Translate this page into:
Translation and Linguistic Validation of the Multidimensional Dyspnea Profile into Hindi in a Palliative Care Setting
*Corresponding author: Mikael Segerlantz, Department of Palliative Care and Advanced Home Health Care, Primary Health Care Skåne, Region Skåne, Lund, Sweden. mikael.segerlantz@med.lu.se
-
Received: ,
Accepted: ,
How to cite this article: Kökeritz M, Dufberg L, Palat G, Ekström M, Brun E, Segerlantz M. Translation and Linguistic Validation of the Multidimensional Dyspnea Profile into Hindi in a Palliative Care Setting. Indian J Palliat Care 2024;30:252-9. doi: 10.25259/IJPC_46_2024
Abstract
Objectives:
The Multidimensional Dyspnea Profile (MDP) comprehensively addresses dyspnea, incorporating both perceptual and affective components, and has proven effective in assessing breathlessness among patients with chronic lung conditions. Despite its validation in High-Income Countries, its applicability in Low/Middle-Income countries remains uncertain. Additionally, the MDP has not been translated into Hindi or validated in an Indian context. Our aim was to translate the MDP into Hindi and linguistically validate it for use in an Indian palliative care setting, with a high rate of illiteracy.
Materials and Methods:
The comprehensibility and acceptability of the translated MDP in Hindi were assessed through in-depth interviews with seven Hindi-speaking patients with cancer. The study focused on tailoring the MDP in a socioeconomically disadvantaged population characterized by a high rate of illiteracy. The translation process involved forward and backward translations by independent certified translators, with input from in-country Indian palliative medicine physicians and healthcare personnel.
Results:
The Hindi version of the MDP was adapted for use in an Indian context and in a population with a high rate of illiteracy, aligning with international guidelines for Patient-Reported Outcomes demonstrating relevance in a specific cultural and healthcare context. The MDP increased healthcare staff ’s understanding of underlying causes of dyspnea in a socioeconomically disadvantaged population enrolled into palliative care and with a high rate of illiteracy.
Conclusion:
The study underscores the importance of linguistic validation and cultural adaptation in ensuring the applicability of Patient-Reported Outcomes measures in diverse healthcare settings. Because the MDP can be perceived as time-consuming, selected parts of the instrument may be used as needed.
Keywords
Dyspnoea
Breathlessness
Multidimensional
Palliative care
Hindi
Illiteracy
INTRODUCTION
Dyspnoea (or breathlessness), the subjective feeling of breathing discomfort, is a cardinal symptom of heart and lung disease.[1] The American Thoracic Society defines dyspnoea as ‘a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity.’ The prevalence of dyspnoea is high among the middle-aged and elderly populations[2] and increases steeply with increasing disease severity across a range of underlying conditions.[3] Dyspnoea is strongly linked to adverse health outcomes and reduced physical activity, often creating a vicious cycle of deconditioning and further worsening breathlessness. Psychological symptoms such as anxiety and depression are reported at a higher rate in patients with dyspnoea and, as a consequence, are associated with impaired quality of life, loss of will to live near death, increased risk of hospitalisation and earlier death. The importance of dyspnoea has been highlighted in recent years, and dyspnoea has been included in the evaluation of disease severity and prognosis in patients with chronic obstructive pulmonary disease (COPD).[4] Dyspnoea is, in fact, a stronger predictor of mortality than the level of airflow limitation in COPD[5] and a negative prognostic factor in people with heart failure.[6,7] Dyspnoea is also common in patients with advanced cancer, with a reported prevalence of 50–70% and as high as 90% in patients with lung cancer.[4]
The individual can differentiate several dimensions of this symptom: The experienced intensity and unpleasantness, the associated emotional response and the functional impact on the person’s life.[1] Despite its serious impact, dyspnoea remains frequently underreported, unmeasured and undertreated in clinical practice.[8,9] Unpleasantness, emotional responses and the sensory qualities of dyspnoea have been measured in different studies using varying (disease-specific) scales, wordings and time frames.[1,10] This lack of standardisation makes it difficult to compare findings between studies, patient populations and settings. Importantly, standardised multidimensional measurement is essential to adequately capture treatment effects in clinical settings.
The multidimensional dyspnoea profile (MDP)
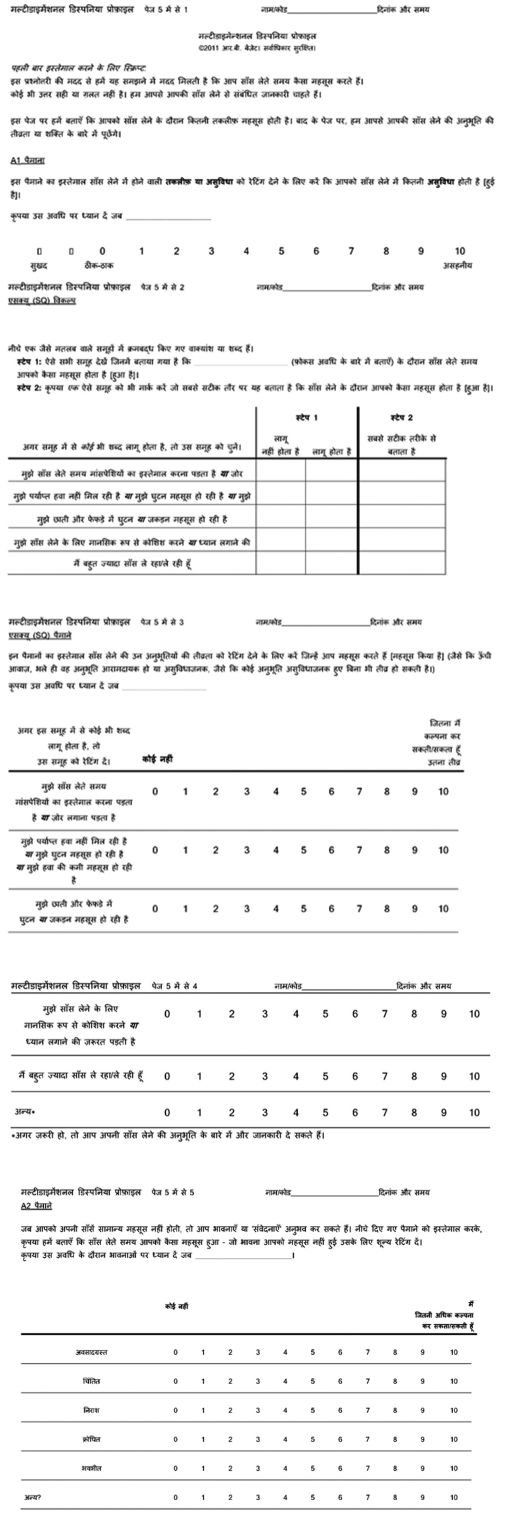
The MDP has been developed to include all aspects of dyspnoea, both perceptual and affective, each of which is evaluated separately.[11] The questionnaire has been shown to be useful and valid in assessing breathlessness in patients with a variety of chronic lung conditions, such as COPD and interstitial lung disease[2,3] and in patients with cardiorespiratory disease.[12] The user defines the time frame or situation of the measurement. MDP assesses the patient’s experience of dyspnoea for a specific time (yesterday or over the past 2 weeks, for instance), and the patient is expected to focus on that specific period when responding. The questionnaire is made up of 5 ‘applies/does not apply’-questions and 11 different rating scales divided into three domains. The first domain uses a numeric scale of 0–10 to rate the overall unpleasantness of dyspnoea. The second domain evaluates the perceptual aspects of dyspnoea using numeric scales and ‘applies/does not apply’-questions. The third domain evaluates the affective aspects of dyspnoea using numerical scales.[4] The first and second domains consider the ‘immediate perception of dyspnoea’, and the third domain is the ‘emotional response.’[4] For example, opioids have been found to have a stronger effect on the unpleasantness and associated anxiety than on the intensity of dyspnoea[13] and pulmonary rehabilitation has been shown to improve the patient’s coping and function in relation to dyspnoea with the symptom intensity possibly remaining unchanged.[14]
The MDP was developed in English by Banzett et al. in the United States in 2011 and has since been translated into different languages, including Swedish, French for France, French for Belgium, French for Canada, German, Dutch for Belgium, Dutch for the Netherlands, English for Canada and English for the UK, Japanese and Spanish.[10] The MDP can be used free of charge in the context of non-funded academic research. A distribution fee applies in the context of funded academic and commercial use. Supplementary materials and figures are available on the European Respiratory Journal website. However, the instrument’s usability is still limited by the few languages it has been translated into.
Health care and the importance of palliative care in India
Although the MDP has been validated in high-income countries, its relevance in low/middle-income countries is yet unclear. In India, a low/middle-income country, the public healthcare system is heavily underfinanced, with limited free healthcare options and a multitude of private care options offered at varying costs.[13] Today, approximately 83 million people (6%) of India’s population are living in poverty, amongst which 51 million people (4%) are living in extreme poverty,[14,15] meaning living on <1.90 US dollars a day.[14] Moreover, despite a high prevalence of dyspnoea in patients with advanced-stage cancer,[5] the MDP has not been validated in a palliative care setting. It is estimated that only 1–2% of all patients in need of palliative care in India receive it[16] compared to 14% worldwide.[17] There is currently no tool for the multidimensional measurement of dyspnoea available in Hindi, a language spoken by over 500 million people,[10,17] which highlights the need for the MDP to be translated into this language and validated in an Indian context. A Hindi version of the MDP could facilitate improved detection and measurement in research and clinical practice in India, as well as comparisons of dyspnoea across languages. We, therefore, aimed to develop a linguistically validated Hindi translation of the MDP.
Aim
The study aims to translate the MDP into Hindi and linguistically validate it for use in an Indian palliative care setting with a high rate of illiteracy.
MATERIALS AND METHODS
Study design
Structured translation and linguistic validation of the MDP[9] from the original American English into Hindi conducted in collaboration with the company Mapi Development, SAS, Language Services Unit, Lyon, France, specialised in translation and linguistic validation of patient reported outcome (PRO) measures.
Research ethics and patient consent
The study was approved by the Ethics Committee at the MNJIORCC in Hyderabad, India. The patients and family members were given oral information from health-care staff regarding the study. Informed consent was obtained from all patients. The consent forms were signed by the patients either in writing or with their fingerprints. The consent form was also signed by witnesses and the healthcare staff.
The translation and linguistic validation were performed in accordance with the guidelines and regulations from Mapi Research Trust, Lyon, France, available at COA translation and linguistic validation | Mapi Research Trust (mapi-trust.org).
Translation
Translation and linguistic validation were conducted in a structured, multistage process according to international guidelines.[18,19] After permission to translate, the MDP was obtained from the developer,[10] and the original instrument was forwards translated into Hindi independently by two certified translators, native in Hindi, assigned by Translated S.R.L, Rome, Italy. The forwards translations were analysed and reconciled by a third translator into one version, Version 1. In step two, Version 1 was then backwards translated to the original language (American English). The backwards translation was reviewed and compared to the original by an in-country linguistic consultant provided by the translation bureau above, and appropriate changes were implemented to obtain translated Version 2.0. The translation process took place from the 13th of October to the 2nd of November 2022
Clinicians’ review
The translation Version 2.0 was reviewed by two Indian physicians (authors GP, SR) at Mehdi Nawaz Jung Institute for Oncology and Regional Cancer Registry (MNJIORCC). They provided detailed feedback on the understandability and validity of key concepts to users of the instrument and people with dyspnoea. The changes were made to obtain Version 2.1 before initiating the study.
Patient selection
Patients included in the study had all been admitted to palliative care, either in-home care or at the Kumudini Devi Hospice. Inclusion criteria were 18 years or older, conscious, able to answer questions regarding breathlessness, native speakers of Hindi and an affirmative response to the question, ‘Have you had any breathing problems at rest or during activity that was distressful during the past 2 weeks?’ Patients younger than 18 years, non-native speakers of Hindi and those with cognitive impairment were excluded.
Linguistic validation
The MDP translated Version 2.1 in Hindi was read out aloud to the patient, at one single point, by one of the healthcare staff, and the patient answered the individual questions. All data were collected by experienced palliative care nurses or physicians using a standardised protocol. The staff then conducted the cognitive interviews to investigate the clarity, understandability and acceptability of the MDP instrument. The validated questions for the patients are shown in Appendix 1. The participants commented on their understanding of each item and suggested alternative formulations for problematic wordings [Appendix 2].
The staff who conducted the patient interviews was then themselves interviewed, to gain an understanding of any underlying problems or misunderstandings of the translated Version 2.1, expressed by the patients. The validated questions for the staff are shown in Appendix 3. The staff who conducted the interviews commented on problems or misunderstandings and suggested alternative formulations for problematic wordings [Appendix 2]. The sample size was determined by reaching data saturation.
After summarising, revising and proofreading, a final linguistically validated MDP in Hindi was issued as Version 3 [Appendix 4]. The linguistic validation process occurred from November 28th to December 16th, 2022.
Patient and Public Involvement statement
The study focuses on patients admitted to palliative care. We believe that involving patients and the public in palliative care research is of paramount importance, as it helps us better understand the experiences and needs of those who are most vulnerable and, thus, in need of palliative care. The patient and public involvement (PPI) throughout the execution and analysis of this research, we actively sought input and feedback both from the patients enrolled in the study and the healthcare workers responsible for their palliative care.
RESULTS
Patients’ demographics
The study patients had different cancer diagnoses, as follows: Lung (n = 3), rectal (n = 2) and breast cancer (n = 1) and additionally, in one patient, an unknown tumour diagnosis. Amongst these patients, four were males and three were females, aged between 42 and 68 years. Dyspnoea severity, assessed by the patients’ responses to the statement ‘I am not getting enough air’ on the shortness of breath questionnaire (SQ), using a scale of 0–10 to indicate the intensity of breathing sensations, exhibited variability, with scores ranging from 3 (n = 1), 4 (n = 2), 5 (n = 1) to 7 (n = 3). Most patients (n = 5) received care at home, while two were in hospice care [Table 1]. Data listing the demographics of the patient group included, ranging from educational level to household income. Provides an overview of the socioeconomic status of the patients. [Supplementary Table 1].
Translation
After extensive input from the clinicians’ review and the in-country linguistic consultant, revisions were made to the initial translations, especially regarding the wording of the descriptive items (second domain).
Linguistic validation
A total of 7 Hindi-speaking patients were included. The interviews were conducted with 5 patients within the palliative home care service and 2 patients at the Kumudini Devi Hospice. Demographics are presented in Table 1. Out of the 7 participants, only six patients were able to complete all questions in the form. All patients answered the validation questions during the interviews.
| Patients | Gender | Age (years) | Cancer diagnoses | Dyspnoea (0-10) | Care setting |
|---|---|---|---|---|---|
| 1 | Male | 67 | Lung | 7 | Home |
| 2 | Male | 68 | Lung | 5 | Home |
| 3 | Female | 53 | Rectum | 4 | Home |
| 4 | Male | 43 | Lung | 3 | Home |
| 5 | Male | Missing | Unknown | 7 | Hospice |
| 6 | Female | 42 | Rectum | 4 | Hospice |
| 7 | Female | 57 | Breast | 7 | Home |
In total, three doctors and one nurse were interviewed and answered the validation questions for the healthcare staff.
In total, five patients (72%) stated that they did not find the MDP questions difficult to understand, whereas two patients (28%) found it difficult to understand. However, two patients (28%) left an incoherent description of the symptom as ‘the most accurate’ in step 2 sensory qualities (SQ) choice, which was mismatched with the answer reported in step 1 (SQ choice) [Appendix 1]. These discrepancies were either that the patient did not answer the question in step 2 at all, or they chose a symptom that they in step 1 had marked as ‘does not apply, ’ or they chose more than one symptom as ‘most accurate. ’
There was also a discrepancy when comparing the question of ‘applies/does not apply’ in SQ choice and the grading of the symptom on a scale from 0 to 10 in the SQ scales. In all, four patients (57%) reported symptoms as ‘does not apply’ on SQ choice while still grading it above a ‘0’ in SQ scales when using Version 2.1 of the translated MDP.
All the healthcare staff (4/4) stated during their interviews that they had gained insight into and more information about the patients’ dyspnoea from using the MDP. They found the instrument useful both in the palliative home-care service and at the hospice. The shortcoming of the translated MDP instrument, Version 2.1, highlighted by the healthcare professionals was the wording of some statements that still could be perceived as difficult to understand and thus lead to misunderstanding and incoherent answers in patients with low levels of education. Another concern was that although the MDP provided a better overview of various qualities of a patient’s breathlessness, it was time-consuming, which could be a barrier for use in severely ill patients (at least several or all items of the instrument).
Final revisions of the translated MDP
Before validation of the translated MDP instrument (Version 2.1) started, feedback was provided by healthcare professionals that the ‘radio metaphor’ found in the American English version of the MDP and shown in Appendix 5 would be difficult to comprehend amongst patients with a low education level and in an Indian context. The recommendation was to remove this metaphor from the translated Version 2.1. To verify this concern, the validation of the MDP initially included the radio metaphor. When asked, patients stated that they were either ‘irritated by music’ or that they ‘listened to music to relieve their symptoms,’ interpreted as a misconception of this metaphor. Consequently, the metaphor was removed from Versions 2.1. Changes made included exchanging specific words for more commonly used ones to facilitate the understanding of the MDP in the studied population. In SQ scales, the exact word ‘scale’ in English was added instead of the translated word, as ‘scale’ is commonly used and well understood in Hindi, according to the physicians involved in the project. In the affective (A2) scales, the word for ‘some’ in Hindi was added to the instructions to make them easier to understand.
After the above-mentioned editing of the translated MDP Versions 2.1, Final Version 3 was then issued.
The Hindi version was approved by the Mapi Institute (August 28, 2023) and added to their database for future use by other researchers.
The exact revisions made during the validation process can be seen in Appendix 2.
DISCUSSION
This study presents a linguistically validated version of the MDP in Hindi, which facilitates multidimensional assessment of dyspnoea using this instrument in a population of approximately 500 million Hindi speakers.[10,17,20] The present version was tailored for use in palliative care in a poor, underprivileged population with a high rate of illiteracy. The translation was conducted in accordance with international guidelines for PROs provided by the Mapi Institute, who are experts in linguistic validation of PRO instruments for cross-cultural use.
The MDP was developed for measurement across diseases. However, this is, to our knowledge, the first time the MDP has been tested and evaluated in a palliative care setting. Our findings highlighted new aspects that needed to be addressed and considered. The MDP instrument is time-consuming and, in a group of patients with a critical illness and often with a high burden of symptoms, the ability to perform and fully comprehend the MDP could be affected. However, selectable parts of the MDP can be chosen and used individually instead of the whole MDP,[6] reducing the time consumption and thus the burden on the patient but also care providers in an otherwise busy healthcare environment.
Our linguistic validation of the MDP instrument was conducted in a population living in very limited socioeconomic circumstances and with low levels of education, which may have affected the capacity for abstract thinking.[19,21] For example, it was difficult for the patients in our validation project to comprehend and thus rate their symptoms from 0 to 10. A misconception of the Numeric Rating Scale (NRS) scaling was evident. The local health professional suggested a more commonly used system of grading that was easier for patients to relate to. The question was then often rephrased, and the patients were instead asked to grade their symptoms in reference to the national currency, the Indian Rupee. One rupee (INR) was equivalent to 10, a half rupee equivalent to 5 and so forth. In addition, the language of our MDP Version 2.2 may still need some minor linguistic simplifications adapted to a group of patients with low levels of education.
CONCLUSION
This project has produced a linguistically validated version of MDP in Hindi, the first tool for multi-dimensional measurement of dyspnoea for Hindi-speaking patients in India. The MDP instrument increased understanding of the different underlying causes of dyspnoea in a palliative care setting. The MDP instrument can be perceived as time-consuming; consequently, selected parts of the instrument may be used as needed. In a group of patients with low levels of education and limited socio-economic circumstances, the language level can still be perceived as difficult. Therefore, it is important to ensure that the patient has a full understanding of the different MDP questions.
Acknowledgements
The authors wish to thank Vineela Rapelli for administrative support regarding the study and Dr. Hrudai, Dr. Wajid, Dr. Prajwell and Mr. Swarup, who contributed to the clinical review of the MDP.
Data management and sharing
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Author’s contributions
Conception, design: ME, MS, EB. Local adjustment of study design: MS, EB, GP, SR. Participated in the translation and revision of important intellectual content: GP, SR. Interviews, validation: LD, MK. Conception of the article and continuous revision of the article: LD, MK, ME, MS, EB. All authors approved the version to be published.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study, waiver number (MNJIORCC 2022).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
One author (Dr Magnus Ekström) was supported by an unrestricted grant from the Swedish Research Council (Dnr: 2019-02081).
References
- An Official American Thoracic Society Statement: Update on the Mechanisms, Assessment, and Management of Dyspnea. Am J Respir Crit Care Med. 2012;185:435-52.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of Dyspnoea Prevalence: Results from the BOLD Study. Eur Respir J. 2014;43:1610-20.
- [CrossRef] [PubMed] [Google Scholar]
- Are There Differences in the Prevalence of Palliative Care-related Problems in People Living with Advanced Cancer and Eight Non-cancer Conditions? A Systematic Review. J Pain Symptom Manage. 2014;48:660-77.
- [CrossRef] [PubMed] [Google Scholar]
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. Available from: http://www.gold/copd.org [Last accessed on 2016 Oct 31]
- [Google Scholar]
- Dyspnea is a Better Predictor of 5-year Survival than Airway Obstruction in Patients with COPD. Chest. 2002;121:1434-40.
- [CrossRef] [PubMed] [Google Scholar]
- Higher New York Heart Association Classes and Increased Mortality and Hospitalization in Patients with Heart Failure and Preserved Left Ventricular Function. Am Heart J. 2006;151:444-50.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic Significance of Dyspnea in Patients Referred for Cardiac Stress Testing. N Engl J Med. 2005;353:1889-98.
- [CrossRef] [PubMed] [Google Scholar]
- Is Chronic Breathlessness Less Recognised and Treated Compared with Chronic Pain? A Case-based Randomised Controlled Trial. Eur Respir J. 2018;52:1800887.
- [CrossRef] [PubMed] [Google Scholar]
- Invisibility of Breathlessness in Clinical Consultations: A Cross-sectional, National Online Survey. Eur Respir J. 2022;60:2201603.
- [CrossRef] [PubMed] [Google Scholar]
- Multidimensional Dyspnea Profile: An Instrument for Clinical and Laboratory Research. Eur Respir J. 2015;45:1681-91.
- [CrossRef] [PubMed] [Google Scholar]
- Dyspnoea-12 and Multidimensional Dyspnea Profile: Systematic Review of Use and Properties. J Pain Symptom Manage. 2022;63:e75-87.
- [CrossRef] [PubMed] [Google Scholar]
- The Management of Chronic Breathlessness in Patients with Advanced and Terminal Illness. BMJ. 2015;350:g7617.
- [CrossRef] [PubMed] [Google Scholar]
- Using Laboratory Models to Test Treatment: Morphine Reduces Dyspnea and Hypercapnic Ventilatory Response. Am J Respir Crit Care Med. 2011;184:920-7.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Pulmonary Rehabilitation on the Major Dimensions of Dyspnea in COPD. COPD. 2013;10:425-35.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability and Validity of the Multidimensional Dyspnea Profile. Chest. 2012;141:1546-53.
- [CrossRef] [PubMed] [Google Scholar]
- Test-retest Reliability of Multidimensional Dyspnea Profile Recall Ratings in the Emergency Department: A Prospective, Longitudinal Study. BMC Emerg Med. 2012;12:6.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and Assessment of Breathlessness in the Clinical Setting. Expert Rev Respir Med. 2014;8:151-61.
- [CrossRef] [PubMed] [Google Scholar]
- Multinational Trials-Recommendations on the Translations Required, Approaches to Using the Same Language in Different Countries, and the Approaches to Support Pooling the Data: The ISPOR Patient-Reported Outcomes Translation and Linguistic Validation Good Research Practices Task Force report. Value Health. 2009;12:430-40.
- [CrossRef] [PubMed] [Google Scholar]
- Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005;8:94-104.
- [CrossRef] [PubMed] [Google Scholar]
- Real-life Assessment of the Multidimensional Nature of Dyspnoea in COPD Outpatients. Eur Respir J. 2016;47:1668-79.
- [CrossRef] [PubMed] [Google Scholar]
- Swedish Translation and Linguistic Validation of the Multidimensional Dyspnoea Profile. Eur Clin Respir J. 2016;3:32665.
- [CrossRef] [PubMed] [Google Scholar]
Appendix 1: Validation questions for the patients
Were the MDP questions difficult to understand? Were there any specific words in the MDP questionnaire that were hard to understand?
Appendix 2: Revisions in detail
Revisions were made to Version 2.1 regarding specific formulation of sentences or words that patients or healthcare professionals commented on were difficult to understand or convey to the participant. As seen below. These changes resulted in Final Version 3 of the MDP.
Revision made to the Version 2.1: Script for first-time use: The radio metaphor [Appendix 5] was removed (1/12/22). The spelling of dyspnoea (written in the Hindi alphabet) was edited to be spelt as it is pronounced, thus removing the letter ‘p’ (5/12/22).
A1 Scales: The word ‘pleasant’ was changed to ‘comfort’ and the word ‘neutral’ to ‘normal’. (5/12/22).
SQ Scales: The translated word for ‘scale’ in Hindi was changed to the exact word scale in English written in the Hindi alphabet (5/12/22).
A2 Scales: The translated word for ‘some’ in Hindi was added to the instructions (5/12/22).
Appendix 3: Validation questions for the healthcare staff
Do you have more knowledge about the patient’s dyspnoea after using the MDP compared to before? Do you think that the MDP would be useful for in-home care/hospice? Do you see any disadvantages to the MDP (in general or in this setting)? If you were to suggest changes to the MDP, what would they be?
Appendix 4: The MDP translated version 3 in Hindi
Appendix 5: The radio metaphor
“On this page we ask you to tell us how unpleasant your breathing feels. On a later page we will ask you about the intensity or strength of your breathing sensations. The distinction between these two aspects of breathing sensation might be made clearer if you think of listening to a sound, such as a radio. As the volume of the sound increases, I can ask you how loud it sounds or how unpleasant it is to hear it. For example, music that you hate can be unpleasant even when the volume is low and will become more unpleasant as the volume increases; music that you like will not be unpleasant, even when the volume increases.”
| Variable | Number (%) |
|---|---|
| Age (years) | 55 mean |
| Gender | |
| Male | 4 (57) |
| Female | 3 (43) |
| Literate | |
| Yes | 6 (86) |
| No | 1 (14) |
| Education | |
| No education | 1 (14) |
| 1–10 years | 5 (72) |
| 11+years | 1 (14) |
| Employment | |
| Unemployed | 3 (43) |
| Daily labourer | 2 (28) |
| Employed | 1 (14) |
| Retired | 1 (14) |
| Household income (per/month, INR) | |
| 5000–10000 | 3 (43) |
| >10000 | 4 (57) |
| White card | |
| Yes | 18 (75) |
| No | 6 (25) |
| Cancer diagnosis | |
| Lung | 3 (43) |
| Rectal | 2 (29) |
| Breast | 1 (14) |
| Unknown | 1 (14) |






