Translate this page into:
Unmet Palliative Care Needs of Patients with Stage B Chronic Heart Failure Classified by the American Heart Association/American College of Cardiology
*Corresponding author: Ryo Matsunuma, Department of Palliative Medicine, Kobe University Graduate School of Medicine, Kobe, Japan. manutsuma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Matsunuma R, Yamaguchi T, Matsumoto K, Sakashita A, Hashiguchi C, Iida M, et al. Unmet Palliative Care Needs of Patients with Stage B Chronic Heart Failure Classified by the American Heart Association/American College of Cardiology. Indian J Palliat Care. 2024;30:384-7. doi: 10.25259/IJPC_37_2023
Abstract
This study sought to explore the unmet palliative care needs of patients diagnosed with Stage B chronic heart failure (CHF) according to the American Heart Association (AHA) and American College of Cardiology (ACC) classifications. We conducted this cross-sectional study between June 1 and August 31, 2020, at Kobe University Hospital. Patients were asked to complete the Integrated Palliative care Outcome Scale (IPOS) along with a customized questionnaire developed by a multidisciplinary team. These tools were filled out by the patients themselves or with help from family members. A total of 101 patients participated in the study, with 55 of them (55%) falling into the Stage B CHF group as classified by AHA/ACC. Among the physical symptoms, 22% reported dyspnea and 20% reported drowsiness as common concerns. Regarding specific problems, 47% identified issues related to exercise, 62% with eating, 26% with finances, and 18% with employment. Notably, financial difficulties were found to be significantly more common among Stage B patients when compared to those in Stages C and D (odds ratio [OR]: 5.22; 95% confidence interval [95% CI]: 1.03–26.5; p = 0.032). Almost 79% of Stage B patients expressed a desire to understand the progression of their disease. In conclusion, stage B CHF patients may face financial difficulties and have unmet informational needs. Therefore, further research is necessary to explore these aspects in greater detail.
Keywords
Chronic heart failure
Palliative care needs
Financial problems
Informational needs
INTRODUCTION
Chronic heart failure (CHF) is a significant global cause of mortality.[1] According to the World Health Organization, cardiovascular diseases, due to their high prevalence and the severe suffering they cause, necessitate palliative care.[2] Numerous studies suggest that early integration of palliative care, especially through a symptom-based needs assessment, is beneficial in managing cardiac conditions.[3,4] However, research on palliative care needs has primarily focused on patients in American Heart Association (AHA)/American College of Cardiology (ACC) Stages C and D, leaving a gap in understanding for those in Stage B CHF according to AHA/ACC classifications. To ensure effective early-stage interventions, it is critical to comprehend the palliative care needs of Stage B CHF patients. Therefore, this study focuses on identifying these unmet needs.
MATERIALS AND METHODS
This study involves a secondary analysis of research that previously examined palliative care needs amongst outpatients with CHF in Japan.[5] Participants were recruited based on the following criteria: (1) A confirmed CHF diagnosis by a cardiologist, (2) regular attendance at the heart failure clinic of Kobe University Hospital, (3) age 20 or older, (4) outpatient status and (5) written informed consent. Exclusion criteria included the inability to communicate in Japanese, deteriorating health conditions as determined by a cardiologist, severe depression or anxiety and cognitive impairment preventing questionnaire completion. Patients with severe depression and anxiety were excluded because the questionnaire included questions on end-of-life (EOL) considerations that could potentially exacerbate their mental health symptoms.
Patients completed the Integrated Palliative Care Outcome Scale (IPOS) and an original questionnaire (supplement) developed by an interdisciplinary team including a palliative care physician, cardiologist, palliative care nurse, palliative care specialist and heart failure nurse specialists. An additional original questionnaire was developed through extensive consultations amongst experts, with the objective of investigating palliative care needs not encompassed by the IPOS, specifically focusing on illness understanding, information needs and daily practical requirements. The custom questionnaire contained 13 items addressing specific issues,[6] comprehension of the name of the patient’s disease;[7] treatment currently received; patients’ knowledge of the expected course of disease; willingness to know the expected course of disease; experience with thinking and discussion surrounding treatment or care if patients could not speak and communicate their intentions at the EOL; willingness to discuss treatment or care if they lost decision-making capacity due to an advanced medical condition; acceptable and unacceptable treatment and care if patients could not speak and communicate their intentions at the EOL[8] and what was important to patients if their lifetime was limited due to disease progression. The two questions regarding patients’ understanding and desire to know the anticipated progression of their disease were classified as 1 = definitely and 2 = mostly, with other responses grouped separately. Questions assessing the level of experience with EOL discussions were categorised as 1 = thoroughly discussed, 2 = somewhat discussed and others. Responses concerning patients’ willingness to discuss the type of EOL treatment or care they wished to receive were categorised as 1 = very much and 2 = a little, with other responses in a separate category. The patients answered either independently or with family assistance, and a cardiologist collected both oral and written informed consent.
To compare heart failure severity, patients were divided into two groups: Those with AHA/ACC Stage B and those with Stages C and D. Continuous variables were analysed using Student’s t-test, while categorical variables were assessed using the Chi-squared test. The Statistical Package for the Social Science software (version 26.0; IBM, Tokyo, Japan) was used for the statistical analyses, and a two-tailed P-value of <0.05 was considered statistically significant. The study was conducted following ethical standards as outlined by the Declaration of Helsinki and approved by Kobe University’s ethics committee (approval no. B200046).
RESULTS
We recruited 101 patients [Table 1]. Of these, patients classified as Stage A (n = 0), Stage B (n = 55, 55%), Stage C (n = 43, 43%) and Stage D (n = 3, 3%) CHF according to AHA/ACC were included. Patients with Stage B CHF were significantly younger than those with Stages C and D (60 vs. 72 years, P< 0.001). According to the IPOS, dyspnoea (22%) and drowsiness (20%) were the most frequently reported physical symptoms. Insomnia (25%) was the most frequent psychological symptom in Stage B CHF patients. Regarding specific problems, exercise (47%), eating (62%), finance (26%) and work (18%) were selected most frequently by Stage B CHF patients. In particular, finance was reported as a significantly more frequent problem in Stage B CHF patients compared with patients with Stages C and D CHF (odds ratio: 5.22; 95% confidence interval: 1.03–26.5; P = 0.032). About 22% of patients with Stage B CHF clearly understood the prospects of their disease. Amongst those who did not understand their disease prospects, 79% of patients with Stage B CHF expressed a willingness to understand the expected course of their disease. Approximately 37% of patients with Stage B CHF reported experience with consideration and discussion of the treatment or care if they could not speak and communicate their intention in the EOL, while 71% of patients were willing to discuss treatment or care. These perspectives did not significantly differ between Stages B and C/D.
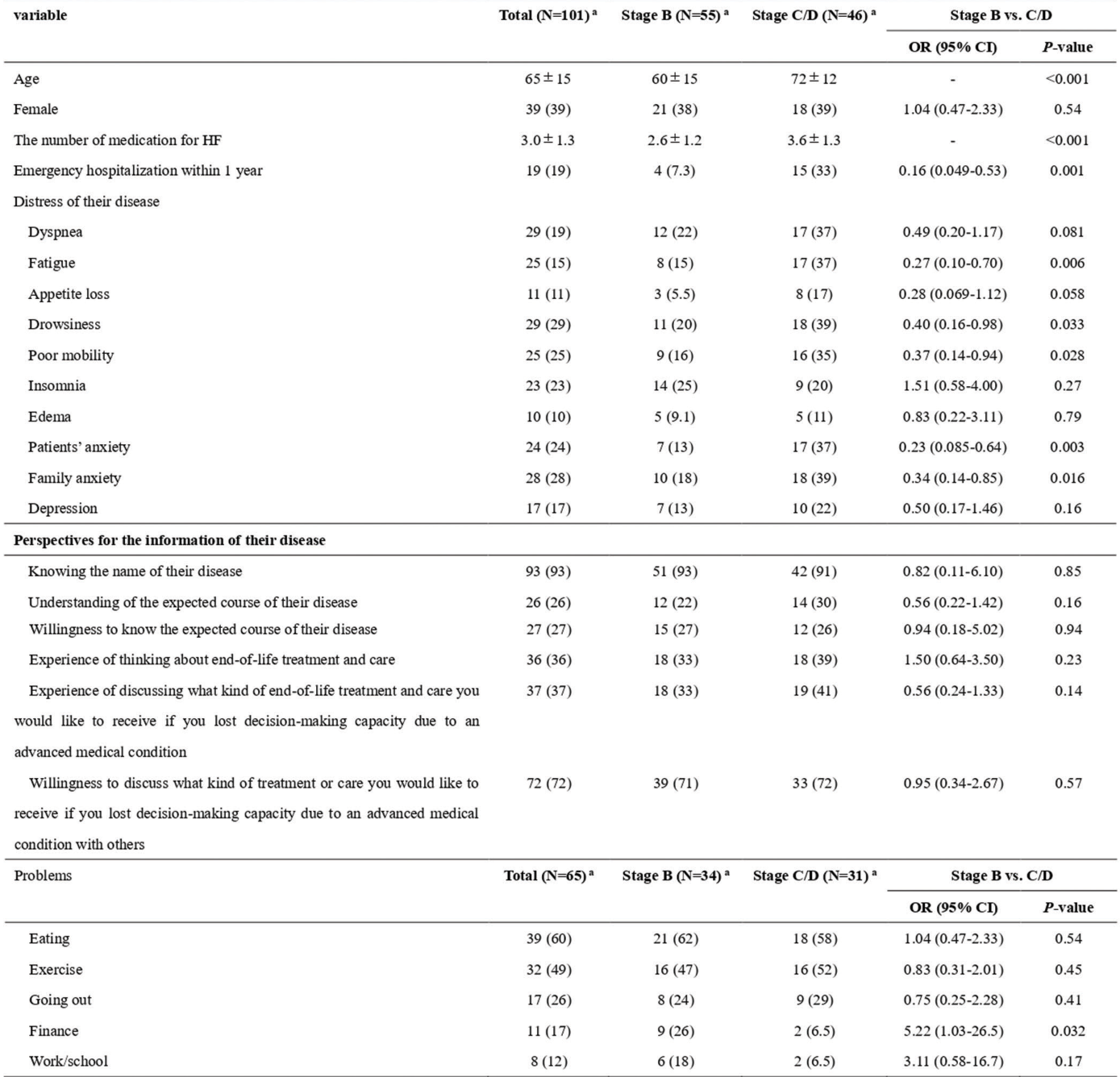 |
HF: Heart failure, C/D means stage C and D, an(%), CI: Confidence interval, IPOS: Integrated Palliative Care Outcome Scale, NYHA: New York Heart Association, OR: Odds ratio, N/A: Not analysed
DISCUSSION
Our results revealed that financial burden was an unmet palliative care need for patients with Stage B CHF. Although specific details of financial problems were not identified, employment-related problems tended to be more frequent (although not statistically significant) in patients with Stage B CHF than in those with Stages C and D in our study. Rorth et al., also reported that 25% of patients with heart failure could not return to the workforce after the first episode of emergency admission.[9] Other reasons for the increased financial burden for patients with CHF and their families reported in previous studies include out-of-pocket expenses, childcare demands and caregiving hours.[10] As Stage B patients were younger than Stage C and D patients in this study, they were more likely to be active members of the workforce and have childcare responsibilities. Thus, Stage B patients might consider themselves to be more affected by financial problems. Another study stated that financial toxicity is a barrier for patients with CHF when making decisions about necessary interventions.[11] However, there are no studies on the nature of financial problems faced by patients with Stage B CHF. Therefore, further studies must be conducted to better understand the actual reasons for the economic burden on patients with Stage B CHF and gain more insight into the impact of their financial issues. Moreover, strategies for healthcare providers to address these concerns should be investigated.
In our study, 80% of patients who did not fully comprehend the progression of their disease indicated a willingness to learn more. Having a clear understanding of their disease trajectory is crucial for patients facing incurable conditions to engage in advance care planning (ACP), including making decisions about future medical care.[7] The European Association for Palliative Care recommends that timely ACP, conducted when patients can still actively participate in the decision-making process, should be a routine part of clinical care. ACP should not be delayed until patients are in the final stages of their illness.[2] However, clinicians caring for patients with CHF have reported several barriers to discussing disease trajectory and EOL care.[8] Nevertheless, our study suggests that clinicians should proceed with these discussions, as a high proportion of patients indicated that they wanted this information.
Insomnia is prevalent in patients with heart failure. While it is possible that insomnia may be associated with physical symptoms, including heart failure, the specific causes of insomnia were not explored in this research. However, further studies are required to investigate this issue.
CONCLUSION
This study revealed that patients with Stage B CHF may have problems regarding financial or informational needs. As our study has a small sample size and is cross-sectional, further studies must be conducted to identify the actual reasons for these problems in patients with Stage B CHF and the impact of these issues. Moreover, strategies for healthcare providers to address these concerns should be investigated.
Ethical approval
The research/study was approved by the Institutional Review Board at Kobe University’s ethics committee, number B200046, dated 26 May 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Financial support and sponsorship
This trial was supported by a Grant-in-Aid for Young Scientists from the Japan Society for the Promotion of Science (grant number 20K16520).
References
- Epidemiology of Heart Failure. Eur J Heart Fail. 2020;22:1342-56.
- [CrossRef] [PubMed] [Google Scholar]
- Global Atlas of Palliative Care at the End of Life. 2014. :111. Available from: http://www.who.int/cancer/publications/palliative-care-atlas/en [Last accessed on 2023 Feb 03]
- [Google Scholar]
- Palliative Care for People Living with Heart Failure: European Association for Palliative Care Task Force Expert Position Statement. Cardiovasc Res. 2020;116:12-27.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Practice Guidelines for Quality Palliative Care (4th edition). Richmond: National Coalition for Hospice and Palliative Care; 2018. Available from: https://www.nationalcoalitionhpc.org/ncp [Last accessed on 2023 Feb 03]
- [Google Scholar]
- Comprehensive Palliative Care Needs in Outpatients with Chronic Heart Failure: A Japanese Cross-Sectional Study. Palliat Med Rep. 2022;3:65-74.
- [CrossRef] [PubMed] [Google Scholar]
- Meeting the Communication and Information Needs of Chronic Heart Failure Patients. J Pain Symptom Manage. 2008;36:149-56.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between Understanding of Current Treatment Intent, Communication with Healthcare Providers, Preferences for Invasive Life-sustaining Interventions and Decisional Conflict: Results from a Survey of Patients with Advanced Heart Failure in Singapore. BMJ Open. 2018;8:e021688.
- [CrossRef] [PubMed] [Google Scholar]
- Return to the Workforce after First Hospitalization for Heart Failure: A Danish Nationwide Cohort Study. Circulation. 2016;134:999-1009.
- [CrossRef] [PubMed] [Google Scholar]
- Financial Burdens and Mental Health Needs in Families of Children with Congenital Heart Disease. Congenit Heart Dis. 2018;13:554-62.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to Goals of Care Discussions With Patients Who Have Advanced Heart Failure: Results of a Multicenter Survey of Hospital-Based Cardiology Clinicians. J Card Fail. 2017;23:786-93.
- [CrossRef] [PubMed] [Google Scholar]







