Translate this page into:
Comparative Evaluation of Retrocrural versus Transaortic Neurolytic Celiac Plexus Block for Pain Relief in Patients with Upper Abdominal Malignancy: A Retrospective Observational Study
Address for correspondence: Prof. Anil Agarwal; E-mail: anil_sgpgi@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
To compare retrocrural versus transaortic techniques for neurolytic celiac plexus block (NCPB) in patients suffering from upper abdominal malignancy.
Methods:
In this retrospective observational study between October 2013 and April 2015, 64 patients with inoperable upper abdominal malignancy received fluoroscopy-guided percutaneous NCPB in our institute. Their case files were reviewed and the patients were divided into two groups depending on the technique used to perform NCPB: retrocrural (Group R; n = 36) versus transaortic (Group T; n = 28). The primary outcome measure was pain as assessed with a numeric rating scale (NRS) from 0 to 10; the secondary outcome measures were morphine consumption per day (M), quality of life (QOL) as assessed by comparing the percent of positive responses in each group, and complications if any. These were noted and analyzed prior to intervention and then on day 1, weeks 1, 2, 3, and months 1, 2, 3, 6 following NCPB.
Results:
Patients in Group R had significantly reduced NRS pain scores at week 1, 2, 3, month 1 and 2 as compared to Group T (P < 0.05). Morphine consumption also reduced significantly in Group R at day 1, week 1, 2, and 3 (P < 0.05). QOL was found to be comparable between the groups, and no major complications were noted.
Conclusion:
Retrocrural NCPB provides superior pain relief along with a reduction in morphine consumption as compared to transaortic NCPB in patients with pain due to upper abdominal malignancy.
Keywords
Neurolytic celiac plexus block
Retrocrural
Transaortic
Upper abdominal cancer pain
INTRODUCTION
Neurolytic celiac plexus block (NCPB) is the chemical neurolysis of the visceral afferent fibers that transmit pain from the upper abdominal viscera. For decades, NCPB has been used for alleviation of malignant upper abdominal pain and is also recommended for the same by the WHO Cancer Pain Relief Program. It helps to reduce pain intensity and decrease systemic analgesic intake.[1]
Several percutaneous approaches have been described for NCPB with changes in the target space where the neurolytic agent is injected and the insertion route of the needle. Various imaging modalities such as computed tomography, fluoroscopy, and ultrasonography have been used to guide needle placement in order to make it placement more accurate, increase the efficacy, and decrease complications. However, there is a lack of evidence suggesting that which approach provides the most effective pain relief with minimal complications; this is partially due to lack of well-designed studies comparing different approaches.
Among the various percutaneous techniques performed under fluoroscopic guidance, the classic retrocrural technique describes the placement of the needle in the retrocrural space with the spread of injectate in the space. The transaortic technique, on the other hand, describes the placement of the needle beyond the anterior wall of the aorta as near as possible to its central axis, immediately below the origin of the celiac artery for the destruction of the celiac ganglia.[2] In this retrospective observational study, we have analyzed the comparative efficacy retrocrural versus transaortic NCPB in providing pain relief to patients suffering from upper abdominal malignancy.
METHODS
This retrospective observational study was conducted in the Pain Clinic, Department of Anaesthesia, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India, a Tertiary Care Hospital.
Inclusion criteria
The study population consisted of patients with inoperable upper abdominal malignancies who responded poorly to opioids for pain relief and received fluoroscopy-guided percutaneous NCPB in our institute between October 2013 and April 2015. Sixty-four patients underwent NCPB in this duration, and their case files were reviewed for data collection.
Outcome measures and assessment
The primary outcome measure was a pain as assessed with a numeric rating scale (NRS); the secondary outcome measures were morphine consumption, quality of life (QOL), and side effects if any. The following data were collected: Age, body weight, and time since onset of pain. NRS score for pain (N) between 0 and 10 and morphine consumption (M) were noted prior to intervention and then on day 1, weeks 1, 2, 3, and months 1, 2, 3, 6. The data were collected by clinic interviews and for patients who could not visit the outpatient department, telephonic interviews were done. QOL was assessed with the help of quality of sleep (S), family life (F), and social interaction (Soc) which were recorded at the above-mentioned time points and these were analyzed between the groups by comparing the percent of positive responses in each category to evaluate QOL. Any other unforeseen complications that had been reported were also compared. The patients were divided into two groups depending on the technique used to perform NCPB: Retrocrural (Group R; n = 36) versus transaortic (Group T; n = 28). The technique used was as per the operator's choice as both the techniques are practiced in our institute.
Procedure technique
All the NCPB were conducted in the operation theater under fluoroscopy guidance and hemodynamic monitoring including electrocardiogram, blood pressure, and pulse oximeter monitoring. Intravenous access was obtained with an 18 G cannula and patients were preloaded with 500 ml of normal saline. The procedures were performed under full aseptic precautions with the patient in a prone position with a pillow underneath the abdomen in order to reverse the thoracolumbar lordosis.
In retrocrural NCPB (Group R), L1 vertebral body was identified and the tip of the transverse process of L1 was aligned along its anterolateral margin with 25-35° oblique angulation of the fluoroscope. Needle entry point was above L1 transverse process along the lateral vertebral body margin; 22 G 15 cm spinal needles were placed on both sides following local anesthetic infiltration. The end points were confirmed on lateral fluoroscopy with needle tips positioned at the anterior margin of the vertebral body. About 1–2 ml of nonionic contrast was injected and confirm correct needle placement in anteroposterior (AP) and lateral fluoroscopic views and to rule out the intravascular injection. 5 ml of 1% lignocaine was then administered through each needle, followed after 5 min by 15 ml of 100% alcohol on each side Figure 1.

- (a-f) C-arm guided retrocrural technique for celiac plexus block
In transaortic NCPB (Group T), only unilateral left-sided transaortic block was performed in a manner similar as described above; 22 G 15 cm spinal needle was inserted from the left side and advanced until it penetrated the aortic wall suggested by feeling of loss of resistance and blood expulsion from the needle hub after removing needle stylet. The needle was advanced until the cessation of blood expulsion. Following negative aspiration 1-2 ml of nonionic contrast was injected to rule out intravascular injection and confirm correct needle placement in AP and lateral fluoroscopic views. 10 ml of 1% lignocaine was administered, followed after 5 min by 20 ml of 100% alcohol Figure 2.
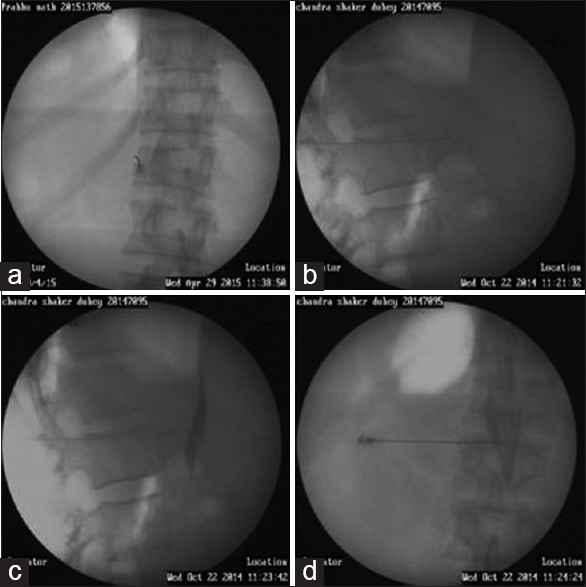
- (a-d) C-arm guided transaortic technique for celiac plexus block
The needles were flushed with 1 ml of 0.9% normal saline and then removed. All the patients were observed in postanesthesia care unit for 4 h; vital signs (pulse, blood pressure, and oxygen saturation) were monitored and complications, if any, were managed and documented.
Statistical analysis
Demographic data were analyzed with one-way ANOVA for continuous variables and Chi-square test for categorical variables. The NRS pain scores and QOL were analyzed with Mann–Whitney U-test, morphine consumption was analyzed with Student's t-test, and the incidences of side effects were analyzed with Fisher's exact test. The package SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. P < 0.05 was considered as significant.
RESULTS
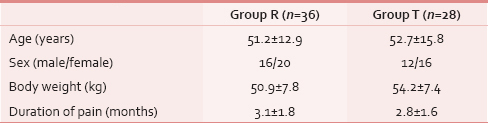
Sixty-four patients suffering from advanced upper abdominal malignancy underwent NCPB for the alleviation of pain during October 2103-April 2015. There was no difference among the groups as regards to age, sex, weight distribution, and duration of pain (P > 0.05) [Table 1]. Diagnosis of patients is presented as numbers [Table 2].

In both the groups, reduction in NRS scores was observed following celiac plexus block. When comparing the two groups, it was found that patients in Group R had significantly reduced NRS pain scores as compared to patients in Group T at week 1, 2, 3, month 1 and 2 (P < 0.05). However, 3rd month onward, NRS pain scores in both the groups were comparable [Figure 3].

- Pain as assessed by numeric rating scale in the various groups. Data are presented as a mean ± standard deviation. *P < 0.05 during within the group comparison. #P < 0.05 during between group comparison
Preprocedure morphine consumption was comparable between the two groups (P > 0.05). Patients in both the groups reported a significant decrease in morphine requirement postprocedure (P < 0.05). When comparing the two groups, morphine consumption was reduced in Group R on day 1, week 1, week 2, and week 3 as compared to Group T (P < 0.05). Thereafter, morphine requirement in both the groups was comparable until the end of assessment period (P > 0.05) Figure 4.

- Morphine consumption in the various groups. Data are presented as a mean ± standard deviation. *P < 0.05 during within the group comparison. #P < 0.05 during between group comparison
There was no significant difference in the QOL of patients between two groups in terms of quality of sleep, interaction with family, and social interaction [Table 3].

Most common complication reported was transient back ache at the site of injection in 61% patients in Group R and 50% patients in Group T (P > 0.05). This was mild in intensity and resolved by itself within a week. Self-limiting diarrhea was another complication seen in 16.7% patients in Group R and 14.3% in Group T (P > 0.05), which resolved within 2-5 days. Hypotension was observed in 22.2% patients in Group R and 21.4% patients in Group T during the procedure (P > 0.05) which was managed by intravascular fluid resuscitation. All the patients were discharged from the hospital on the same day once their hemodynamics were stabilized, usually within 4 h. On follow-up, none of the patients described features suggestive of postural hypotension. No major complications were observed.
DISCUSSION
NCPB is the most widely used interventional procedure for upper abdominal pain relief with demonstrated efficacy for patients with malignant and chronic nonmalignant pain. It has been shown to provide a long lasting benefit for 70-90% of patients with pancreatic and intraabdominal cancers[3] with the benefit ranging from 50 days till up to the time of death.[4] All our patients who received NCPB, irrespective of the technique used, demonstrated a significant reduction in visual analog scale scores following the procedure, thus reaffirming the efficacy of NCPB.[5]
The technique for celiac plexus block was first described by Kappis in 1914. Since then, various approaches have been developed differing in the route of insertion of the needle, the final position of the needle, and imaging modalities to improve the accuracy of needle placement.[6] However, there is a lack of well-designed studies comparing different approaches.
In this retrospective observational study, we have compared the fluoroscopy-guided retrocrural technique versus the transaortic technique, and report that pain was significantly reduced in Group R till the 2nd month postprocedure (P < 0.05). Morphine consumption also was reduced in Group R as compared to Group T up to the 3rd week postprocedure (P < 0.05). Subsequently, however, pain relief and morphine consumption were found to be comparable in both the study groups till the end of the assessment period, i.e., 6 months (P > 0.05).
Among the various posterior percutaneous techniques performed under fluoroscopic guidance, the classic retrocrural technique describes the bilateral needle placement and injection of neurolytic agent posterior-cephalad to diaphragm in the retrocrural space. The injectate is found to first concentrate posterior to the aorta and in front of the L1 vertebral body where it blocks the retroaortic celiac plexus fibers. It then diffuses cephalad to block the splanchnic nerves. It finally encircles the aorta only when enough drug is injected to transgress the diaphragm by diffusing caudad through the aortic hiatus.[7] It has thus been suggested that the retrocrural technique is more likely to produce splanchnic nerve block rather than actual celiac plexus block and is also referred to as a “deep splanchnic block”.[8]
The transaortic technique, on the other hand, describes the placement of the needle beyond the anterior wall of the aorta as near as possible to its central axis, immediately below the origin of the celiac artery for the destruction of the celiac ganglia. The injectate thus encircles the aorta, covering first the anterior, and then the posterior surfaces of the aorta.[9] It is known that advanced abdominal malignancy can spread and engulf the celiac ganglia, thereby preventing its adequate coverage by the neurolytic agents when injected anterior to the aorta. Deposition of the agent more proximally may help to overcome this problem. This might explain the superiority of the retrocrural technique as observed in our study. However, this could be confounded by the fact that the volume of injectate used in the retrocrural technique was more (30 ml) than that used in the transaortic technique (20 ml). This is a limitation of our study due to its retrospective observational design, and it would be interesting to compare the two techniques in a prospective randomized controlled trial, thus minimizing any confounding factors.
Post NCPB, any residual or breakthrough pain was managed as per the WHO ladder. The differences observed in morphine consumption indicate that in retrocrural group, postprocedure, satisfactory pain relief was achieved with the use of simple analgesics and weak opioids like tramadol, obviating the need to consume high doses of strong opioids like morphine. The maximum benefit lasted up to the 3rd week postprocedure. Frequent side effects such as dry mouth, drowsiness, constipation, and nausea and vomiting have been often reported with the use of morphine in cancer patients[10] and reduction in morphine requirement is known to improve social and cognitive scales and hence facilitate better end of life care.[11] Reduction of morphine consumption was thus a valuable advantage of the retrocrural technique.
The importance of QOL issues for cancer patients is well-recognized and over the past several decades numerous studies have addressed the physical, emotional, social, and sexual well-being of cancer patients. A number of cancer-specific QOL measures have been developed[12] and various previous studies evaluating NCPB in pancreatic malignancies have demonstrated improved physical, emotional, and social well-being in patients receiving NCPB).[1314] We found the QOL to be similar, both pre- and post-procedure in both the groups. This may be attributed to the fact that our study population consisted of a much more diverse group of diagnoses, and that factors such as progression of the tumor, malignancy-related complications, and reduction in efficacy of the block over time contributed in hindering significant improvement. Another limitation of the present study is that we did not use a standardized QOL questionnaire.
NCPB is usually a safe procedure with rare serious complications. These complications are usually caused due to either chemical or traumatic injury to the surrounding structures. The most common complication that we observed was a transient backache at the site of injection. Previously, hypotension secondary to sympathetic denervation has been documented in almost one-third patients and self-limiting diarrhea in about 40% patients as a result of unopposed parasympathetic activity. These were also observed in our group of patients as well, irrespective of the technique used for NCPB. Various other complications have also been reported such as shoulder pain, dysesthesia, impaired ejaculation, diaphragmatic paralysis, and pneumothorax. These complications are uncommon. As regards major neurological complications, only 11 cases of paraplegia have been reported in the literature.[2] None of the rarer complications were observed in any of our patients.
CONCLUSION
In this retrospective observational study, we conclude that retrocrural neurolytic celiac plexus provides superior pain relief along with a reduction in morphine consumption as compared to transaortic neurolytic celiac plexus in patients with pain due to upper abdominal malignancy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The role of neurolytic celiac plexus block in the treatment of pancreatic cancer pain. Transplant Proc. 2008;40:1200-4.
- [Google Scholar]
- Celiac plexus block in pancreatic neuroendocrine tumors. Clin J Oncol Nurs. 2011;15:218-20.
- [Google Scholar]
- Celiac plexus neurolysis for abdominal cancer pain: A systematic review. Pain Med. 2013;14:1140-63.
- [Google Scholar]
- European Palliative Care Research Collaborative (EPCRC). Sympathetic blocks for visceral cancer pain management: A systematic review and EAPC recommendations. Crit Rev Oncol Hematol. 2015;96:577-83.
- [Google Scholar]
- CT-guided percutaneous neurolytic celiac plexus block technique. Abdom Imaging. 2006;31:710-8.
- [Google Scholar]
- Atlas of Interventional Pain Management: Expert Consult: Online. Philadelphia: Elsevier Health Sciences; 2014. p. :2768.
- Celiac plexus block: A roentgenographic, anatomic study of technique and spread of solution in patients and corpses. Anesth Analg. 1981;60:369-79.
- [Google Scholar]
- Celiac plexus neurolysis with the modified transaortic approach. Radiology. 1990;175:274-6.
- [Google Scholar]
- A multispecialty approach to the diagnosis and management of pancreatic cancer. Am J Gastroenterol. 2000;95:17-31.
- [Google Scholar]
- Comparative study of the effects of the retrocrural celiac plexus block versus splanchnic nerve block, C-arm guided, for upper gastrointestinal tract tumors on pain relief and the quality of life at a six-month follow up. Korean J Pain. 2015;28:22-31.
- [Google Scholar]
- Assessing quality of life in adult cancer survivors (QLACS) Qual Life Res. 2005;14:1007-23.
- [Google Scholar]
- Comparison between celiac plexus block and morphine treatment on quality of life in patients with pancreatic cancer pain. Pain. 1996;64:597-602.
- [Google Scholar]
- Efficacy of coeliac plexus and splanchnic nerve blockades in body and tail located pancreatic cancer pain. Eur J Pain. 2004;8:539-45.
- [Google Scholar]






