Translate this page into:
Death Preparation and Quality of Life amongst Family Caregivers of Terminal Cancer Patients: A Multicentre Cross-sectional Study
*Corresponding author: In Cheol Hwang, Department of Family Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, South Korea. spfe0211@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kim Y, Lee J, Lee Y, Lee C, Hwang S, Seo M, et al. Death Preparation and Quality of Life amongst Family Caregivers of Terminal Cancer Patients: A Multicentre Cross-sectional Study. Indian J Palliat Care. 2025;31:8-14. doi: 10.25259/IJPC_213_2024
Abstract
Objectives:
Caring for ill cancer patients imposes a considerable burden on families, significantly reducing quality of life (QoL). This study examined the association between death preparation and QoL amongst family caregivers (FCs) of terminally ill patients with cancer in South Korea.
Materials and Methods:
A multicentre cross-sectional survey using questionnaires was conducted in nine inpatient palliative care units in South Korea. Data from 170 FCs who answered questions about preparedness for death were analysed. A stepwise multivariate logistic model was used to identify the factors associated with FCs’ QoL. The estimated QoL scores were also compared between the groups according to preparedness level.
Results:
Factors associated with high QoL included old age, fewer daily caregiving hours, fewer caregiving durations and practical preparedness for death. The well-prepared group had significantly higher QoL scores in the burdensome domain. This significant association remained robust in FCs with low educational or social support levels, poor resilience and dysfunctional families.
Conclusion:
Practically, well-prepared FCs experienced a high QoL in hospice care settings. FCs are likely to benefit from assessment and encouragement of their preparedness for death.
Keywords
Caregivers
Neoplasms
Preparedness for death
Quality of life
Terminal care
INTRODUCTION
Caring for ill cancer patients imposes a considerable burden on families, significantly reducing quality of life (QoL).[1-3] Based on the close linkage of family QoL with caregiving activities and patient QoL,[4,5] the importance of QoL, not only for patients but also for their families, has been highlighted as a goal of palliative care in clinical guidelines.[6] The QoL of family caregivers (FCs) varies according to the disease trajectory;[7] However, overall, palliative care rather than curative settings affects QoL more.[8] In hospice settings, several factors have been identified as associated with FC QoL, such as caregiving burden, economic burden and caregiver mental health.[8,9]
Preparedness for death is defined as caregivers’ perception of their readiness for a patient’s death.[10] It involves how accurately a caregiver knows the patient’s prognosis and how he/she prepares emotionally for the patient’s death. Preparedness can be assessed in terms of emotional and practical aspects,[11] which indicates that readiness for a patient’s death consists of emotions related to the death itself and challenges in daily living, such as new household responsibilities and funeral arrangements. The preparation stage has been reportedly associated with caregivers’ coping strategies, perception of financial adequacy, bereavement response and mental health, such as depression and anxiety.[10] Thus, a lack of preparedness for death can be linked to poor FC QoL, as unprepared FCs might experience a higher care burden and more emotional distress than well-prepared FCs. Although several studies have reported associations between FC preparedness and caregiving outcomes, such as bereavement response or emotional distress, studies regarding the association of preparedness with caregivers’ QoL are relatively scarce.[12] In a Swedish study of widowers, a low degree of preparedness increased the risk of low or moderate QoL 4–5 years after the loss (relative risk, 1.18; 95% confidence interval [CI], 1.3– 2.6).[13] However, to our knowledge, no study has examined preparedness for death and QoL amongst FCs of patients with cancer in Korea. As end-of-life care should be considered under diverse sociocultural circumstances,[14] tailored research on different cultures or countries is needed. Therefore, we aimed to assess the preparedness state of FCs of patients with terminal cancer and examine the association between FC preparedness and their QoL.
MATERIALS AND METHODS
Study design and participants
This study was based on a multicentre cross-sectional survey conducted in nine inpatient palliative care units in South Korea. We collected data from June 2021 to May 2023, mostly within 1 week of admission. FCs were eligible to participate if they were responsible for most patient care, were older than 20 years and were able to provide information regarding the survey. We consecutively administered questionnaires to eligible FCs. The researchers explained the aim and scope of the survey to the FCs and administered self-report questionnaires after obtaining their consent. To minimise missing values, the researchers checked the responses immediately after receiving the completed surveys and inquired about any missing data. A total of 170 FCs were included in the statistical analyses.
Measures
QoL
The Korean version of the Caregiver QoL Index-Cancer (CQOLC-K) was used to assess FCs’ QoL. The reliability/validity of CQOLC-K was documented in a previous study.[15] It consists of 35 items, each rated on a five-point scale ranging from 0 (not at all) to 4 (very much). Ten items pertain to burden, seven to disruptiveness, seven to positive adaptation, three to financial concerns and eight to additional factors (sleep disruption, satisfaction with sexual functioning, day-to-day focus, mental strain, information about the illness, patient protection, management of patient’s pain and family interest in caregiving). A total score was obtained by adding all item scores, and domain scores were calculated by adding the item scores for each domain. The maximal total score was 140, with higher scores indicating better QoL.[15] We categorised the participants into low- and high-QoL groups according to the mean value (70) of the total CQOLC-K score.
Preparedness for death
The FCs’ perceptions of their readiness for patient death were assessed in terms of both emotional and practical aspects. Emotional preparedness was evaluated based on responses to the question, ‘I am emotionally well-prepared for the patient’s death’. Practical preparedness was evaluated based on responses to the question, ‘I am practically well-prepared for the patient’s death such as new responsibilities, future plans and funeral arrangements’. Responses were ranked on a five-point scale as follows: (1) Not at all, (2) no, (3) average, (4) yes and (5) very much so.[10] We categorised participants into low and high-preparedness groups according to the median value of each preparedness score.
Covariates
With reference to our prior study on a similar issue,[16] demographic information, such as age, sex, relationship with the patient, education level, marital status and religion, was obtained. Relationships with patients were categorised as ‘spouse’ or ‘others’ (including children, siblings, parents and others). Education level was categorised as ‘high school or lower’ or ‘college or higher’. Marital status was categorised as ‘married’ or ‘unmarried’ (including never married, divorced, separated or widowed). Religious affiliation was categorised as ‘no religion’ or ‘religion’ (including Protestantism, Catholicism, Buddhism and others). FCs’ resilience was assessed using the Connor– Davidson Resilience Scale, which comprises 25 items on a five-point scale from 0 (not at all confident) to 4 (completely confident). Higher scores indicated greater resilience.[17]
Objective burden of care, social support and family functioning levels were assessed to evaluate the caregiving environment. The burden of care was evaluated as caregiving hours per day, days per week and months per year. As an evaluation tool for social support level, the Medical Outcome Study Social Support Survey was used, which comprises 19 items rated on a five-point scale, from 1 (not at all) to 5 (all of the time). Higher scores indicate greater social support.[18] The family function was assessed using the Korean version of the family Adaptation, Partnership, Growth, Affection and Resolve (APGAR). The family APGAR comprises five items rated on a three-point scale ranging from 0 (hardly ever) to 2 (almost always). The total score ranged from 0 to 10, with higher scores indicating greater satisfaction with family functioning.[19]
Statistical analysis
The characteristics of participants according to the total QoL score of FCs were compared using the Chi-square test for categorical variables and the t-test for continuous variables. Logistic regression analyses were performed to identify factors associated with high QoL, and linear regression models were used to estimate QOL scores in total and in four subdomains (burdensomeness, disruptiveness, positive adaptation and financial concerns) according to preparedness level. Regression coefficients for total QoL scores were calculated for the educational level, resilience, social support and family function subgroups. All statistical analyses were performed using STATA/MP version 17.0 (StataCorp., College Station, TX, USA), and a statistically significant P-value was defined as <0.05.
RESULTS
Characteristics of study participants
Table 1 shows the characteristics of the study participants according to FCs’ QoL. Low and high QoL scores were determined using mean CQOLC-K total scores. Amongst the 150 participants, 76 and 94 belonged to the low- and high-QoL groups, respectively. The mean age of study participants was 50.6 ± 13.1 and 56.2 ± 12.3 in the low- and high-QoL group, respectively (P = 0.005). There were no significant differences in sex, relationship with the patient, education level or religious affiliation, according to the FC QoL. However, the proportion of married individuals was higher in the high-QoL group (84.8%) than that in the low-QoL group (P = 0.019). The resilience score was also higher in the high-QoL group than in the low-QoL group (62.3 ± 17.1 vs. 54.0 ± 16.4; P = 0.002). Moreover, the high-QoL group tended to spend less time on caregiving than the low-QoL group. The high-QoL group showed higher social support and family function scores. Regarding preparedness for death, the interquartile ranges of preparedness scores were 2–4 and 3–4 for emotional and practical preparedness, respectively. Compared with the low-QoL group, the high-QoL group showed higher scores in both emotional (P = 0.001) and practical preparedness (P < 0.001).
| Range | FC’s QoL | Highd (n=94) | P-value | ||
|---|---|---|---|---|---|
| IQR | Lowd (n=76) | ||||
| Caregiver’s factors | |||||
| Age | 44–62 | 50.6±13.1 | 56.2±12.3 | 0.005 | |
| Female sex | 61 (80.3) | 68 (72.3) | 0.230 | ||
| Spouse | 32 (42.1) | 37 (39.4) | 0.717 | ||
| Education more than college | 38 (50.0) | 56 (60.2) | 0.184 | ||
| Married | 53 (69.7) | 78 (84.8) | 0.019 | ||
| Professing a religion | 38 (50.7) | 52 (55.9) | 0.498 | ||
| Resiliencea | 47–69 | 0–100 | 54.0±16.4 | 62.3±17.1 | 0.002 |
| Caregiving environment | |||||
| Hours of caregiving per day | 12–24 | 0–24 | 20.2±6.6 | 17.5±8.2 | 0.023 |
| Days of caregiving per week | 5–7 | 0–7 | 6.0±1.7 | 5.3±2.1 | 0.027 |
| Months of caregiving | 1–9 | 10.1±14.6 | 6.6±9.7 | 0.066 | |
| Level of social supportb | 61–91 | 0–100 | 72.0±19.9 | 78.0±15.6 | 0.034 |
| Family function levelc | 5–8 | 0–10 | 5.6±2.7 | 6.8±2.4 | 0.006 |
| Preparing for death | |||||
| Emotionally | 2–4 | 1–5 | 2.9±1.0 | 3.4±0.9 | 0.001 |
| Practically | 3–4 | 1–5 | 2.7±1.0 | 3.6±0.7 | <0.001 |
FC: Family caregiver, QoL: Quality of life, IQR: interquartile range. Data are presented as mean±standard deviation or number (percentage). P-values were obtained using the t-test or Chi-square test. aBy Connor–Davidson Resilience Scale; bBy Medical Outcome Study Social Support Survey; cBy Adaptation, Partnership, Growth, Affection and Resolve; dBy total score (mean value, 70) of Caregiver Quality of Life Index-Cancer
Factors associated with high QoL
Table 2 presents the results of the univariate and multivariate logistic analyses for high QoL. In univariate analysis, older FC (odds ratio [OR], 1.04 per 1-year increase; 95% CI, 1.01– 1.06), fewer caregiving days (OR, 0.83 per 1-day increase; 95% CI, 0.70–0.98), hours (OR, 0.95 per 1-h increase; 95% CI, 0.91–0.99) and being married (OR, 2.42; 95% CI, 1.14– 5.13) were associated with high QoL. Besides, higher levels of family function (OR, 1.18; 95% CI, 1.04–1.34), social support (OR, 1.02; 95% CI, 1.00–1.04) and resilience (OR, 1.03; 95% CI, 1.01–1.05) were also associated with high QoL. Regarding preparedness for death, both emotional and practical preparedness were significantly associated with high QoL (OR, 1.72 for emotional and 3.86 for practical). Stepwise multivariate analysis identified factors associated with high QoL, including high practical preparedness (OR, 3.66; 95% CI, 2.14–6.25).
| Univariate | P-values | Stepwise multivariate | P-values | |
|---|---|---|---|---|
| OR (95% CI) | Adjusted OR (95% CI) | |||
| FC’s age (per 1-year increase) | 1.04 (1.01–1.06) | 0.006 | 1.04 (1.00–1.07) | 0.042 |
| Female FC | 0.64 (0.31–1.33) | 0.232 | ||
| Non-spouse | 1.12 (0.61–2.07) | 0.717 | ||
| Caregiving days (per 1-d increase) | 0.83 (0.70–0.98) | 0.030 | ||
| Caregiving hours (per 1-h increase) | 0.95 (0.91–0.99) | 0.025 | 0.92 (0.87–0.98) | 0.006 |
| Caregiving months (per 1-m increase) | 0.98 (0.95–1.00) | 0.076 | 0.97 (0.93–1.00) | 0.043 |
| High educational level of FC (college graduate or more) | 1.51 (0.82–2.79) | 0.184 | ||
| Married FC | 2.42 (1.14–5.13) | 0.021 | ||
| No religion of FC | 0.81 (0.44–1.49) | 0.498 | ||
| Functional family function (per 1-point APGAR increase) | 1.18 (1.04–1.34) | 0.007 | ||
| Social support level (per 1-point increase) | 1.02 (1.00–1.04) | 0.036 | ||
| High resilience (1-point increase) | 1.03 (1.01–1.05) | 0.003 | ||
| Well prepared (per 1-point increase) | ||||
| Emotionally | 1.72 (1.23–2.40) | 0.002 | ||
| Practically | 3.86 (2.43–6.12) | <0.001 | 3.66 (2.14–6.25) | <0.001 |
Table presents only significant variables (P<0.05) in multivariate logistic models. FC: Family caregiver, QoL: Quality of life, APGAR: Adaptation, partnership, growth, affection and resolve, OR: Odds ratio, CI: Confidence interval
FC’s QoL by preparedness level
Figure 1 presents the estimated total CQOLC-K scores and each subdomain according to the preparedness level. The preparedness level was categorised as low or high based on the median preparedness score. There were no significant differences in the CQOLC-K scores according to emotional preparedness level, except for the burdensome subdomain (12.3 vs. 18.5; P < 0.001). However, the CQOLC-K scores were significantly higher in the high practical preparedness group than in the low practical preparedness group in the total (62.0 vs. 73.4; P = 0.001) and burdensome subdomain (12.3 vs. 18.3; P < 0.001), but no differences were observed in the scores for the other three subdomains.
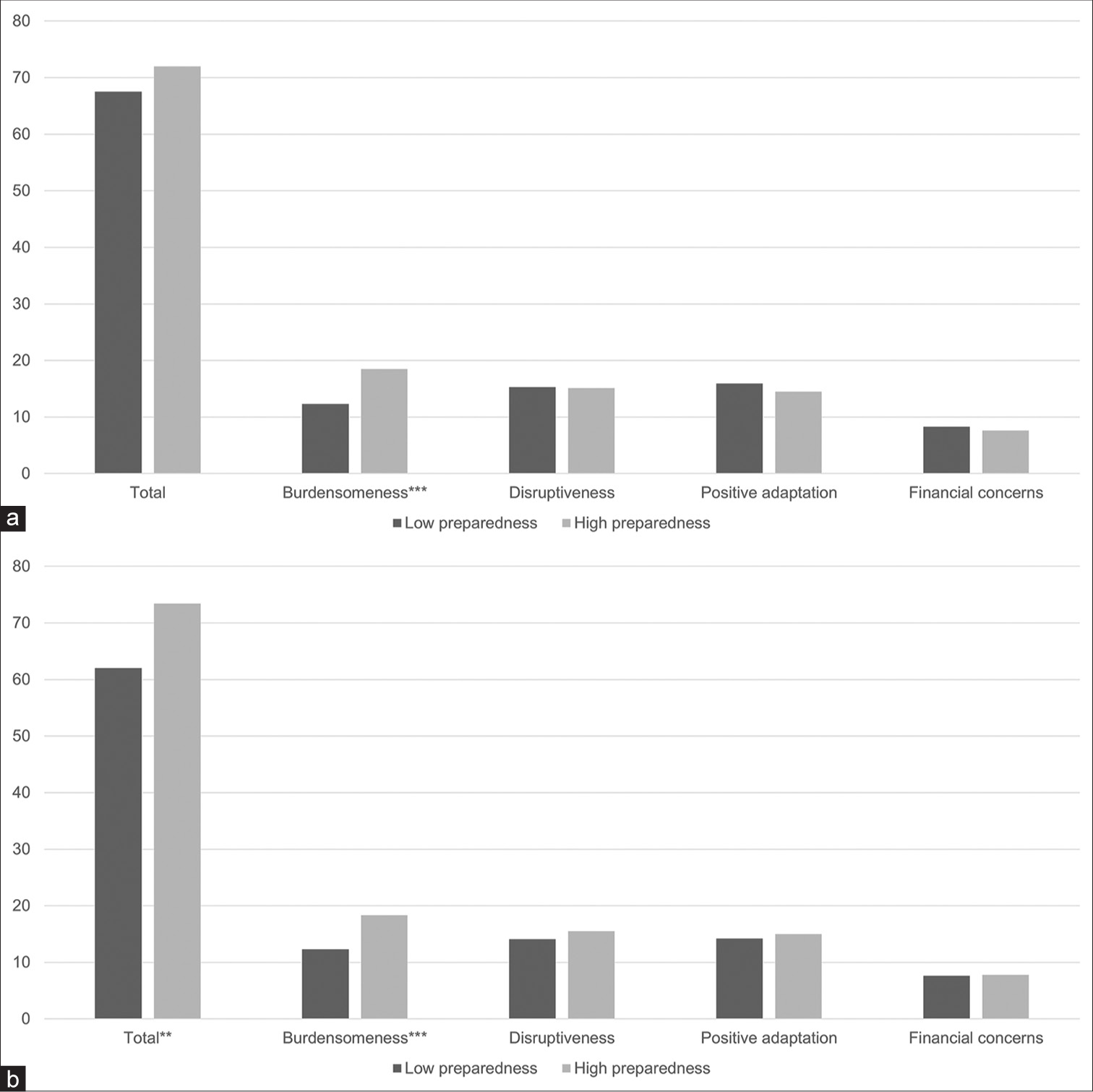
- (a) Emotional preparedness. (b) Practical preparedness. Estimated QoL scores in total and subdomains by preparedness level. Adjusted for all variables in Table 1; By median value of preparedness. **P < 0.01 and ***P < 0.001.
Subgroup analysis for the association between practical preparedness and FC’s QoL
Table 3 shows the regression coefficient (ß) for total QoL scores per 1-point increase in practical preparedness in total and subgroups. Overall, practical preparedness was significantly associated with FC’s QoL (ß, 5.75; 95% CI, 1.86–9.65). Subgroup analyses found several variables that differentiated the significance (i.e., P ≥ 0.05 vs. P < 0.01). The significant association between practical preparedness and FC’s QoL remained robust in groups with low educational levels, low resilience, low social support and dysfunctional families.
| ßb | 95% CI | P-value | |
|---|---|---|---|
| Overall | 5.75 | 1.86–9.65 | 0.004 |
| Attained education level | |||
| High school graduate or less | 9.02 | 3.34–14.71 | 0.002 |
| College graduate or more | 4.93 | −0.73–10.59 | 0.087 |
| Resilience level | |||
| Low (score≤59) | 9.05 | 3.81–14.29 | 0.001 |
| High (score>59) | 3.06 | −2.96–9.08 | 0.313 |
| Social support | |||
| Low (score<75) | 9.23 | 3.47–15.00 | 0.002 |
| High (score≥75) | 3.78 | −1.95–9.50 | 0.192 |
| Family functionality | |||
| Functional (score≥7) | 3.32 | −2.97–9.61 | 0.294 |
| Dysfunctional (score<7) | 10.18 | 4.65–15.71 | <0.001 |
FC: Family caregiver, QoL: Quality of life, CI: Confidence interval. Only variables with a significant difference are presented (i.e., P≥0.05 vs. P<0.01). Regression coefficient for total QoL scores per 1-point increase in practical preparation from multivariate logistic models adjusted for age, sex, relationship to patient, education level, marital status, religiosity, social support, resilience, family functionality, care burdens (hours per day, days per week and caregiving months) and emotional preparedness
DISCUSSION
In this study, practically well-prepared FCs showed higher QoL than poorly prepared FCs, which remained significant in groups with poor psychosocial states. Previous studies have reported several contributing factors associated with FC QoL;[16,20,21] however, studies on preparedness as a factor in FC QoL are relatively rare. A few previous studies have investigated the association between preparedness and FC’s QoL,[22,23] but they were conducted in Taiwan with different measures for preparedness than ours. To the best of our knowledge, this is the first study to evaluate the association between preparedness level and QoL in the FCs of patients with terminal cancer in South Korea. We comprehensively evaluated caregiver and caregiving attributes associated with FC’s QoL, such as religion, family function, social support and resilience and ultimately investigated emotional and practical preparedness as aspects of FC’s QoL.
Preparing for a family member’s death is considered an important component of end-of-life care, not only for family members but also for patients and healthcare providers. Amongst the 26 attributes rated as important at the end of life, four items related to a patient’s death were identified.[24] Regular and transparent communication among patients, family members and healthcare providers enables families to better prepare for death.[25] However, despite the fact that communication with health-care providers about death and dying is one of the most crucial aspects of end-of-life care,[26] the lack of discussion of the patient’s approaching death frequently frustrates family members.[27] In particular, truth-telling has been uncommon in East Asian countries, including Korea, because of traditional Confucianism, which emphasises social ethics rather than spiritual issues and regards death as a taboo. Even unawareness of death has been considered a good death in Korea.[28] The association between preparedness and FC’s QoL observed in our study implies that end-of-life discussions, which contribute to FC’s preparedness for death, can improve FC’s QoL.
The level of preparedness observed in our study was relatively low compared with that in previous studies. In an American study using the same method as ours,[10] the mean scores of emotional and practical preparedness were 3.42 ± 1.5 and 3.67 ± 1.5, respectively. These scores are comparable to those of our high-QoL group (3.4 ± 0.9 for emotional preparedness and 3.6 ± 0.7 for practical preparedness). Since preparedness is linked to cultural beliefs and pre-loss caregiver attributes such as depression, anxiety or financial status,[10] cultural differences and unmeasured caregiver attributes may affect the differences in preparedness levels. In addition, according to a cross-cultural study conducted amongst palliative care physicians in East Asian countries,[29] 59% of Korean FCs are reluctant to engage in end-of-life discussions with physicians. We believe that the reluctance to engage in end-of-life conversations originating from death as a taboo is one of the most plausible reasons for low preparedness in Korea.
In our study, the FC’s overall QoL was significantly related to practical preparedness, not to emotional preparedness, which was consistent with a previous finding.[23] Practical adaptation to the loss could be as vital as an emotional one, according to the ‘dual process model’ proposed by Stroebe and Schut.[30] During the pre-loss phase as well, to some FCs, practical uncertainty could be more distressing than the psychosocial aspects.[31] In addition, significant differences were observed only in the burdensome domain, but the explanation for these remains unclear. Further studies are needed to elucidate the mechanisms by which different QoL domains are associated with preparedness.
Our subgroup analyses revealed that the association between practical preparedness and QoL was prominent in FCs with lower education, low resilience, low social support and dysfunctional families. This suggests that the relative contribution of practical preparedness to QoL is greater in the psychosocially poor group. These results increase the robustness of understanding of the intricacy of the process of preparing for death and the importance of preparedness assessment according to FC’s attributes and caregiving environment.
Caregiver preparedness for death can be assessed using a multidimensional approach. Carr suggested that preparedness can be approached as emotional and practical dimensions,[11] which we used to assess preparedness for death in this study. Previous studies have assessed emotional and practical preparedness with each single question, ‘How prepared do you think you are for the death of the patient emotionally (or practically)’?[10] Other research groups have suggested the multidimensional nature of preparedness as medical, psychosocial, spiritual and practical dimensions[32] or as cognitive, affective and behavioural aspects.[31] In a recent study,[33] researchers suggested a preliminary framework for FC preparedness based on establishing both present and future certainties. However, a consensus regarding the best preparedness assessment has not been reached.[33]
In the current study, besides practical preparedness for death, other factors associated with FCs’ QoL were identified (i.e., FC’s age and objective care burden), which were consistent with previous results.[34] Increased daily time spent on caregiving was a significant predictor of QoL,[35] and caregiving duration also showed a significant impact on the QoL and supportive care needs.[36] Caregivers who devote the majority of their time to the patient may struggle to find time for themselves, making it challenging to manage other obligations, including financial burden, which negatively affects their overall QoL.[35] Therefore, it is important for family members to share and divide caregiving time, and further, supporting programmes or services are needed to lessen the time spent on patient care.
This study had several limitations. First, we could not establish a causal relationship between preparedness level and QoL because of the cross-sectional study design. In addition, preparedness can change and vary at different caregiving points.[31] Longitudinal and interventional studies are required to confirm the relationship between preparedness and QoL. Second, since preparedness can be affected by various factors such as caregivers’ emotional symptoms, daily living competencies or financial status,[10] these unmeasured covariates might have influenced the results. Third, the results observed in this study cannot be generalised to other populations because it was conducted with Korean FCs of patients with terminal cancer in inpatient palliative care units. Finally, the validity of the Korean version of death preparedness was not formally tested. To address this, we conducted a brief translating process: Two bilingual doctors first translated the questionnaire and reached a consensus and then a pilot test was performed with 13 samples (i.e., doctor, nurse, social worker, patient and caregiver), who provided feedback.
CONCLUSION
Amongst Korean FCs of patients with terminal cancer, QoL was significantly linked to practical preparedness for death, not to emotional preparedness. Our findings warrant the personalised assessment to evaluate each FC’s needs and preparedness levels. Moreover, to enhance FCs’ QoL during the end of life, specific palliative care services to help FCs prepare the death practically are needed through developing programmes and intervention studies.
Ethical approval
The research/study was approved by the Institutional Review Board at Veterans Health Service Medical Center; International St. Mary’s Hospital; Gachon University Gil Medical Center; Ilsan Hospital; Daegu Dongsan Hospital; Eunpywong St. Mary Hospital/Incheon St. Mary Hospital; Korea University Guro Hospital; National Cancer Center, number BOHUN2021-07-007-001; 21IRB064; GDIRB2021-283; NHIMC2022-05-003-003; DDH21-009D; CIRB-20210928-001; 2021GR0396; NCC2021-0231, dated various.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: This work was supported by Gachon University Gil Medical Center (No. FRD2021-14).
References
- Quality of Life in Caregivers of Cancer Patients: A Literature Review. Int J Environ Res Public Health. 2023;20:1570.
- [CrossRef] [Google Scholar]
- Informal Caregiver Burden for Solid Tumour Cancer Patients: A Review and Future Directions. Psychol Health. 2021;36:1514-35.
- [CrossRef] [Google Scholar]
- Family Caregivers' Involvement in Caring with Cancer and their Quality of Life. Asian Pac J Cancer Prev. 2019;20:1735-41.
- [CrossRef] [Google Scholar]
- Reciprocal Suffering: The Need to Improve Family Caregivers' Quality of Life through Palliative Care. J Palliat Med. 1998;1:357-66.
- [CrossRef] [Google Scholar]
- Quality of Life in Patients with Breast Cancer: The Influence of Family Caregiver's Burden and the Mediation of Patient's Anxiety and Depression. J Nerv Ment Dis. 2019;207:921-6.
- [CrossRef] [Google Scholar]
- NCCN Guidelines® Insights: Palliative Care, Version 2. 2021. J Natl Compr Canc Netw. 2021;19:780-8.
- [CrossRef] [Google Scholar]
- Quality of Life of Family Caregivers of Cancer Survivors: Across the Trajectory of the Illness. Cancer. 2008;112:2556-68.
- [CrossRef] [Google Scholar]
- Quality of Life and Mental Health in Caregivers of Outpatients with Advanced Cancer. Psychooncology. 2013;22:403-10.
- [CrossRef] [Google Scholar]
- Cancer Caregivers' Preparedness for Loss and Bereavement Outcomes: Do Preloss Caregiver Attributes Matter? Omega (Westport). 2019;80:224-44.
- [CrossRef] [Google Scholar]
- Death and Dying in the Contemporary United States: What are the Psychological Implications of Anticipated Death? Soc Person Psychol Compass. 2012;6:184-95.
- [CrossRef] [Google Scholar]
- Pre-loss Grief and Preparedness for Death among Caregivers of Terminally Ill Cancer Patients: A Systematic Review. Soc Sci Med. 2021;284:114240.
- [CrossRef] [Google Scholar]
- Long-term Harm of Low Preparedness for a Wife's Death from Cancer--A Population-based Study of Widowers 4-5 Years after the Loss. Am J Epidemiol. 2010;172:389-96.
- [CrossRef] [Google Scholar]
- Does Ethnicity Matter-Cultural Factors Underlying Older Adults' End-of-life Care Preferences: A Systematic Review. Geriatr Nurs. 2020;41:89-97.
- [CrossRef] [Google Scholar]
- Korean Version of the Caregiver Quality of Life Index-Cancer (CQOLC-K) Qual Life Res. 2005;14:899-904.
- [CrossRef] [Google Scholar]
- Factors Associated with Quality of Life Among Family Caregivers of Terminally Ill Cancer Patients. Psychooncology. 2016;25:217-24.
- [CrossRef] [Google Scholar]
- Development of a New Resilience Scale: The Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18:76-82.
- [CrossRef] [Google Scholar]
- Reliability, Validity, and Item Response of MOS Social Support Score among Incarcerated Women. Women Crim Justice. 2014;24:1-21.
- [CrossRef] [Google Scholar]
- The Family APGAR: A Proposal for a Family Function Test and Its Use by Physicians. J Fam Pract. 1978;6:1231-9.
- [CrossRef] [Google Scholar]
- The Factors Associated with the Quality of Life of the Spouse Caregivers of Patients with Cancer: A Cross-sectional Study. J Palliat Med. 2012;15:216-24.
- [CrossRef] [Google Scholar]
- Hospice Family Caregivers' Quality of Life. J Clin Nurs. 2009;18:2563-72.
- [CrossRef] [Google Scholar]
- Course of Changes in Emotional Preparedness for Death and Its Associations with Caregiving Outcomes for Family Caregivers of Terminally Ill Cancer Patients Over Their Last Year of Life. J Pain Symptom Manage. 2021;61:974-82.
- [CrossRef] [Google Scholar]
- Caregivers' Death-Preparedness States Impact Caregiving Outcomes and Patients' Endof-Life Care. J Pain Symptom Manage. 2022;63:199-209.
- [CrossRef] [Google Scholar]
- Factors Considered Important at the End of Life by Patients, Family, Physicians, and Other Care Providers. JAMA. 2000;284:2476-82.
- [CrossRef] [Google Scholar]
- Family Perspectives on Dying in Long-term Care Settings. J Gerontol Nurs. 1999;25:19-25.
- [CrossRef] [Google Scholar]
- Prognosis Communication in Serious Illness: Perceptions of Older Patients, Caregivers, and Clinicians. J Am Geriatr Soc. 2003;51:1398-403.
- [CrossRef] [Google Scholar]
- Communication in Cancer Care in Asia: A Narrative Review. JCO Glob Oncol. 2023;9:e2200266.
- [CrossRef] [Google Scholar]
- A Cross-Cultural Study on Behaviors When Death Is Approaching in East Asian Countries: What Are the Physician-Perceived Common Beliefs and Practices? Medicine (Baltimore). 2015;94:e1573.
- [CrossRef] [Google Scholar]
- The Dual Process Model of Coping with Bereavement: Rationale and Description. Death Stud. 1999;23:197-224.
- [CrossRef] [Google Scholar]
- Preparing Family Caregivers for Death and Bereavement. Insights from Caregivers of Terminally Ill Patients. J Pain Symptom Manage. 2009;37:3-12.
- [CrossRef] [Google Scholar]
- Preparing Caregivers for the Death of a Loved One: A Theoretical Framework and Suggestions for Future Research. J Palliat Med. 2006;9:1164-71.
- [CrossRef] [Google Scholar]
- Preparedness for the Death of an Elderly Family Member: A possible Protective Factor for Pre-loss Grief in Informal Caregivers. Arch Gerontol Geriatr. 2021;94:104353.
- [CrossRef] [Google Scholar]
- Impact of Informal Cancer Caregiving Across the Cancer Experience: A Systematic Literature Review of Quality of Life. Palliat Support Care. 2020;18:220-40.
- [CrossRef] [Google Scholar]
- Quality of Life of Caregivers of Women Receiving Cancer Treatment in Turkey. Florence Nightingale J Nurs. 2023;31:S31-7.
- [CrossRef] [Google Scholar]
- Quality of Life vs. Supportive Care Needs for Oral Cancer Caregivers: Are They Related? Curr Oncol. 2023;30:1733-44.
- [CrossRef] [Google Scholar]







