Translate this page into:
Continuous Low-Dose Oral Chemotherapy in Recurrent and Persistent Carcinoma of Cervix Following Chemoradiation: A Comparative Study Between Prolonged Oral Cyclophosphamide and Oral Etoposide
Address for correspondence: Dr. Upasana Baruah, E-mail: drupasana@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
To compare the efficacy and toxicities of low-dose oral cyclophosphamide and oral etoposide in patients with persistent and recurrent cervical cancer with gross pelvic disease following full course of chemoradiation therapy.
Materials and Methods:
30 patients with recurrent and persistent cervical cancer with gross pelvic disease were enrolled in this trial. The patients were randomly divided into two groups of 15 patients each with one group receiving low dose oral cyclophosphamide (100 mg/day) and the other group receiving low-dose oral etoposide (50 mg/day). Results were statistically analysed by IBM SPSS Statistics 19.
Results:
Oral etoposide was not well tolerated with grade 2 neutropenia occurring in 33.3% and grade 3 neutropenia in 6.6% and thrombocytopenia occurring in 13.3%. Oral cyclophosphamide group on the other hand was better tolerated with none of the patients having thrombocytopenia and 6.6% patients having grade 2 neutropenia. There were two complete response (15.38%) and one partial response at the end of study (7.6%) in the cyclophosphamide group whereas there was no complete response and two partial response (16.6%) in the oral etoposide group.
Conclusion:
Long-term, low-dose oral etoposide was found to be less tolerated without any significant effect with patients with persistent and recurrent cervical cancer with gross pelvic disease following full course of chemoradiation therapy in contrast to oral cyclophosphamide which was found to be effective and well-tolerated by the patients.
Keywords
Metronomic therapy
Oral cyclophosphamide
Oral etoposide
Recurrent carcinoma cervix
INTRODUCTION
Studies on various experimental tumor models have demonstrated the antitumor effect of continuous low-dose chemotherapy on tumor cells.[12] The success of low dose chemotherapy is believed to be based on continuous administration, activation of cancer immunology, and antiangiogenic activity. Continuous low-dose therapy is found to cause more cancer cell destruction as there are greater percentages of cells which proliferate and move into the cell cycle. Also, the tumor cells get less opportunity to regenerate due to continuous administration of the drug.[3]
An additional advantage of administering chemotherapy at continuous low doses is the reduced occurrence of the various dose limiting side effects of cytotoxic chemotherapy, as a consequence of which the drug is better tolerated amongst the patients, enabling the administration of larger or equivalent amount of chemotherapy.[4]
Most patients who relapse after full dose of primary radiotherapy or who have persistent disease following radiotherapy are not candidates for further radiotherapy. Pelvic exenteration is an option available for small central recurrence but cannot be done in patients with tumor involving the pelvic side walls, with metastasis and those who are poor surgical candidates. The overall survival and prognosis is poor for these patients even following chemotherapy and they are taken up for palliative care only.[567]
Based on the results available to us from the existing literature,[189] on low dose oral chemotherapy, we devised a low-dose protocol using oral cyclophosphamide and oral etoposide, which was expected to be administered to patients for more than 6 months without significant acute or cumulative toxicity in patients with recurrent and persistent cervical cancer following radiation therapy.
Aim
To compare the efficacy and toxicities of low-dose oral cyclophosphamide and oral etoposide in patients with persistent and recurrent cervical cancer with gross pelvic disease following full course of chemoradiation therapy.
MATERIALS AND METHODS
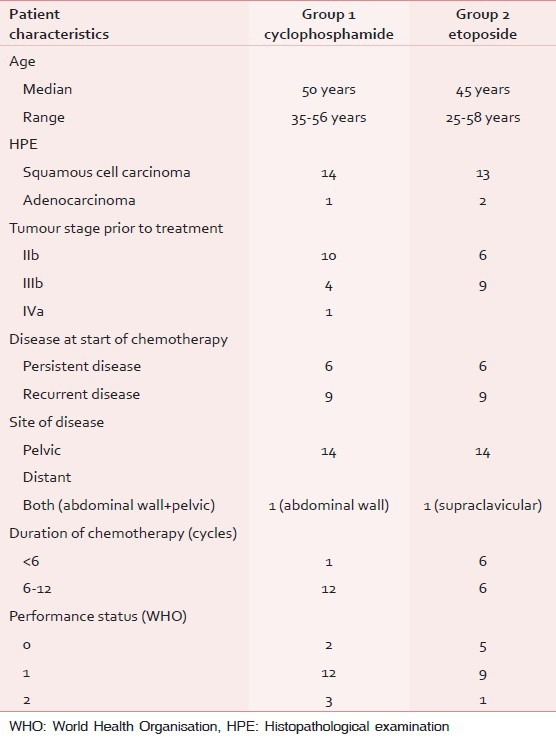
Patient eligibility: 30 patients with recurrent and persistent cervical cancer with gross pelvic disease were enrolled in this trial from our institution over the period Aug 2012 to Dec 2012. They were followed up till Dec 2013. The patients were randomly divided into two groups of 15 patients each with one group receiving low dose oral cyclophosphamide (100 mg/day) and the other group receiving oral etoposide (50 mg/day). Results were statistically analyzed by IBM SPSS Statistics 19. The selected patients were not considered suitable for any other treatment and were under palliative care. The patient characteristics are shown in Table 1.
Eligibility criteria included age < 60 years, histological proof of malignancy, and WHO performance status of 0 to 2, life expectancy of > 3 months, and at least a single site of measurable (two-dimensional) disease. Hematopoietic: WBC at least 3,000/mm3. Absolute granulocyte count at least 1,500/mm3, platelets at least 100,000/mm3. Hepatic: Bilirubin no more than 1.5 times normal, AST no more than three times normal, Alkaline phosphatase no more than three times normal, Renal creatinine no greater than 2.0 mg/dl. Other: Body surface area at least 1 m2, no requirement for intravenous hydration or nutritional support, no significant infection and absence of other malignancy. In addition all the patients underwent complete physical examination, complete blood counts, liver function test, blood urea and serum creatinine analysis, routine urine examination, and chest radiograph as a part of pretreatment evaluation. Blood tests were repeated every 3 weeks. Computerized tomogram of abdomen and was done prior to start of chemotherapy and was repeated later for response assessment. Informed consent was taken prior to treatment.
The dose of oral cyclophosphamide was 100 mg given for 14 days every 21 days and for oral etoposide was 50 mg given for 14 days every 21 days. Response was defined according to RESIST criteria.[10]
RESULTS
A total of 30 patients were taken up for study and were randomly divided into two groups of 15 patients each. All the patients had completed prior conventional chemoradiation with brachytherapy. At the end of 12 months two patients were lost to follow up in the oral cyclophosphamide group and three patients were lost to follow up in the oral etoposide group. Rest of the patients were evaluated for response to treatment. In patients with stable disease and partial response, treatment was continued and in patients with complete response additional three cycles of chemotherapy was given following which treatment was discontinued. Treatment was discontinued in patients with progressive disease and unacceptable levels of toxicity. Toxicity analysis could be done in all the patients as patients were lost on follow up only toward the end of study period [Table 2]. Oral etoposide was not well tolerated with grade 2 neutropenia occurring in 33.3% and grade 3 neutropenia in 6.6% and thrombocytopenia occurring in 13.3%. Oral cyclophosphamide group on the other hand was better tolerated with none of the patients having thrombocytopenia and 6.6% patients having grade 2 neutropenia. Anemia developed in 53.3% patients in the etoposide group and 40% required blood transfusion whereas it was 40% in the cyclophosphamide group and only 13.3% required blood transfusion. Six patients in the oral etoposide group showed progressive disease at the end of 6 month of study whereas only two patients had progressive disease in the cyclophosphamide group implying poor response in the etoposide group. At the end of study there were 6 deaths due to progressive disease in the etoposide group whereas there were three deaths in the oral cyclophosphamide group. There were two complete responses (15.38%) and one partial response at the end of study (7.6%) with overall response of 23.07% in the cyclophosphamide group. PFS in the complete responders were over 6 months. There was no complete response but two partial responses (16.6%) in the oral etoposide group [Table 3]. There were three stable patients in the oral cyclophosphamide and one stable patient in the oral etoposide group. Median overall survival was 14.3 months in the oral cyclophosphamide group and 11.5 months in the oral etoposide group (P < 0.045) [Figure 1].



- Overall survival of the enrolled patients (months)
DISCUSSION
Low-dose oral chemotherapy is a promising new treatment option in the field of oncology which is continuously evolving. There are limited data of its role in gynecologic malignancies.
Use of oral etoposide in the treatment of ovarian cancer as a second line therapy is well known whereas very few studies are available of its role in recurrent cervical cancer.[1112] The overall response in these studies ranged from 11.8% to 28.6%.[1112]
Similarly, no study using of oral cyclophosphamide in recurrent or advanced cervical carcinoma was available but its efficacy in other advanced malignancies such as carcinoma ovary and breast have been documented.[913] In our study oral etoposide therapy was less tolerated with overall response rate of 16.6% (partial response) which was similar to other similar to other studies.[1011] In our study, no complete response was noted in the oral etoposide group. Even though no therapy was discontinued for toxicity, six patients (50%) had to discontinue therapy due to progressive disease at the end of 6 month of study period. The overall response in the oral cyclophosphamide group was 23.07% with two complete responses and one partial response. Only mild hematologic toxicity was noted in the cyclophosphamide group as compared to the oral etoposide group. In contrast to oral etoposide only one patient in the cyclophosphamide group showed disease progression at the end of 6 month of study period. Thus, in the oral cyclophosphamide group greater number of patients could be given treatment for more than six cycles (92.30%) [Table 1].
The overall response between the two groups was not found to be statistically significant (P > 0.29), which means that both drugs have got a potential in managing patients with recurrent/persistent cervical cancer following chemoradiation. However, median overall survival at the end of study period was better for the oral cyclophosphamide group at 14.3 months as compared to oral etoposide which was 11.5 months (P < 0.045). Thus, considering the low toxicity of and the better median overall survival period of oral cyclophosphamide it can be concluded that oral cyclophosphamide is a better option for patients with recurrent and persistent cervical cancer following chemoradiation. However, our study had some drawbacks due to the small sample size and loss of follow up of few patients and hence the findings needs to be confirmed by further randomized clinical trials.
CONCLUSION
To conclude as carcinoma cervix occurs mostly in the lower socioeconomic group of people, especially in India where patients cannot afford expensive chemotherapy and costly surgical interventions, low-dose oral cyclophosphamide because of its affordable price can be a practical alternative.
ACKNOWLEDGEMENTS
We would like to thank all the patients who have participated in the study. We would also like to thank Dr. Bhargab J Saikia, Dept of Medical Oncology, all the supporting staff and the Department of Palliative Oncology for their support.
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Cancer Res. 2000;60:1878-86.
- [Google Scholar]
- Continuous low dose therapy with vinblastine and VEGF receptor-2 antibody induces sustained tumor regression without overt toxicity. J Clin Invest. 2000;105:R15-24.
- [Google Scholar]
- The anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer. 2004;4:423e36.
- [Google Scholar]
- Prognostic factors for survival in patients with recurrent cervical cancer previously treated with radiotherapy. Int J Gynecol Cancer. 2010;20:834-40.
- [Google Scholar]
- Paclitaxel and cisplatin as first-line therapy in recurrent or advanced squamous cell carcinom a of the cervix: A Gynecologic Oncology Group study. J Clin Oncol. 1999;17:2676-80.
- [Google Scholar]
- Cisplatin and gem citabine in patients with metastatic cervical cancer. Gan To Kagaku Ryoho. 2004;31:1057-62.
- [Google Scholar]
- Antitumor effects in mice of low-dose (metronomic) cyclophosphamide administered continuously through the drinking water. Cancer Res. 2002;62:2731-5.
- [Google Scholar]
- Low dose oral methotrexate and cyclophosphamide in metastatic breast cancer: Antitumour activity and correlation with vascular endothelial growth factor levels. Ann Oncol. 2002;13:73-80.
- [Google Scholar]
- Response assessment in solid tumours (RECIST): Version 1.1 and Supporting Papers. Eur J Cancer. 2009;45:225-310.
- [Google Scholar]
- Prolonged oral etoposide in recurrent or advanced squamous cell carcinoma of the cervix: A gynaecologic oncologic group study. Gynecol Oncol. 1998;70:263-6.
- [Google Scholar]
- Clinical trial of daily low-dose oral etoposide for patients with residual and recurrent cancer of ovary or uterus. J Obstet Gynaecol. 1995;21:569-76.
- [Google Scholar]
- Oral cyclophosphamide in recurrent ovarian cancer. Asia Pac J Clin Oncol 2013 Epub Ahead of Print
- [Google Scholar]






