Translate this page into:
An Update on Initial Epidemiological Profile, Clinical Course, and Outcome of COVID-19 Patients at a Tertiary Care Center in India
Address for correspondence: Dr. Anjali Kochhar, 262, Narmda Apartments, New Delhi, India. E-mail: kochharanjali0@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background and Aim:
Coronavirus disease 2019 (COVID-19) has become a global pandemic with the spectrum of disease from asymptomatic or mild disease to severe cases requiring intensive care unit (ICU) admission. In India, it started with milder presentation affecting younger population. Later on, an increase in disease severity was observed involving older age group as well. However, there is a paucity of published data regarding patients requiring ICU care in India. This case series describes the initial experience of an ICU in India regarding epidemiological profile, clinical course, and outcome of critically ill COVID-19 patients.
Methods:
This case series included 27 consecutive laboratory-confirmed COVID-19 patients who were admitted in a tertiary care ICU over 14 days period, followed up till their discharge from ICU. Demographic and clinical data, including laboratory and radiological findings, were compiled with special attention to co-morbidities of the patients. The management of these patients was done as per the institutional protocol for critically ill COVID-19 patients.
Results:
The median age of the patients was 50 years with no difference in gender. Comorbid conditions were seen in 85% of the patients with diabetes (43.7%) and hypertension (37.5%) as the most common conditions. The median duration of symptoms before admission was 6 days with fever as the most common clinical symptom at presentation. Chest roentogram showed bilateral lung infiltrates in 88.8% of the patients. Mild, moderate, and severe hypoxia were observed in 3, 8, and 16 patients, respectively. Ten patients were managed with oxygen therapy. Seventeen patients (62.9%) required ventilatory support. Mortality rate among patients admitted to our ICU was 59.2%.
Conclusions:
This case series shows middle-aged patients with comorbid diseases present with severe COVID-19 disease and have poor outcome.
Keywords
Coronavirus disease 2019
critically ill patients
India
INTRODUCTION
Coronavirus disease 2019 (COVID-19) originated from the city of Wuhan, China, in December 2019, thereafter; soon it became pandemic involving Indian subcontinent as well. Up to May 12, 2020, India had 46,008 active cases, 22,454 recovered cases, and 2293 deaths.[1] COVID-19 has shown a wide spectrum of disease ranging from asymptomatic or mild disease to severe cases requiring intensive care unit (ICU) admission. Increasing number of cases led to rapid filling up of ICU worldwide. There are reports from China, Italy, and the United States that show high mortality rates among critically ill patients.[234] COVID-19 outbreak in India has shown different course as compared to other countries. Initial report showed COVID-19 presenting as mild respiratory illness in young males in India.[5] However, there is a paucity of published data regarding patients requiring ICU care in our country.
The objective of this case series is to describe epidemiological profile, clinical course, and outcome of 27 consecutive COVID-19 patients confirmed by reverse transcriptase-polymerase chain reaction (RT-PCR) and admitted in a tertiary care ICU over 14 days period. Demographic and clinical data, including laboratory and radiological findings, were compiled with special attention to comorbid conditions of the patients.
METHODS
We included the confirmed cases of severe acute respiratory illness (SARI) due to COVID-19 presenting to the ICU of V. M. M. C and Safdarjung Hospital, a COVID-designated tertiary care hospital, from April 20, 2020, to May 3, 2020. Confirmation of the COVID-19 was done by the RT-PCR assay of nasopharyngeal and oropharyngeal swab specimen in accordance with the ICMR guidelines.[6]
The management of these patients was done as per the institutional protocol for critically ill COVID-19 patients. The criteria for ICU admission were acute respiratory failure (respiratory rate >30/min and arterial oxygen saturation <92% on room air), acute respiratory distress syndrome (ARDS), septic shock, and multiorgan dysfunction syndrome (MODS).
Patients were monitored using multipara monitors with recording of heart rate, noninvasive blood pressure, arterial oxygen saturation, and temperature. Ventilatory parameters were monitored throughout along with arterial blood gas analysis. Baseline blood investigations, including complete blood count, kidney function test, liver function test, serum electrolytes, international normalized ratio (INR) and random blood sugar were monitored regularly. In addition, additional specific investigations such as lactate dehydrogenase, C-reactive protein, D-dimer, and cardiac markers (Troponin-I, Creatine phosphokinase-myocardial band [CPK-MB]) were done. Electrocardiogram was obtained daily, and QTc interval was calculated using the Fridericia's formula.
Degree of hypoxemia was categorized as mild hypoxemia PaO2/FIO2: 200-300), moderate hypoxemia (PaO2/FIO2:100-200) and severe hypoxemia (PaO2/FIO2: <100). Patients with mild-to-moderate hypoxemia were put on oxygen therapy. Criteria for intubation and mechanical ventilation were tachypnea (RR >35 bpm), worsening hypoxemia, shock, and poor Glasgow Coma Scale.
Patients were started on prophylactic broad-spectrum antibiotics including azithromycin. Hydroxychloroquine, thromboprophylaxis, and other supportive management were given as per ICU protocol. Hydroxychloroquine was discontinued in patients having prolonged QTc. Ventilatory management was done as per ARDS-net protocol.[7] Weaning was done as per the patient's clinical condition. Patients with stable hemodynamics who no longer required oxygen therapy were transferred to isolation room facility.
Data collection and analysis
Epidemiological data were collected from the patient's record. Details of current illness, comorbid conditions, and concomitant medications were also noted. Clinical course and outcome was observed during their stay in ICU and patients were followed up till their discharge from ICU.
Deidentified (anonymized) data were summarized in Microsoft Excel and analysis for continuous variables was done using median and range. For categorical variables, analysis was done as counts and percentage.
RESULTS
This report includes 27 confirmed cases of SARI due to COVID-19 requiring ICU admission from April 20, 2020, to May 3, 2020. The demographic data and co-morbid conditions of the patients are shown in Table 1. Median age of the patients was 50 years (range 9–90 years) with female: male ratio of 14:13. Eight patients (29.6%) were aged 60 years and above. Median weight of the patients was 60 kg (range 32–100). Grade-1 obesity was observed in two patients.
| Parameter | Value |
|---|---|
| Epidemiological data | |
| Total cases (male:female), n | 27 (13:14) |
| Age (years), median (range) | 50 (9-90) |
| Weight (kg), median (range) | 60 (32-100) |
| Contact history, n (%) | 2 (7.4) |
| Duration of symptoms (days), median (range) | 6 (2-21) |
| Co-morbid conditions, n (%) | |
| Diabetes | 9 (33.3) |
| Hypertension | 8 (29.6) |
| Coronary artery disease | 2 (7.4) |
| Valvular heart disease | 2 (7.4) |
| Chronic kidney disease | 2 (7.4) |
| Thyroid disease | 2 (7.4) |
| Seizure disorder | 2 (7.4) |
| Psychiatric illness | 2 (7.4) |
| Chronic obstructive pulmonary disease | 2 (7.4) |
| Cancer | 2 (7.4) |
| Gout | 1 (3.7) |
| Tuberculosis | 1 (3.7) |
| Poliomyelitis | 1 (3.7) |
| Trauma (femur fracture) | 1 (3.7) |
| Pancreatitis | 1 (3.7) |
Majority of the patients (85%) had associated comorbidities. Among these, diabetes (43.7%) and hypertension (37.5%) were most common. Nearly 18.7% of the patients had both of these chronic illnesses [Table 1].
None of the patients had a history of travel. Two patients (7.4%) had a history of contact with the COVID-positive patient. Twenty-one patients were admitted directly, and six patients were referred cases from other hospitals [Table 1].
Majority of patients (66.6%) were admitted to the ICU during their 1st week of illness, 14.8% in the 2nd week, and 18.5% in the 3rd week of illness. Median duration of symptoms before admission was 6 days. Clinical symptoms at the presentation included fever (77.7%), shortness of breath (70.3%), and cough (62.9%) [Figure 1].
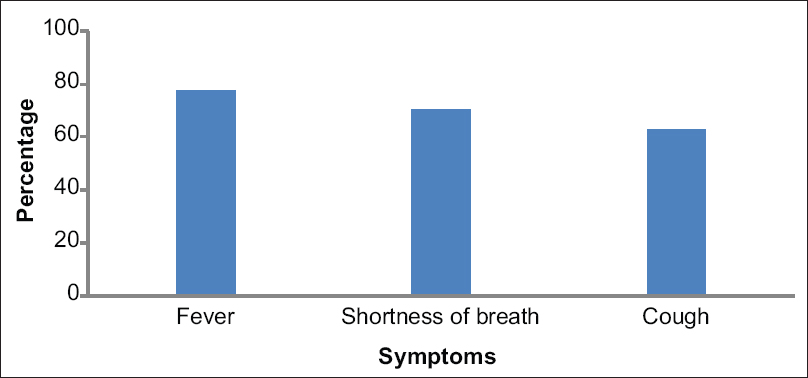
- Clinical symptoms at presentation
Baseline laboratory data are shown in Table 2. Three patients had hemoglobin <7 g/dl requiring blood transfusion. Two patients had lymphocytopenia (lymphocyte count 3%). Thrombocytopenia and thrombocytosis were observed in one patient each. Serum bilirubin was found to be raised in one patient. Liver enzymes, aspartate aminotransferase, and alanine aminotransferase were found to be elevated (> three times) in six (22.2%) patients. None of the patients had coagulopathy at the time of admission. Lactate and creatinine were elevated in seven (25.9%) and five (18.5%) patients, respectively.
| Parameter | Median (range) |
|---|---|
| Hemoglobin (g/dl) | 10.1 (6.3-15.1) |
| WBC’s (per mm3) | 8800 (3800-16,300) |
| Platelet count (per mm3) | 180,000 (72,000-624,000) |
| Serum bilirubin (mg/dl) | 0.7 (0.2-2.3) |
| AST (u/l) | 57 (15-736) |
| ALT (u/l) | 48 (5-531) |
| Serum creatinine (mg/dl) | 0.8 (0.2-9.2) |
| Lactate (mm/l) | 1.5 (0.3-4.3) |
| INR | 1.08 (0.8-1.5) |
WBC’s: White blood cells, AST: Aspartate aminotransferase, ALT: Alanine aminotransferase, INR: International normalized ratio
Chest roentogram showed bilateral lung infiltrates in 88.8% of the patients. Empyema and pleural effusion were seen in one patient each.
Mild, moderate, and severe hypoxemia was observed in 3, 8, and 16 patients, respectively [Figure 2].
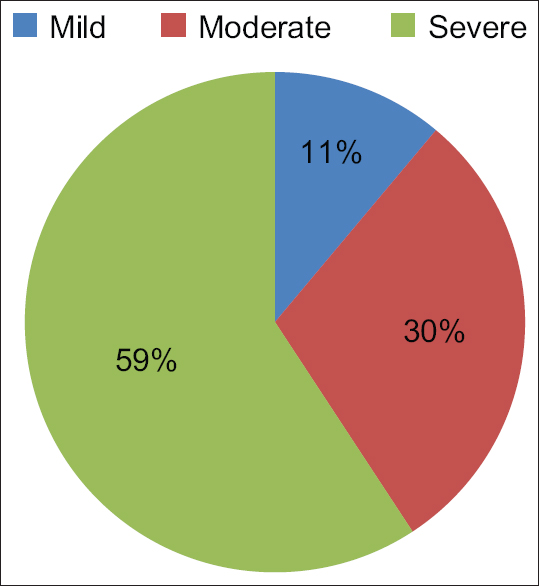
- Degree of hypoxia
Ten patients (37%) were managed with oxygen therapy. Seventeen patients (62.9%) required ventilatory support. Seven patients (25.9%) developed shock and MODS during their ICU stay. Mortality rate among patients admitted to our ICU was 59.2%. Individual patient course is shown in Figure 3.
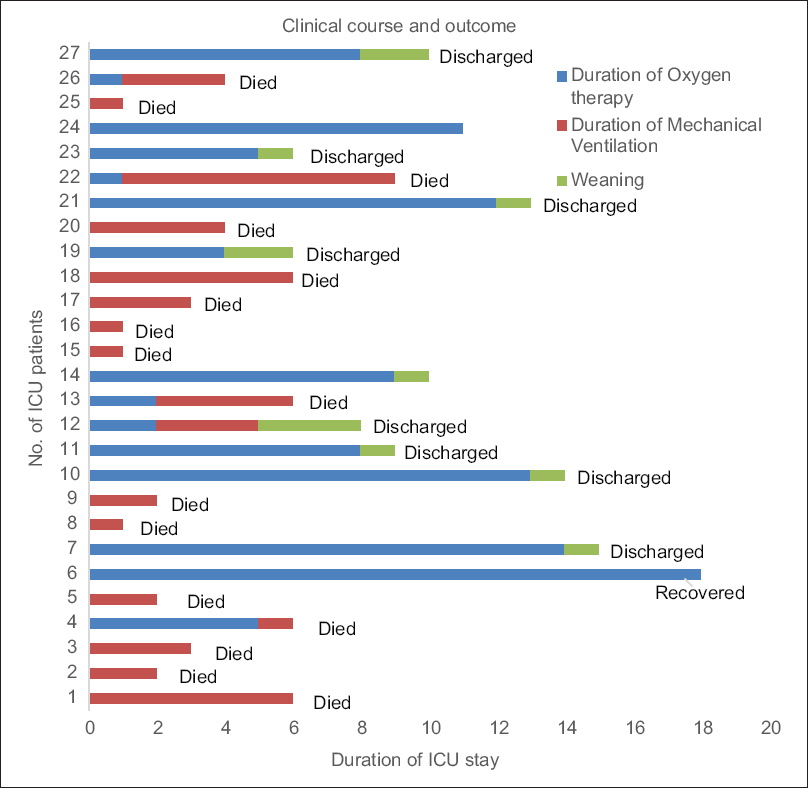
- Clinical course and outcome of individual patient
DISCUSSION
To the best of our knowledge, this is the first case series reporting epidemiological profile, clinical characteristics, and early outcome of confirmed cases of SARI due to COVID-19 requiring ICU admission in the Indian population.
Our data shows that ICU admission was required in the middle-aged patients (median age 50 years) with no significant gender difference. Initial data of first 21 patients admitted in the same centre in India showed male preponderance (median age 40 years) with mild disease course.[5]
We observed the higher incidence of comorbidities (85%) compared to the reports by Wang et al. (72.2%) from China and Grasselli et al. (68%) from Italy in critically ill patients.[89] This could be due to the genetic and racial differences in patient population. Diabetes and hypertension were the most common comorbid illnesses in critically ill patients as seen by most of the previous studies.[4910]
History of travel was reported in 62% patients by Gupta et al., whereas none of our patients revealed such history. This difference could be possibly due to potential community transmission of the disease owing to rapid human-to-human transmission at the time of this report.[111213]
The median duration of symptoms observed was 6 days in our series similar to the findings by Guan et al. from China.[14] Fever was the most common presenting symptom followed by shortness of breath and cough in this case series, whereas cough was observed as the most common presenting symptom by Young et al.[15]
Lymphopenia, a cardinal feature of SARI due to COVID-19 was observed in only two patients in our series, whereas the reports by Zhou et al. and Bhatraju et al. reported higher incidence of lymphopenia in their series.[210] This difference could be due to the less number of patients observed over a limited period of time in our report or difference in the severity of disease. Bilateral lung infiltrates were observed as the most common radiological finding as mentioned in other reports.[1015]
Majority of the patients on mechanical ventilation succumbed to the disease. The mortality rate of the patients requiring mechanical ventilation was high in our case series as reported from China, Washington, and New York Area.[2416]
Among the patients who died, 59.2% had associated comorbid diseases with 37% having 2 or >2 comorbid conditions. Bhatraju et al. in their case series from the Seattle region have also observed poor outcome among the elderly and in patients with comorbidities.[10]
We observed 59.2% mortality rate in our ICU which is lower than the reported by previous reports (62%–78%). The possible reason for this observation could be the difference in severity of the disease.[21617]
Limitations of our study include the data from a single center and observations over a limited period of time. As it is an initial experience, there is a need for larger data over a long period of time to know the course and outcome of disease in India.
CONCLUSIONS
This case series shows middle-aged patients with comorbid diseases present with severe COVID-19 disease and have poor outcome. Considering the novel infection and with evolving change in treatment strategy, our study can be a stepping stone for further research and data analysis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2020. Available from: https://www.mohfw.gov.in
- Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054-62.
- [Google Scholar]
- Case-fatality rate and characteristics of patients dying in relation to covid-19 in Italy. JAMA. 2020;323:1775-6.
- [Google Scholar]
- Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area and the North well COVID-19. JAMA 2020 pii: e206775
- [Google Scholar]
- Clinical and epidemiologic profile of the initial COVID-19 patients at a tertiary care centre in India. Monaldi Arch Chest Dis. 2020;90:1294.
- [Google Scholar]
- Available from: https://mainicmrnicin/content/covid-19
- Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301-8.
- [Google Scholar]
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-9.
- [Google Scholar]
- Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574-81.
- [Google Scholar]
- Covid-19 in critically Ill patients in the Seattle Region – Case series. N Engl J Med. 2020;382:2012-2.
- [Google Scholar]
- A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395:514-23.
- [Google Scholar]
- Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382:872-4.
- [Google Scholar]
- Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199-207.
- [Google Scholar]
- Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-20.
- [Google Scholar]
- Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323:1488-94.
- [Google Scholar]
- Characteristicsand outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612-4.
- [Google Scholar]
- Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-81.
- [Google Scholar]






