Translate this page into:
A Descriptive Study to Assess the Knowledge, Attitude, Practices, Perceived Barriers, and Support Regarding Palliative Care and End-of-Life Care among Critical Care Nurses of Tertiary Care Medical Institute
Address for correspondence: Dr. Rakesh Garg, Room No. 139, Fist Floor, Department of Onco-Anaesthesia and Palliative Medicine, Dr. BRAIRCH, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029, India. E-mail: drrgarg@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
The role of nurses working in critical care setup is one of the key members for optimal provision of the palliative care and end-of-life care (EOLC). This study aims to assess knowledge, attitude, practices, and perceived barriers regarding palliative and EOLC among critical care nurses.
Methods:
A cross-sectional study was conducted among 386 critical care nurses of a tertiary care center, selected through convenience sampling technique. Data related to knowledge, attitude, practices, and perceived barriers were collected using a standardized tool. The collected data were analyzed using SPSS version 24.
Results:
We observed that mean knowledge, attitude, and practice scores of critical care nurses were 9.83 ± 2.50 of 20, 104.91 ± 13.04 of 150, and 17.61 ± 4.36 of 27, respectively. One of the major barriers in providing palliative and EOLC was being called for attending to other newly admitted patients. The mean knowledge score of nurses was found to be significantly higher among female nurses (P = 0.016). Nurses who had additional training pertaining to palliative and EOLC had significantly higher mean knowledge (P = 0.001) and attitude scores (P = 0.02) than those who did not have such training. The mean practice (P = 0.02) and attitude score (P = 0.002) was significantly higher among postgraduate nurses as compared to nurses with lower qualification. The mean attitude score was significantly higher among nurses of lower age group (P = 0.04) along with a negative correlation of age of nurses with attitude (P = 0.01). Nurses' practice was positively correlated to the attitude (P = 0.001) and knowledge (P = 0.01).
Conclusion:
There is a considerable gap between critical care nurses' knowledge and practices, in spite of having a good attitude regarding palliative and EOLC. This necessitates the strengthening of both preservice and in-service education for nurses.
Keywords
Attitude
barriers
critical care nurses
end-of-life care
knowledge
palliative care
practices
INTRODUCTION
According to the World Health Organization, “Palliative care is an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems; physical, psychosocial and spiritual.”[1] End-of-life care (EOLC) may be defined as “the active, total care of patients who are unresponsive to curative treatment.”[2] There is a working culture among health-care workers due to which center of interest is on cure and purposefully or accidentally, the vast majority of them maintain a distance from the dying patient.[3] The role of nurses in the provision of palliative and EOLC is determined by their interest, willingness, attitude, and rapport with the patient and family members.[4]
The role of critical care nurses in overall management of critically ill patients is paramount and irrefutable. The involvement of nurses in critical decision-making along with adequate training in palliative and EOLC needs to be emphasized.[4567] However, there are not sufficient data from critical care nursing personnel with regard to the understanding of palliative and EOLC.
The objectives of the study were to assess the knowledge, attitude, practice, perceived barriers, and support regarding palliative and EOLC among critical care nurses. This will be helpful in understanding a portion of the sufficiency as well as deficiencies among critical care nurses in regard to various aspects of palliative and EOLC. The secondary objective of this study was to determine the association of knowledge, attitude, and practices regarding palliative and EOLC with the selected variables.
METHODS
This descriptive cross-sectional study was carried out at critical care units of a tertiary care teaching Institute after institutional ethical committee approval vide Ref. No. IECPG-43/28.02.18. The critical care nurses, who were registered nurses and working in critical care units for at least 1 year, were enrolled for the study and written informed consent was obtained to participate in the study.
Data collection tools
Data related to demography and study parameters were assessed and recorded using the following tools [Appendix]:
Tool I
It consisted of demographic datasheet.
Tool II
Self-administered knowledge assessment questionnaire: It was developed by the researcher based on a review of the literature and validated by experts for its content, face, construct, and criteria (r = 0.88). It included 20 multiple choice questions with four options each. The areas covered were philosophy and meaning of palliative and EOLC, patient assessment, management of airway, breathing, pain, constipation, delirium, oral health, death, and loss. Each question was scored, as 1 score will be given for correct answer and 0 score for incorrect/unanswered answer. Knowledge was categorized as per the review of literature as poor <10 scores (<50% of total score), satisfactory 10–13 scores (50%–65% of total score), good 14–17 scores (66%–85% of total score), and excellent >17 scores (>85% of total score).[12367]
Tool III
Frommelt Attitude toward Care of the Dying[8] Scale for attitude is 30-item standardized tool with 5-point Likert scale to indicate respondents' attitudes toward caring for dying patients. It includes 15 positively and 15 negatively worded statements with response options: strongly disagree (1), disagree (2), uncertain (3), agree (4), and strongly agree (5). Possible scores ranged from 30 to 150. Attitude scores were categorized, as per the review of literature, as favorable ≥90 scores (>60% of total score) and unfavorable <90 scores (≤60% of total score).[12367]
Tool IV
Self-reported practice checklist: It was developed by the researcher based on a review of the literature and validated by experts for its content, face, construct, and criteria (r = 0.94). It included 10 items with subitems (with a total of 27 items) and scored as 0 for no and 1 for yes. Maximum scores were 27. The practice was categorized by the researcher as per the review of literature, as satisfactory >20 marks (>75% of total score) and poor ≤20 marks (≤75% of total score).[12367]
Tool V
It consisted of self-administered scale for perceived barriers and open-ended questionnaire for perceived support.[2] This is a 3-point Likert scale with response options: not at all, some extent, and large extent. It contained four main items – environmental factor, family related factors, knowledge and skill, and treatment policy with subitems. Two open-ended (optional) questions were to measure perceived support for critical care nurses [Appendix].
The various data shall be summarized and correlation shall be statistically sought for various demographic parameters and study parameters with regard to attitude knowledge and practice.
Statistical analysis
The sample size was calculated based on data obtained from a pilot study among 40 nurses. Based on the estimated prevalence of knowledge as 50%, with margin of error as 5% and confidence interval 95%, 386 critical care nurses were enrolled for the study. Collected data were coded and entered into Microsoft Excel 2010 spreadsheet and checked for errors. SPSS (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.) was used for descriptive and inferential statistical analysis (independent t-test [for two groups, i.e., gender, marital status, and additional qualification pertaining to palliative care and EOLC] and ANOVA [for more than two groups, i.e., age, qualification, and experience in critical care units and working critical care units]) to find frequencies, percentage, and mean of variables under the study. The level of significance was set up as P ≤ 0.05.
RESULTS
Of 400 nurses, 386 critical care nurses were recruited for the study and were analyzed for the outcome parameters, as the rest did not meet the inclusion/exclusion criteria [Figure 1].
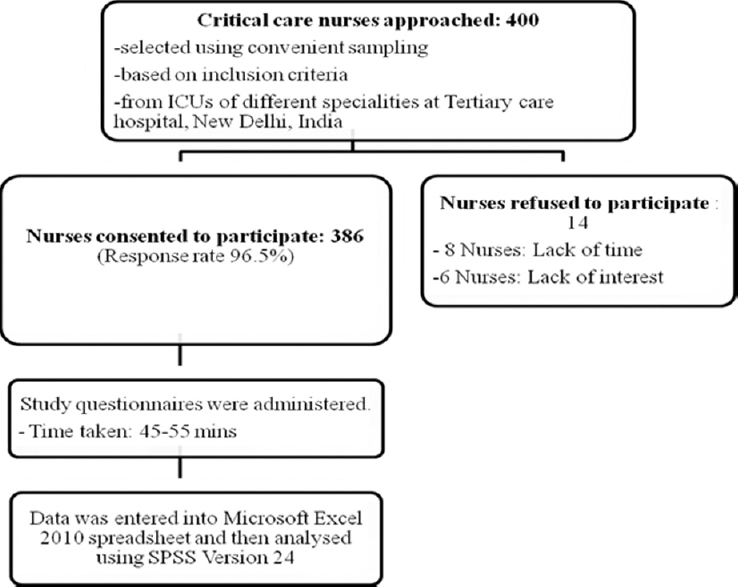
- Flow diagram of data collection procedure
The demographic profile revealed that majority nurses were females, married, graduates, and >2 years of experience in critical care units [Table 1].
| Demographic variables | n (%) |
|---|---|
| Age (years) | |
| 21-30 | 179 (46.4) |
| 31-40 | 200 (51.8) |
| >40 | 7 (1.8) |
| Gender | |
| Male | 172 (44.6) |
| Female | 214 (55.4) |
| Qualification | |
| General nursing and midwifery | 95 (24.6) |
| Postbasic nursing | 70 (18.1) |
| BSc Nursing | 201 (52.1) |
| MSc Nursing | 20 (5.2) |
| Marital status | |
| Unmarried | 77 (19.9) |
| Married | 309 (80.1) |
| Experience in critical care unit (months) | |
| 12-24 | 79 (20.5) |
| 25-36 | 66 (17.1) |
| 37-48 | 21 (5.4) |
| >48 | 220 (57) |
| Additional training in palliative care | |
| Yes | 224 (58) |
| No | 162 (42) |
| Type of critical care unit | |
| Medical and surgical | 101 (26.2) |
| Cardiology and cardiothoracic | 200 (51.8) |
| Neurology and neurosurgical | 85 (22) |
Knowledge, attitude, and practice scores regarding palliative and end-of-life care (n = 386)
The mean knowledge score was 9.83 ± 2.50 where 51.6% of the nurses had satisfactory knowledge, 41.4% had poor knowledge, and 7% had good knowledge regarding palliative and EOLC. The mean attitude score of nurses was 104.91 ± 13.04 where 88.1% of the nurses had a favorable attitude and 11.9% of the nurses had an unfavorable attitude toward palliative and EOLC. The mean practice score of nurses was 17.61 ± 4.36, with 63.5% of the nurses having poor practices, whereas only 36.5% of the nurses had satisfactory practices regarding palliative and EOLC.
Table 2 shows that various perceived barriers were reported by critical nurses. Out of that, minimal (4.9%) number of nurses reported that workload is not a barrier in providing palliative and EOLC. Family members do not accept patient's poor prognosis (88.6%), difference in physician's opinion about treatment (84.7%), nurses being continually called for information (83.6%), and family members do not understand the meaning of lifesaving (82.6%) are some of the barriers reported by critical care nurses [Tables 2 and 3].
| Items | Perceived as a barrier | ||
|---|---|---|---|
| Not at all, n (%) | To some extent, n (%) | To a large extent, n (%) | |
| Environmental factors | |||
| Nurses workload | 19 (4.9) | 188 (48.7) | 179 (46.4) |
| Lack of privacy in critical care unit design | 112 (29) | 212 (54.9) | 62 (16.1) |
| Liberal visiting hours | 110 (28.5) | 205 (53.1) | 71 (18.4) |
| Restrictive visiting hours | 174 (45.1) | 154 (39.9) | 58 (15) |
| Lack of available resources | 91 (23.6) | 190 (49.2) | 105 (27.2) |
| Family members | |||
| Not understanding meaning of lifesaving | 67 (17.4) | 239 (61.9) | 80 (20.7) |
| Continually calling for information | 63 (16.3) | 226 (58.5) | 97 (25.1) |
| Fighting about life support use | 86 (22.3) | 235 (60.9) | 65 (16.8) |
| Not accepting patient poor prognosis | 44 (11.4) | 223 (57.8) | 119 (30.8) |
| Not present when patient dies | 105 (27.2) | 160 (41.5) | 121 (31.3) |
| Nurses knowledge and skills | |||
| Lack of nursing education and training | 115 (29.8) | 172 (44.6) | 99 (25.6) |
| Not knowing patients’ wishes | 121 (31.3) | 182 (47.2) | 83 (21.5) |
| Treatment policy | |||
| Not considering nurses’ opinion | 102 (26.4) | 191 (49.5) | 93 (24.1) |
| Being called to help with newly admitting patients | 79 (20.5) | 238 (61.7) | 69 (17.9) |
| Difference in physicians’ opinion about treatment | 59 (15.3) | 217 (56.2) | 110 (28.5) |
| Nurse (n=1): There should be adequate infusion pump at least (4 per patient) in an ICU with proper functioning ventilators and bedside monitors |
| Nurse (n=2): Provision of free or subsidized accommodation and provision of food for patient’s close members (for at least 1 or 2) if patient stays at hospital or healthcare setting |
| Nurse (n=3): Nurses should also be involved in discussions during doctors rounds |
| Nurses (n=266): There should be in-service training for critical care nurses regarding palliative and EOLC |
| Nurses (n=299): There should be good communication among doctors and nurses so that care can be provided effectively |
| Nurses (n=320): Palliative and EOLC should be provided by the same nurse to maintain continuity of care |
| Nurses (n=316): Family members should be involved in patient’s palliative and EOLC |
EOLC: End-of-life care, ICU: Intensive care unit
The association among the studied parameters was analyzed [Table 4]. It revealed that the younger age group had a statistically higher mean attitude score. Female nurses had more mean knowledge score than the male nurses. The mean knowledge as well as the practice score of nurses who had additional training was statistically higher than those who had not additional training. Postgraduate nurses had statistically higher practice as well as attitude mean scores than other lower qualification group. Nurses working in neurology/neurosurgical critical care units had statistically higher mean attitude score.
| Demographic variables | Frequency (n) | Mean±SD | ||
|---|---|---|---|---|
| Knowledge score | Attitude score | Practice score | ||
| Age (years) | ||||
| 21-30 | 179 | 17.45±3.85 | 106.47±14.64 | 9.97±2.32 |
| 31-40 | 200 | 17.76±4.78 | 103.79±10.65 | 9.72±2.63 |
| >40 | 7 | 17.71±4.57 | 97.14±24.70 | 9.57±3.25 |
| P | 0.61 | 0.04 | 0.78 | |
| Gender | ||||
| Male | 172 | 17.63±4.33 | 105.83±13.44 | 9.49±2.54 |
| Female | 214 | 17.60±4.40 | 104.18±12.70 | 10.11±2.44 |
| P | 0.02 | 0.22 | 0.95 | |
| Marital status | ||||
| Married | 309 | 17.7 ±4.13 | 104.63±12.85 | 9.85±2.58 |
| Unmarried | 77 | 17.17±5.21 | 106.06±13.83 | 9.74±2.15 |
| P | 0.69 | 0.41 | 0.39 | |
| Additional training of palliative care | ||||
| Yes | 224 | 17.78±4.56 | 106.36±10.68 | 10.37±2.29 |
| No | 162 | 17.38±4.08 | 102.92±15.56 | 9.09±2.58 |
| P | 0.001 | 0.02 | 0.37 | |
| Qualification | ||||
| General nursing and midwifery | 95 | 17.44±4.05 | 101.55±12.19 | 9.80±2.55 |
| Postbasic nursing | 70 | 17.61±3.81 | 102.66±11.92 | 9.51±2.83 |
| BSc nursing | 201 | 17.40±4.66 | 106.91±13.72 | 9.91±2.29 |
| MSc nursing | 20 | 20.55±3.64 | 108.80±9.07 | 10.35±3.08 |
| P | 0.54 | 0.002 | 0.02 | |
| Experience in critical care unit (months) | ||||
| 12-24 | 79 | 18.08±4.44 | 104.84±13.74 | 9.81±2.53 |
| 25-36 | 66 | 17.06±3.74 | 109.06±15.73 | 9.91±2.30 |
| 37-48 | 21 | 16.29±4.06 | 106.43±8.99 | 9.00±2.32 |
| >49 | 220 | 17.74±4.52 | 103.55±11.99 | 9.90±2.56 |
| P | 0.47 | 0.03 | 0.25 | |
| Critical care units | ||||
| Medical/surgical | 101 | 17.65±4.00 | 101.8±17.07 | 9.38±2.65 |
| Cardiology/cardiovascular surgery | 200 | 17.76±4.53 | 105.58±10.47 | 10.02±0.48 |
| Neurology/neurosurgical | 85 | 17.24±4.40 | 106.98±12.51 | 9.93±2.32 |
| P | 0.10 | 0.02 | 0.65 | |
The correlation of the age of nurses with their attitude, knowledge, and practice was −0.13, −0.05, and 0.03, respectively (P = 0.01, 0.32, and 0.50, respectively). There was a significant negative correlation of age of nurses to their attitude regarding palliative and EOLC. The correlation of the practice of critical care nurses with their knowledge and attitude was 0.14 and 0.34, respectively (P = 0.01 and 0.001, respectively). The practice of critical care nurses is significantly correlated to the knowledge and attitude of critical care nurses regarding palliative and EOLC.
DISCUSSION
We observed from our study that 41.4% of the nurses had a poor knowledge with regard to palliative care and EOLC with many perceived barriers. Furthermore, the knowledge score of female nurses regarding palliative and EOLC is significantly higher than male nurses. In the present study, a significantly higher knowledge and attitude score was found among nurses who had additional training regarding palliative and EOLC.
Similar findings have been reported by other studies as well.[910] The new findings from our study revealed that there is an utter need of higher structured training for nurses that would not only increase knowledge but also change attitude and practice pattern with regard to palliative care and EOLC. Not only higher education but also additional training like in-service training program for nurses would be helpful for better provision of palliative care and EOLC. Hence, higher education among nurses needs to be encouraged and supported. Nurses need to be timely motivated and reinforced to maintain the continuity of best care.
It appears that neurological/neurosurgical critical care units had more chronic debilitated patient in views of nature of diseases, so the understanding of palliative and EOLC appears to be better among critical care nurses in these specialties. An appropriate protocol may be developed and made available to nursing staff based on findings of the current study, and the outcome from these may be translated across all types of critical care units.
In the present study, one of the most reported perceived barriers by critical care nurse was their workload (95.1%), which is comparable to the study findings of Attia et al.[2] where all the nurses (100%) reported workload as a barrier in providing palliative and EOLC. This needs a policy consideration to include palliative care nurses as a part of routine care for patients with chronic diseases, and the nurses should be involved in treatment planning as well. New nursing post can be created as nurse counselor, palliative nurse, etc. Other barriers reported by nurses included the absence of understanding lifesaving terminology (82.6%) and denial for acceptance of poor prognosis among family members (88.6%). This indicates the need of counseling for family members and involvement of nurses as well. Majority of nurses reported that availability of good communication between health-care team (77%), provision of in-service training for nurses (68%), and involvement of family members in patient's care (81%) could support them in rendering effective palliative and EOLC.
The strength of the study lies in the adequacy of sample size, selecting the participants from the critical care units with different specialties and using a standardized tool for assessing the attitude of critical care nurses toward palliative and EOLC.
CONCLUSION
We conclude that the role of nurses for the provision of palliative and EOLC in critically ill patients is paramount. However, there appears to be a significant gap between knowledge and practices of critical care nurses related to palliative and EOLC. The barriers perceived by critical care nurses need to be addressed with administrative and clinical policies for optimal delivery palliative and EOLC. The appropriate training, policy change, and involvement of nurses in treatment planning would help in avoiding many of the barriers in the provision of effective palliative and EOLC.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Critical care nurses' perception of barriers and supportive behaviors in end-of-life care. Am J Hosp Palliat Care. 2013;30:297-304.
- [Google Scholar]
- Assessment of palliative care awareness among undergraduate healthcare students. J Clin Diagn Res. 2017;11:JC06-10.
- [Google Scholar]
- The nurses' knowledge and attitudes towards the palliative care. J Educ Pract. 2015;6:91-100.
- [Google Scholar]
- Critical care nurses' knowledge, practice, obstacles and helpful measures towards palliative care for critically Ill patients. AJNS. 2017;6:293-303.
- [Google Scholar]
- Palliative care awareness among Indian undergraduate health care students: A needs-assessment study to determine incorporation of palliative care education in undergraduate medical, nursing and allied health education. Indian J Palliat Care. 2010;16:154-9.
- [Google Scholar]
- Refining the frommelt attitude toward the care of the dying scale (FATCOD-B) for medical students: A confirmatory factor analysis and Rasch validation study. Palliative Supportive Care. 2018;16:50-9.
- [Google Scholar]
- Assessment of nurses' knowledge, attitude, practice and associated factors towards palliative care: In the case of Amhara region hospitals. Adv Biol Res. 2016;10:110-23.
- [Google Scholar]
- Assessment of knowledge, attitude and practice and associated factors towards palliative care among nurses working in selected hospitals, Addis Ababa, Ethiopia. BMC Palliat Care. 2014;13:1-11.
- [Google Scholar]
APPENDIX
Tool I: Sociodemographic datasheet
1. Age(completed years)________________
2. Gender
Male Female Others
3. Educational qualification
GNM Post Basic Bsc.Nursing BSc Nursing MSc Nursing Others ______________
4. Marital status
Married Unmarried Divorced Widow/Widower Separated
5. Years of experience in critical care _____________
6. Any previous training in palliative and end of life care,
Yes No
6.1. If Yes, mention details of training
Last training month/year ______________
Place of training_______________
Duration of training____________
7. Presently working ward/ICU _________________
Tool II: Knowledge assessment questionnaire for nurses
Instructions – These are multiple choice questions to evaluate your knowledge on palliative and end-of-life care. Read all the sentences carefully and encircle the correct option. All your answers will be treated as strictly confidential. 1 score will be given for correct answer and 0 score for incorrect answer.
1. Palliative care is defined as
Care only for dying patient Care given to cancer patients only Care given to improve quality of life Care in which aggressive treatment is given
2. Hospice care is given
When prognosis is good When patient diagnosis is made When focus is on cure of patient When all treatment fail or exhausted
3. Palliative care should begin
Before the diagnosis With the diagnosis After 2 year of diagnosis At the end stage of life
4. Deterioration of physical function towards the end of life is
A natural part of the dying process Unrelated to dietary intake Not a common occurrence for most Best managed through aggressive physical rehabilitation
5. What do you mean by ESAS
Edmonton symptom assessment scale Edmonton symptom assessment system Edmonton scale for anxiety assessment Edmonton scale for anger assessment
6. After patient admission, APACHE II score is calculated
Within 12 h Within 24 h Within 48 h Within 72 h
7. Lowest and highest score for Glasgow Coma Scale (GCS) are
3 and 15 0 and 15 3 and 12 0 and 12
8. A range of pharmacological interventions for breathlessness include
Antibiotics, aspirin, opioids, and oxygen Diuretics, bronchodilators, anti-emetics, and opioids Opioids, bronchodilators, anxiolytics, and aspirin Opioids, anxiolytics, bronchodilators, and oxygen
9. Which intervention is not recommended in the management of respiratory tract secretions at the end of life?
Deep suctioning Patient repositioning Reduction of artificial hydration Anti-muscarinic medications
10. Adjuvant analgesic in palliative and end of life care means a drug whose
primary indication is for pain only primary indication is for pain and has anxiolytic effect primary indication is for something other than pain and has no analgesic effects primary indication is for something other than pain and has analgesic effects
11. Which of the following is weaker opioid
NSAIDs Tramadol Morphine Fentanyl
12. WHO analgesic ladder for moderate to severe pain includes
Strong opioid Non opioid +/- adjuvant. Weak opioid +/- non opioid +/- adjuvant Strong opioid +/- non opioid +/- adjuvant
13. All are common anticholinergic adverse effects EXCEPT
Pupil dilation Urinary retention Increased peristalsis Increased intraocular pressure
14. Which of the following are sign of opioid toxicity
Sleepiness, hypertension, and aggression Hypertension, irritability, and restlessness Hypotension, pinpoint pupil, and insomnia Sleepiness, respiratory depression, and pinpoint pupil
15. Oral candidiasis needs treatment because
It may become a systemic infection It is painful and impacts on the quality of life It can reduce dietary intake It can exacerbate halitosis (bad breath)
16. The most appropriate first line treatment for the management of constipation is
Stool softener and stimulant Stool softener and rectal intervention Rectal intervention and stimulant Stimulant, rectal intervention, and stool softener
17. Patient who are opiate dependent will
Benefit from increase in dietary fibres Always require prescribed laxatives Need to reduce opioid dosage in case of unresolved constipation Need to drink 2-3L of fluid daily to prevent constipation
18. Which of following is a clinical feature of delirium
Disorientation to time and place with normal attention Fluctuation of symptoms over months to year Onset of impaired attention over hours to days Consistently normal level of alertness
19. Which form of euthanasia is considered to be illegal in India
Passive Active Accidental Varies according to state
20. The period of acceptance of loss and grief during which the person learns to deal with loss is known as
Normal Grief Anticipatory grief Bereavement Mourning
| Areas | Strongly agree | Agree | Uncertain | Disagree | Strongly disagree |
|---|---|---|---|---|---|
| 1. Giving care to the dying person is a worthwhile experience | |||||
| 2. Death is not the worst thing that can happen to a person | |||||
| 3. I would be uncomfortable talking about impending death with the dying person | |||||
| 4. Caring for the patient’s family should continue throughout the period of grief and bereavement | |||||
| 5. I would not want to care for a dying person | |||||
| 6. The non-family caregivers should not be the one to talk about death with the dying person | |||||
| 7. The length of time required to give care to a dying person would frustrate me | |||||
| 8. I would be upset when the dying person I was caring for gave up hope of getting better | |||||
| 9. It is difficult to form a close relationship with the dying person | |||||
| 10. There are times when death is welcomed by the dying person | |||||
| 11. When a patient asks, “Am I dying?” I think it is best to change the subject to something cheerful | |||||
| 12. The family should be involved in the physical care of the dying person | |||||
| 13. I would hope the person I’m caring for dies when I am not present | |||||
| 14. I am afraid to become friends with a dying person | |||||
| 15. I would feel like running away when the person actually died | |||||
| 16. Families need emotional support to accept the behavior changes of the dying person | |||||
| 17. As a patient nears death, the non-family caregiver should withdraw from his or her involvement with the patient | |||||
| 18. Families should be concerned about helping their dying member make the best of his or her remaining life | |||||
| 19. The dying person should not be allowed to make decisions about his or her physical care | |||||
| 20. Families should maintain as normal an environment as possible for their dying member | |||||
| 21. It is beneficial for the dying person to verbalize his or her feelings | |||||
| 22. Care should extend to the family of the dying person | |||||
| 23. Caregivers should permit dying persons to have flexible visiting schedules | |||||
| 24. The dying person and his or her family should be the in-charge decision makers | |||||
| 25. Addiction to pain relieving medication should not be a concern when dealing with a dying person | |||||
| 26. I would be uncomfortable if I entered the room of a terminally ill person and found him or her crying | |||||
| 27. Dying persons should be given honest answers about their condition | |||||
| 28.Educating families about death and dying is not a non-family caregiver’s responsibility | |||||
| 29. Family members who stay close to a dying person often interfere with the professional’s job with the patient | |||||
| 30. It is possible for non-family caregivers to help patients prepare for death |
Possible scores ranges from 30 to 150. Attitude will be categorized (arbitarily) as: Favorable attitude : >90 score. Unfavorable attitude: <90 score
| Practice areas | Yes | No | |
|---|---|---|---|
| I discuss regarding palliative care with patient | |||
| During diagnosis | |||
| When disease progress | |||
| At the end of life | |||
| I discuss regarding palliative care with family members | |||
| During diagnosis | |||
| When disease progress | |||
| At the end of life | |||
| I always inform the patient about procedures | |||
| I do patient assessment daily | |||
| For adults (>12 years) | For pediatric patients (<12 years) | ||
| Head to toe | Head to toe | ||
| Glasgow coma scale | Pediatric Glasgow coma scale | ||
| SOFA score | AVPU | ||
| APACHE II | Growth and development assessment | ||
| Braden scale | |||
| Delirium assessment | |||
| Pain assessment | Pain assessment | ||
| I manage secretions by | |||
| Suctioning as needed | |||
| Nebulization as prescribed | |||
| I maintain hygiene and care by | |||
| Daily sponging | |||
| Daily hair care | |||
| Daily mouth care | |||
| Daily changing of linens | |||
| I practice pressure ulcers prevention measures | |||
| Back massage | |||
| Positioning change | |||
| I consider cultural factors when dealing with terminally ill patient | |||
| I consider psychological factors (depression, anxiety, coping etc.) when dealing with terminally ill patient | |||
| I address spiritual issue by | |||
| Connecting with spiritual counselor | |||
| Listening with empathy | |||
| Understanding patient reaction | |||
Total score – 27. Practice will be categorized as Satisfactory: >20 score (>75% of total score), Poor: <20 score (<75% of total score). SOFA: Sequential organ failure assessment, APACHE: Acute physiology and chronic health evaluation, AVPU: Alert to voice, pain or unresponsive
| I believe following factors as barriers in providing palliative and end of life care | Not at all | To some extent | To large extent |
|---|---|---|---|
| Environmental factors | |||
| Nurses workload | |||
| Lack of privacy in ICU design | |||
| Liberal visiting hours | |||
| Restrictive visiting hours | |||
| Lack of available resources | |||
| Family members | |||
| Not understanding meaning of lifesaving | |||
| Continually calling for information | |||
| Fighting about life support use | |||
| Not accepting patient’s poor prognosis | |||
| Not present when patient dies | |||
| Nurses knowledge and skills | |||
| Lack of nursing education and training | |||
| Not knowing patients’ wishes | |||
| Treatment policy | |||
| Not considering nurses’ opinion | |||
| Calling the nurse to help with newly admit patients | |||
| Difference in physicians’ opinion about treatment | |||
| Any other (which is not mentioned above) ___________________________________________ What factors do you consider are available as a support for providing palliative and end of life care?_____________________________________________________________ What supportive factors that you feel should be available for providing palliative and end of life care that are not yet available?___________________________________________________________ | |||
ICU: Intensive care unit






