had similar baseline scores. There were 29 dropouts 12 (yoga) and 17 (controls) following surgery. Sixty-nine participants contributed data to the current analysis (33 in yoga, and 36 in controls). An ANCOVA, adjusting for baseline differences, showed a significant decrease for the yoga intervention as compared to the control group during RT (first result) and CT (second result), in (i) anxiety state by 4.72 and 7.7 points, (ii) depression by 5.74 and 7.25 points, (iii) treatment-related symptoms by 2.34 and 2.97 points, (iv) severity of symptoms by 6.43 and 8.83 points, (v) distress by 7.19 and 13.11 points, and (vi) and improved overall quality of life by 23.9 and 31.2 points as compared to controls. Toxicity was significantly less in the yoga group (P = 0.01) during CT.
Conclusion:
The results suggest a possible use for yoga as a psychotherapeutic intervention in breast cancer patients undergoing conventional treatment.
Keywords
Cancer
depression
meditation
quality of life
yoga
INTRODUCTION
Psychosocial morbidity is common in breast cancer patients after mastectomy and increased during radiotherapy (RT) and chemotherapy (CT), wherein the majority of patients reported some degree of depression, anxiety, social dysfunction, and inability to work.[123] The literature on psychosocial treatment for breast cancer patients provides uniform evidence for an improvement in mood, coping, adjustment, vigor, and a decrease in distressing symptoms.[456] This was seen in women who assumed a sense of self-control and responsibility[12] while standard psychotherapy approaches such as cognitive behavioral techniques or supportive-expressive group therapy encourage problem-solving, sharing, and support, they do not include noncognitive resources such as body and breath awareness, postures, meditation, or spiritual exploration. It is here that complementary and alternative medicine approaches such as yoga may be helpful. There is a growing desire among cancer patients to assume a proactive role and responsibility in their personal care, with most of them evincing an interest in using complementary and alternative medicine and mind-body therapies.[78]
Yoga as a complementary and mind-body therapy is being practised increasingly in both Indian and Western populations. It is an ancient Indian science that has been used for therapeutic benefit in numerous health-care concerns such as diabetes,[9] asthma,[10] hypertension,[11] cardiorespiratory illnesses,[12] anxiety,[13] musculoskeletal disorders,[14] and cancer[15] in which mental stress was believed to play a role. These techniques not only bridge psychosocial and somatic aspects of care but also address the subject's spiritual needs. Yoga techniques such as asanas (postures done with awareness), pranayama (voluntarily regulated nostril breathing), yoga nidra (guided relaxation with imagery) and meditation, promote physical well-being, and mental calmness. Practitioners have to be actively involved in the practice with a sense of self-control and mindful awareness. Such awareness combined with relaxation and attention of mental phenomena will alter the perceptions and mental responses to both external and internal stimuli, slow down reactivity, and responses to such stimuli and instil a greater control over situations. This could be particularly useful in cancer patients who perceive cancer as a threat. In addition, cancer patients find these healthcare alternatives to be more congruent with their own values, beliefs, and philosophical orientations toward health and life.[16]
Various components of yoga such as meditation, breathing exercises, and asanas have also been used in cancer patients with promising results. Several of these studies have shown to improve psychosocial outcomes such as improved affective states, decrease in mood disturbance, stress symptoms and improved quality of life, and spiritual well-being in breast cancer[151718] and in conferring immunological benefits in early breast and prostate cancer patients.[19] Most of these studies have methodological problems with design, some are not randomized[19] and lack effective controls and involve heterogeneous cancer population, with varying stages of their disease and treatment.[17] These studies also do not address the issues of the effect of conventional treatment on psychological morbidity, treatment-related side effects, and quality of life. Moreover, all of these studies on cancer patients were conducted in Western populations. There are no published studies until date evaluating the effect of yoga interventions on cancer patients in India. Yoga being an ancient Indian philosophy and science has a mass appeal and following in India and evaluating its efficacy in Indian cancer patients will help us understand any cross-cultural differences in its impact.
The purpose of the current trial was to study whether a support intervention based on the use of a widely used mind/body and psychospiritual intervention such as yoga would be a viable alternative to standard “supportive therapy and counseling” sessions in breast cancer outpatients undergoing conventional treatment. We, therefore, hypothesized that an integrated yoga-based stress reduction program would help the cancer patients to better cope with their disease and treatment actively, reduce treatment-related symptoms, distress and toxicity, and improve the quality of life during conventional cancer treatment.
In this study, we compared the effects of a 24-week “integrated yoga program” with “supportive therapy” control intervention in operable breast cancer patients undergoing conventional treatment.
PATIENTS AND METHODS
This randomized controlled trial was conducted between 2000 January to June 2004 by two institutions, Swami Vivekananda Yoga Anusandhana Samsthana and Bangalore Institute of Oncology in Bangalore. The institutional review boards of both the institutions approved the study. Ninety-eight recently diagnosed women with stage II and III operable breast cancers (group mean age 49.1 ± 9.45 years) were recruited from Bangalore Institute of Oncology, over a 2½ year period from January 2000 to June 2002. Patients were included if they met the following criteria: (i) Women with recently diagnosed operable breast cancer, (ii) age between 30 and 70 years, (iii) Zubrod’s, performance status 0–2 (ambulatory >50% of time), (iv) high school education, (v) willingness to participate (vi) treatment plan with surgery followed by either or both adjuvant RT and CT. Patients were excluded if they had (i) a concurrent medical condition likely to interfere with the treatment, (ii) any major psychiatric, neurological illness, or autoimmune disorders, and (iii) secondary malignancy. The details of the study were explained to the participants, and their informed consent was obtained.
Baseline assessments were done on 98 patients before their surgery. A total of 69 patients contributed data to the current analyses at the second assessment (postsurgery-4 weeks after surgery), 67 patients during and following RT, and 62 patients during and following CT. The reasons for dropouts were attributed to migration to other hospitals, use of other complementary therapies (e.g., Homeopathy or Ayurveda), lack of interest, time constraints, and other concurrent illness [See trial profile; Figure 1]. However, the order of adjuvant treatments following surgery differed among the subjects with some receiving RT followed by CT, and others vice versa and with some receiving partial CT-3 cycles followed by RT and again 3 cycles of CT. There were four to six assessments depending on the treatment regimen. Irrespective of their treatment regimen, the assessments were scheduled at pre- and post-surgery, pre mid and post-RT and CT. Even though there was heterogeneity with respect to the treatment regimen, this was homogenous when both the groups were compared. Moreover, all participants in the study received the same dose of radiation (50 cGy over 6 weeks) and prescribed standard CT schedules (CMF or FAC).
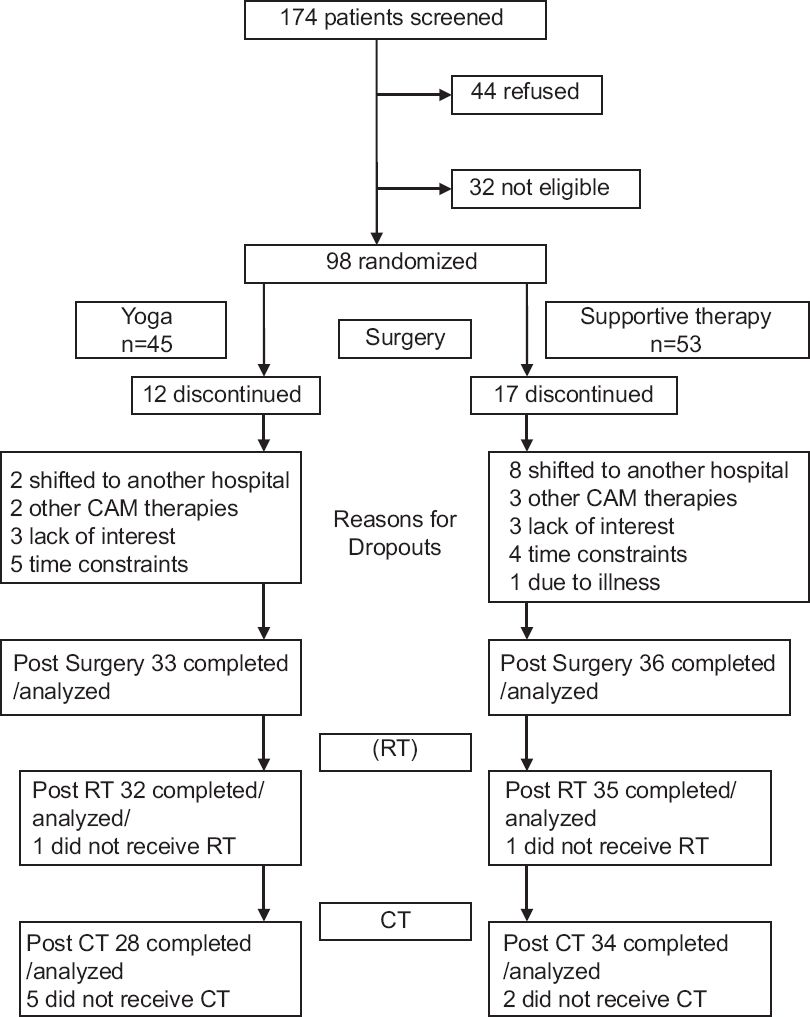
- Trial profile
Measures
At the initial visit, before randomization demographic information, medical history, clinical data, intake of medications, investigative notes, and conventional treatment regimen were ascertained from all consenting participants. Standard self-report questionnaires such as the state-trait anxiety inventory (STAI),[20] Beck's depression inventory (BDI),[21] and functional living index of cancer (FLIC)[22] were imparted to the participants during the study. Subjective symptom checklist was developed during the pilot phase to assess treatment-related side effects, problems with sexuality and image, and relevant psychological and somatic symptoms related to breast cancer. The checklist consisted of 31 such items each evaluated on two dimensions; severity graded from no to very severe (0–4), and distress from not at all to very much (0–4). These scales measured the total number of symptoms experienced, total/mean severity, and distress score and were evaluated previously in a similar breast cancer population.[23] Finally, treatment-related toxicity and side effects were objectively analyzed by the investigators using the World Health Organization Toxicity Criteria[24] during CT.
Randomization
Consenting participants were randomly allocated to either yoga or supportive therapy groups using random numbers generated by a random number table at a different site by a person who had no part in the trial. Randomization was performed using opaque envelopes with group assignments, which were opened sequentially in the order of assignment during recruitment with names and registration numbers written on their covers. The order of randomization was verified with the hospital date of admission records before surgery at study intervals to make sure that field personnel had not altered the sequence of randomization to suit allocation of consenting participants into 2 study arms. Participants were randomized at the initial visit before starting any conventional treatment. Following randomization, participants underwent surgery followed by either RT or CT or both.
Interventions
The intervention group received “integrated yoga program” and the control group received “supportive counseling sessions” both imparted as individual sessions. The objectives of this yoga intervention as described to participants were (i) to develop an opportunity to understand one's personal responses to daily stress and explore ways and means to cope with them (ii) to learn concepts and techniques which bring about stress reduction and change in appraisal, and (iii) to enable the participants to take an active part in their self-care and healing.
The yoga practices consisted of a set of asanas (postures done with awareness) breathing exercises, Pranayama (voluntarily regulated nostril breathing), meditation, and yogic relaxation techniques with imagery. These practices were based on the principles of attention diversion, awareness, and relaxation to cope with stressful experiences.
The sessions began with didactic lectures and interactive sessions on philosophical concepts of yoga and importance of these in managing day-to-day stressful experiences (10 min) beginning every session. This was followed by a preparatory practice (20 min) with few easy yoga postures, breathing exercises and pranayama, and yogic relaxation. The subjects were then guided through any one of these meditation practices for the next 30 min. This included focusing awareness on sounds and chants from Vedic texts[25] or breath awareness and impulses of touch emanating from palms and fingers while practicing yogic mudras, or a dynamic form of meditation which involved practice with eyes closed of four yoga postures interspersed with relaxation while supine, thus achieving a combination of both “stimulating” and “calming,” practice.[26] In meditation, participants try to develop clarity in their thinking, learn to observe their own mind, decrease negative mind states, and develop positive mind states and maintain equipoise in their emotions. On the theistic side, the use of chants and mantras helped them to connect with the divine spiritually. These sessions were followed by informal individual counseling sessions that focused on problems related to impediments in home practice, clarification of participant's doubts, motivation, and supportive interaction with spouses. The participants were also informed about the practical day-to-day application of awareness and relaxation to attain a state of equanimity during stressful situations and were given homework in learning to adapt to such situations by applying these principles.
The subjects were given booklets and instructions on these practices and were encouraged to pursue relevant themes and gain greater depth through proficiency in practice. Subjects were provided audiotapes of these practices for home practice using the instructor's voice so that a familiar voice could be heard on the cassette.
The subjects underwent four such in-person sessions during their pre- and post-operative period and were asked to undergo three in-person sessions every week for 6 weeks during their adjuvant RT treatment in the hospital with self-practice as homework on the remaining days. During CT subjects underwent in-person sessions during their hospital visits for CT administration (once in 21 days) and were also imparted in person sessions by their trainer once a week. The subjects were asked to practice daily for an hour for 6 days/week as homework.
Their homework was monitored on a day-to-day basis by their instructors through telephone calls and weekly house visits. Participants were also encouraged to maintain a daily log listing the yoga practices done, use of audiovisual aids, duration of practice, experience of distressful symptoms, intake of medication, and diet history. There were two instructors in all one being a physician in naturopathy and yoga and other a trained and certified therapist in yoga from the yoga institute. They together supervised and imparted the yoga and supportive therapy intervention with help from trained social workers and counselors at the hospital.
Supportive counseling sessions as control intervention aimed at enriching the patient's knowledge of their disease and treatment options, thereby reducing any apprehensions and anxiety regarding their treatment and involved interaction with the patient's spouses. Subjects and their caretakers were invited to participate in an introductory session lasting 60 min before starting any conventional treatment wherein they were given information about each conventional treatment and management of its related side effects, dietary advice, providing information about a variety of common questions, and showing a patient coping successfully. This counseling was extended over the course of their adjuvant RT and CT cycles during their hospital visits (once in 10 days, 15 min sessions), and participants were encouraged to meet their counselor whenever they had any concerns or issues to discuss. Subjects in the supportive therapy group also completed daily logs or dairies on treatment-related symptoms, medication, and diet during their CT cycles. Similar supportive sessions have been used successfully as a control comparison group to evaluate psychotherapeutic interventions[2728] and similar coping preparations have been effective in controlling CT-related side effects[29] while the goals of yoga intervention were stress reduction and appraisal change the goals of supportive therapy were education, reinforcing social support, and coping preparation.
Statistical methods
Data were analyzed using Statistical procedures were conducted using SPSS version 10 (Sun Micro solutions, Gujarat, India for PC Windows 2000). Study participants underwent Surgery, RT, and CT and interventions were compared for each of these treatments. Mean scores for STAI-state and trait, BDI, symptom checklist, FLIC, and toxicity were calculated for the complete sample. Since order of their adjuvant treatment differed with some receiving RT followed by CT and others receiving CT followed by RT, outcome measures for these groups were therefore compared using analysis of covariance at follow-up intervals with their respective baseline measures as a covariate. Alternatively, intent to treat (ITT) analyses was conducted as repeated measures analyses using SAS institute for advance analytics. These mixed-model analyses use data from all participants who were initially randomized regardless of whether they had observations at each time point. Here estimates of the missing subjects follow-up data based on the observed values of the completers were used to assess the potential impact of the missing data on the results. Subjects were gauged for their regularity of practice during surgery, RT, and CT. This regularity of practice was classified as a category variable, and ANCOVA using baseline measure as covariates was performed to compare effects of regularity of yoga practice with outcome measures during surgery, RT, and CT.
RESULTS
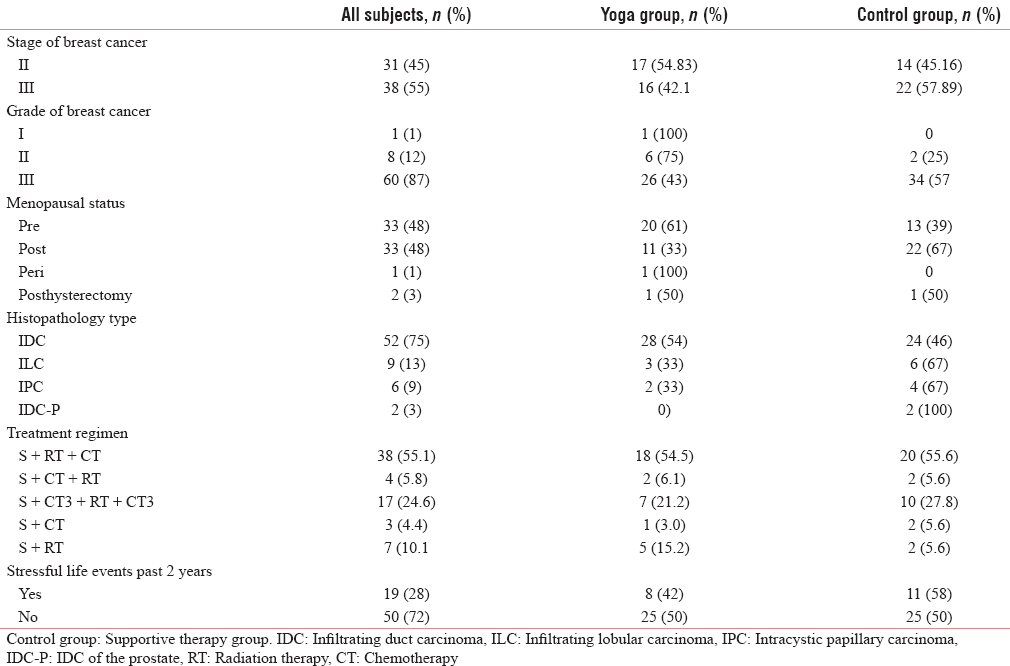
The age, stages of disease, grade, and node status were similar in the yoga and supportive therapy (control) groups [Table 1].
State-trait anxiety inventory - state and trait scores
Participants reported higher levels of anxiety at baseline (before surgery) as compared to other time points. Analysis of covariance using baseline anxiety states as a covariate showed significant decrease in anxiety states following surgery (F [66] = 4.22, P = 0.04], before RT (F [63] = 8.32, P = 0.005), and during RT (F [63] = 7.37, P = 0.009) in the yoga group as compared to controls. Following RT, there was a profound decrease in anxiety states (F [63] = 13.68, P < 0.001), and these effects were maintained during CT (F [58] = 3.84, P < 0.001) and following CT (F [58] = 3.84, P < 0.001). As described in the methods, we also performed repeated measure ITT analyses at follow-up intervals on all randomized subjects with estimates of mixing data elements. ITT analyses showed significant decrease in anxiety states only during CT (t [96] = −2.13, P = 0.04) and following CT (t [96] = −2.11, P = 0.04) compared to controls in the intervention group [Tables 2 and 3].
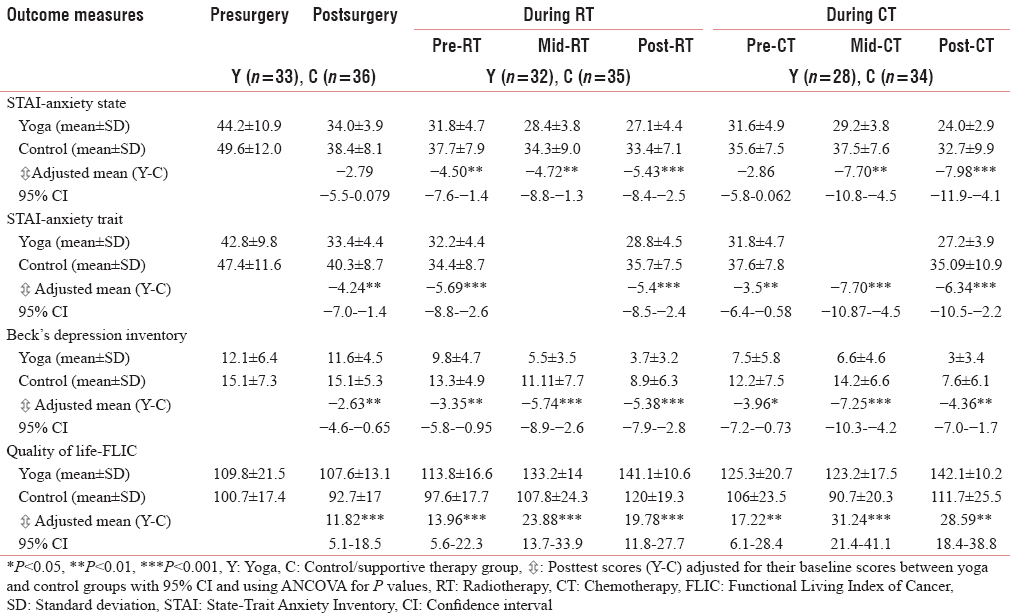
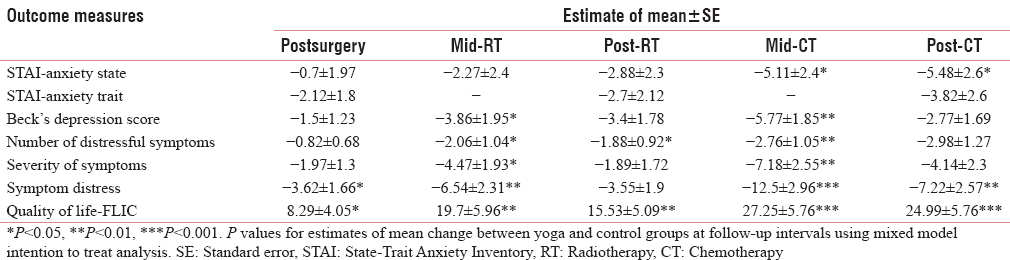
STAI-trait scores were high in yoga group initially in the period between diagnosis and surgery as compared to controls. ANCOVA using baseline anxiety trait score showed significant decrease in anxiety trait scores following surgery, (F [66] = 9.10, P = 0.004), following RT (F [62] =12.96, P = 0.001), and following CT (F [58] = 9.42, P = 0.003) in yoga group as compared to controls. However, ITT analyses performed on all randomized subjects at these follow-up intervals showed no significant changes.
Beck depression scores
Both the groups reported decrease in their depression with time. Analysis of covariance using baseline depression scores as a covariate showed significant decrease in depression following surgery (F [65] = 7.06, P = 0.01), before RT (F [62] = 7.77, P = 0.007), and following RT (F [62] = 17.35, P < 0.001) in the yoga group as compared to controls. The yoga group also showed decrease in depression score before CT (F [57] =6.02, P = 0.02), and after CT (F [57] = 10.90, P = 0.002) as compared to controls. The decrease in depression became more evident during treatment with significant decrease during RT (F [62] = 13.32, P = 0.001) and CT (F [57] = 22.3, P < 0.001). However, an ITT analyses on all randomized subjects showed yoga intervention to significantly reduce depression only during RT (t [96] = −1.98, P = 0.05) and CT (t [96] = −3.12, P = 0.002) [Tables 2 and 3].
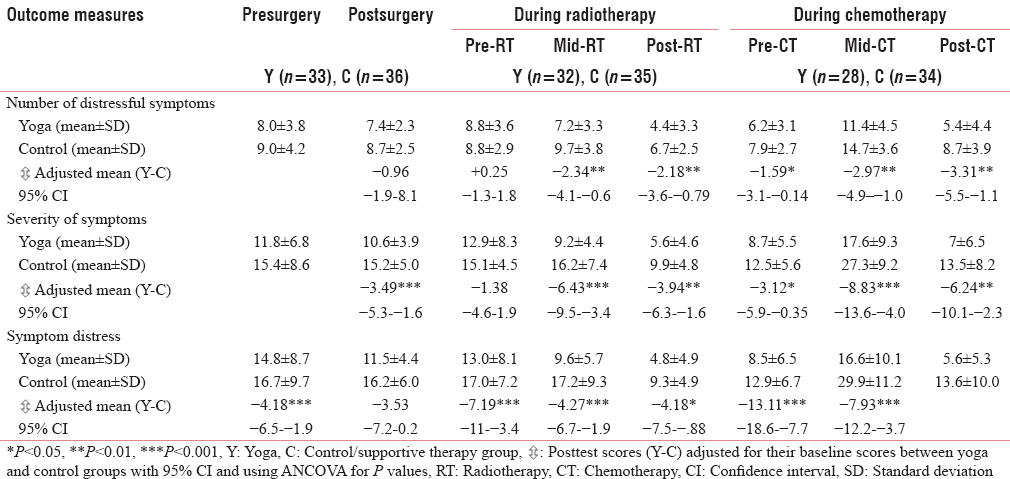
Symptom Scores on symptom checklist
Symptom scores on symptom checklist assessed total no of symptoms, severity of symptoms and total distress experienced. The analysis of covariance using baseline symptom scores as a covariate showed significant decreases in symptom severity (F [66] = 14.11, P < 0.001) and distress (F [66] = 13.40, P = 0.001) following surgery in yoga group as compared to controls. There was also a significant decrease in symptom number (F [63] =7.24, P = 0.009), severity (F [63] = 17.45, P < 0.001), and distress (F [63] = 14.25, P < 0.001) during RT. The intervention effects were more profound during CT showing a significant decrease in number of symptoms (F [58] = 9.43, P = 0.003), severity of symptoms (F [58] = 13.61, P < 0.001), and distress experienced (F [58] = 23.12, P < 0.001) in the yoga group as compared to controls. Following CT, the intervention effects were significant for decrease in symptom number (F [58] = 9.36, P = 0.003), severity (F [58] = 10.27, P = 0.002), and distress (F [58] = 13.79, P < 0.001) in yoga group as compared to controls. ITT analyses showed only a significant decrease in distress following surgery (t [96] = −2.19, P = 0.03) and significant decrease in number (t [96] = −1.97, P = 0.05), (t [96] = −2.65, P = 0.009); severity of symptoms (t [96] = −2.32, P = 0.002), (t [96] = −2.82, P = 0.005) and distress (t [96] = −2.83, P = 0.006), (t [96] = −4.22, P = 0.001) during RT and CT [Tables 3 and 4].
Functional living index of cancer-global quality of life scores
The quality of life scores changed considerably at various stages of treatment. Analysis of covariance using baseline quality of life scores as a covariate showed significant improvements in quality of life following surgery (F [66] = 12.34, P = 0.01) in yoga group as compared to controls. The intervention effects showed more profound improvements in quality of life during RT (F [63] = 22.31, P < 0.001) and CT (F [58] = 40.59, P < 0.001) in the yoga group as compared to controls when controlled for baseline score as a covariate. A repeated measure ITT analyses on all randomized subjects showed similar significant improvements in the quality of life during all the follow-up assessments [Tables 2 and 3].
Common toxicity criteria
Common toxicity criteria guidelines were used to evaluate the CT-induced systemic and organ toxicity with individual toxicity scores graded from zero to four and overall toxicity score extrapolated as a sum of these scores. Independent samples t-test showed yoga group with significantly reduced overall toxicity score as compared to controls (t [58] = −3.873, P = 0.01) (95% confidence interval −5.8 to −0.85).
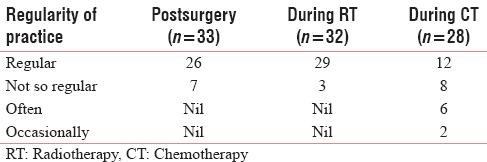
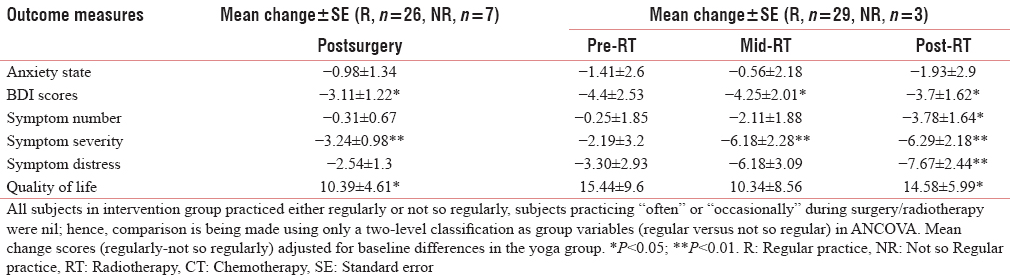
Regularity of practice
Participants in the intervention group were gauged for regularity of practice (classified into four categories of group variables) based on their frequency/average number of days of yoga practice per week. Their regularity of practice was categorized as (i) occasionally (practiced once a week), (ii) often (practice 2–3 times/week), (iii) not so regularly (home practice 4–5 times/week) to (iv) regularly (6 or more times/week) during various stages of conventional treatment. Following surgery, ANCOVA was performed on outcome measures using their baseline scores as a covariate to see the effects of the regularity of practice in the yoga group. Regularity of practice was related to significant decrease in depression scores (F [32] = 6.43, P = 0.017), symptom severity (F [32] = 10.85, P = 0.003) and improvements in quality of life (F [32] = 5.08, P = 0.03) postsurgery. ANCOVA was performed on all outcome measures using baseline measures as a covariate to gauge the effect of the regularity of practice during RT and CT in the yoga group. Subjects who were regular in their yoga practices showed significant decreases for depression (F [29] = 4.44, P = 0.04) and symptom severity (F [31] = 7.33, P = 0.01) during RT. The changes were more profound with continuation of practice with further decrease following RT in depression scores (F [29] = 5.20, P = 0.03), number of symptoms (F [31] = 5.31, P = 0.03), distress (F (31) = 9.86, P = 0.004), and improvements in quality of life (F [31] = 5.91, P = 0.02). However, regularity of practice during CT did not have sufficient power to detect any significant differences with outcome measures during CT [Tables 5 and 6].
DISCUSSION
The previous studies using meditation and yoga in cancer patients have shown beneficial effects in improving mood states, sleep, and quality of life in heterogeneous cancer patients with varying stages of disease and treatment. This is the first randomized controlled study comparing the efficacy of two supportive interventions, yoga with supportive therapy counseling sessions in Stage II and III breast cancer patients undergoing conventional cancer treatment. In the present study, 98 recently diagnosed breast cancer patients were randomly allocated to receive either yoga or supportive therapy before surgery and were followed up with their respective interventions during RT and CT. Following yoga intervention, breast cancer patients showed a significant decrease in reactive and chronic anxiety, depression and distressful symptoms, and improvement in their quality of life during various stages of conventional treatment compared to the control group.
Anxiety state and trait
Participants enrolled in our study had high levels of anxiety state before their surgery as compared to other stages of treatment. Both interventions seemed to reduce anxiety states subsequently. Yoga intervention reduced the anxiety state scores by 10% following surgery, 10.1% and 11.6% during and following RT, and 16.2% and 16.8% during and following CT from their baseline means (adjusted for baseline differences) than the control group indicating that effects of yoga intervention was better than supportive therapy and also when intervention was sustained for a longer duration. Our results are consistent with other studies using meditation and relaxation for generalized anxiety.[4]
Depression
Our study has shown that depression tended to decrease more with time in the yoga group as compared to controls. Yoga intervention decreased depressive symptoms more than the controls by from their baseline means (adjusted for baseline differences) by 19.2% following surgery, 42.4% and 39.7% during and following RT, and 56.5% and 31% during and following CT. Our results are consistent with other studies using relaxation techniques and adjuvant psychological therapy that have shown a similar decrease in depression in these populations (16). Another important factor to note was that our intervention was effective in reducing mild-to-moderate levels of depression and would have been more effective in participants with higher scores for depression.
Quality of life
Our yoga intervention was effective in improving overall quality of life following surgery by 11.2%, compared to supportive therapy from their baseline means (adjusted for baseline differences). The quality of life improved by 22.68% and 30.1% during RT and CT in yoga group compared with supportive therapy. Similarly, yoga helped in reducing self-reported symptoms by 27% and 35%, severity of symptoms by 46.4% and 65.2% and self-reported distress by 42.3% and 82.9% during RT and CT than the control group. The severity and distressful symptoms were more during RT and CT than following their treatment due to treatment-related toxicity and decrease in treatment-related toxicity by yoga intervention could have contributed to decrease in severity and distressful symptoms and consequent improvement in the quality of life. Our results indicate that practising regularly and gaining proficiency in practice could confer greater benefits in these patients.
Conventional treatment-related toxicity
Even though one Grade 4 toxicity cannot be equated to four Grade 1 toxicities, the fact that a composite score is different between the treatment groups still suggests that the overall severity of toxicity is lower in the yoga group indicating that yoga intervention could be of some benefit in reducing the severity of conventional treatment-related toxicity.
Results indicate that yoga intervention did confer some benefit finding, but it was difficult to delineate which aspects of yoga intervention were more beneficial. However, the facets of the yoga-based stress reduction program such as relaxation, meditation, asana, pranayama, social support, opportunity to assume active role in their own care, self-responsibility, and control over ones lives may have been beneficial. Overall, these beneficial effects can be conferred on yoga practices that helped in stress reduction rather than on mere social support and education consistent with other behaviorally oriented programs that have shown better results with stress reduction than purely supportive interventions.[430] It is in this context that our study has been able to elucidate the effects of a yoga-based stress reduction program clearly.
The emotional distress, anxiety, depression, and concerns of cancer patients vary with time, age, stage of disease, duration of illness, and treatment and as such psychosocial interventions should be tailored to the needs of the study population. It is in this context that the homogeneity of support groups has to be maintained to evaluate the effects of structured psychosocial interventions that address specific needs and concerns of the support group.[3132] Earlier studies with meditation in cancer patients have worked on heterogeneous cancer population varying in age, type and, stages of cancer and treatment as compared to the present study which is a homogenous group with respect to their age, disease status, and treatment. One of the major contributions of this study is the longitudinal and prospective follow-up of a homogenous group of breast cancer patients with similar clinical and demographic characteristics undergoing conventional cancer treatment.
We chose to have individual yoga therapy and supportive counseling sessions as compared to group therapy sessions as a group setting could have instilled a sense of community wherein patients could model successful coping and gain self-esteem and motivation in their ability to help others in a group. This could have contributed to improvement in outcome measures thereby, confounding the benefits conferred by our intervention.[3334] Moreover, these individual sessions also helped to understand the specific needs and concerns of participants and monitor individual progress in practice.
Some of the major limitations to the study are, first, that the participants received conventional therapies (radiation, surgery, and CT) in different combinations reflect the usual practices of current breast cancer treatments. Although this introduced heterogeneity into the conventional treatment, there were not significant differences in the frequency of treatment combinations received by the yoga and control groups. It is possible that the yoga therapy worked more effectively for women receiving certain sequences of conventional treatment than others. We were not able to assess this possibility due to the limited sample sizes of these subgroups. The heterogeneity of conventional treatment, to the extent that it might affect yoga therapy, is likely to introduce variability in outcomes that would make it more difficult to show a benefit from yoga. However, the finding that yoga therapy was of benefit in a population receiving different sequences of conventional therapy should increase the generalizability of results, as the benefits are unlikely to be restricted to a specific sequence of conventional treatment. Second, the conclusions following this study can be limited by the fact that although the trail was randomized, many patients chose to participate because they were either willing or hoping to be assigned to the yoga program. This may also be the reason for a greater percentage of dropouts in the control group. In an Indian setting, the enthusiasm among the community for these traditional therapies is so great that it is very difficult to do controlled studies in this area. Third, even though the control group had been given supportive counseling and education only, it is possible that they also had access to information and treatment of similar mind-body therapies elsewhere in the community. Fourth, the contact hours and duration of the yoga intervention was more as compared to supportive therapy and counseling as is with any yoga intervention, and this could have conferred more benefits. However, it should be noted that supportive therapy interventions were used only with an intention of negating the confounding variables such as social support, instructor-patient interaction and education, which were known to improve the psychological and social functioning in cancer patients.[28] Another objective of using social support as a control was with a view of analyzing and identifying the effects of stress reduction conferred by yoga intervention versus a purely supportive intervention on outcome measures. Fifth, because of the desire to incorporate support and education in the yoga program, it is not clear whether a yoga program without support and education would have conferred the same benefits. Our study had an attrition rate of 29%, which is in concordance with other studies that have compared similar stress reduction interventions such as guided relaxation and imagery to standard education and support intervention[35] or standard psychotherapy. The attrition rates being high in this study the actual beneficial effects accrued by the intervention on intention to treat analyses were less when compared to analyses done only on the completers. It is in this context that the results of the intervention have to be viewed with caution.
Our findings are similar to earlier findings, which envisage a greater role for psychological distress in modulating treatment outcomes in terms of toxicity and quality of life.[36] Even though the mood disturbances decrease substantially with time,[1737] yoga group reported better affective states during different phases of treatment than the control group. Our observations are similar to those observed by a structured psychiatric intervention with decrease in affective states and improved methods of coping[7] and meditation in breast cancer patients showing a decrease in mood disturbance, distress, and improved the quality of life.[1517] In summary, our yoga-based intervention was effective in reducing psychological morbidity, distressful symptoms, toxicity, and improving the quality of life in early breast cancer patients undergoing conventional cancer treatments. This was probably facilitated through stress reduction and helping the cancer patients to cope better with their illness at various stages of their conventional treatment. However, larger randomized controlled trails with structured psychiatric interventions as controls are needed to further validate our findings.
Financial support and sponsorship
The Central Council for Research in Yoga and Naturopathy under the Department of AYUSH, Govt. of India, provided financial Support for the present study.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are thankful to Dr. Jayashree, Mrs. Anupama for imparting the yoga intervention. We are grateful to Dr. Frederick Hecht, MD, Director, Research, OCIM, UCSF, for his advice in editing this paper and Dr. Michael Acree, PhD for guidance on statistical methods.
REFERENCES
- Patient perceptions of the side-effects of chemotherapy: The influence of 5HT3 antagonists. Br J Cancer. 1997;76:1055-61.
- [Google Scholar]
- Quality-of-life-adjusted evaluation of adjuvant therapies for operable breast cancer. The International Breast Cancer Study Group. Ann Intern Med. 1991;114:621-8.
- [Google Scholar]
- Psychosocial effects of radiotherapy after mastectomy. Br Med J (Clin Res Ed). 1987;294:1515-8.
- [Google Scholar]
- A comparison of meditation-relaxation and cognitive/behavioral techniques for reducing anxiety and depression in a geriatric population. J Geriatr Psychiatry. 1989;22:231-47.
- [Google Scholar]
- A structured psychiatric intervention for cancer patients. I. Changes over time in methods of coping and affective disturbance. Arch Gen Psychiatry. 1990;47:720-5.
- [Google Scholar]
- Psychotherapy during radiotherapy: Effects on emotional and physical distress. Am J Psychiatry. 1985;142:22-7.
- [Google Scholar]
- The prevalence of complementary/alternative medicine in cancer: A systematic review. Cancer. 1998;83:777-82.
- [Google Scholar]
- Lifestyle modification in management of diabetes mellitus. J Indian Med Assoc. 2002;100:178-80.
- [Google Scholar]
- Effect of yoga breathing exercises (pranayama) on airway reactivity in subjects with asthma. Lancet. 1990;335:1381-3.
- [Google Scholar]
- Non-drug therapy in prevention and control of hypertension. J Assoc Physicians India. 2003;51:1001-6.
- [Google Scholar]
- An introduction to Kundalini yoga meditation techniques that are specific for the treatment of psychiatric disorders. J Altern Complement Med. 2004;10:91-101.
- [Google Scholar]
- Psychophysiologic effects of Hatha Yoga on musculoskeletal and cardiopulmonary function: A literature review. J Altern Complement Med. 2002;8:797-812.
- [Google Scholar]
- Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100:2253-60.
- [Google Scholar]
- Use of alternative therapies among breast cancer outpatients compared with the general population. Altern Ther Health Med. 1999;5:71-6.
- [Google Scholar]
- A randomized, wait-list controlled clinical trial: The effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62:613-22.
- [Google Scholar]
- The efficacy of a mind-body-spirit group for women with breast cancer: A randomized controlled trial. Gen Hosp Psychiatry. 2002;24:238-48.
- [Google Scholar]
- Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448-74.
- [Google Scholar]
- Test Manual for the State Trait Anxiety Inventory. Paolo Alto, CA: Consulting Psychologists Press; 1970.
- Measuring the quality of life of cancer patients: The Functional Living Index-Cancer: Development and validation. J Clin Oncol. 1984;2:472-83.
- [Google Scholar]
- Behavioral Management of Patients with Cancer. National Institute of Mental Health and Neurosciences 1996
- [Google Scholar]
- World Health Organization. WHO Handbook for Reporting Results of Cancer Treatment. Geneva: WHO Offset Publication; 1979.
- Autonomic changes while mentally repeating two syllables – One meaningful and the other neutral. Indian J Physiol Pharmacol. 1998;42:57-63.
- [Google Scholar]
- Oxygen consumption and respiration following two yoga relaxation techniques. Appl Psychophysiol Biofeedback. 2000;25:221-7.
- [Google Scholar]
- Adjuvant psychological therapy for patients with cancer: A prospective randomised trial. BMJ. 1992;304:675-80.
- [Google Scholar]
- Group coping skills instruction and supportive group therapy for cancer patients: A comparison of strategies. J Consult Clin Psychol. 1986;54:802-8.
- [Google Scholar]
- Preparing patients for cancer chemotherapy: Effect of coping preparation and relaxation interventions. J Consult Clin Psychol. 1991;59:518-25.
- [Google Scholar]
- Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2:888-91.
- [Google Scholar]
- Malignant melanoma. Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Arch Gen Psychiatry. 1993;50:681-9.
- [Google Scholar]
- Psychological interventions for cancer patients to enhance the quality of life. J Consult Clin Psychol. 1992;60:552-68.
- [Google Scholar]
- Relaxation therapy as an adjunct in radiation oncology. J Clin Psychol. 1992;48:388-93.
- [Google Scholar]
- Psychosocial consequences of mastectomy: Levels of morbidity and associated factors. J Psychosom Res. 1988;32:383-91.
- [Google Scholar]
- Coping with a breast cancer diagnosis: A prospective study. Health Psychol. 1993;12:16-23.
- [Google Scholar]






