Translate this page into:
Approaches and Best Practices for Managing Cancer Pain within the Constraints of the COVID-19 Pandemic in India
Address for correspondence: Dr. Nandini Vallath, Room No. 821, Homi Bhaba Building, Tata Memorial Hospital, Dr E Borges Road, Parel Mumbai - 400 012, India. E-mail: aanandini@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Novel corona virus disease 2019 (COVID-19) is an ongoing pandemic that has impacted the entire world. The Indian government has responded strongly and very stringently to the crisis, through a nationwide lockdown. The health-care (HC) systems in the country are striving hard to maintain equitable care across illness spectra, while responding the emergencies imposed by the COVID-19 crisis. Under these circumstances, guidelines for managing several diseases including that for cancer care have been modified. As modified guidelines for cancer care have their focus on disease management, cancer pain management and maintaining continuity of care for patients with advanced progressive disease have taken a backseat in the available cancer care guidelines. This article describes the challenges, approaches to solutions with evidence-based practices that can be utilized to ensure competent management of cancer pain during the COVID-19 pandemic in India. It provides an overview of adapting to telehealth consultations for identification, evaluation and management of cancer pain, safe and rational use of analgesics and adjuvant drugs, recognizing and responding to holistic care needs and addressing the total pain, ensuring continuity of pain management, and strategies when complying with narcotic drug regulations, while ensuring safety of patients and HC providers.
Keywords
Neoplasms
pain management
severe acute respiratory syndrome coronavirus 2
“In the midst of this catastrophe, more than looking in to find serenity we need to look out for one another to practice humanity.”
–Abhijit Naskar
INTRODUCTION
Corona virus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus has rapidly progressed to a stage of public health emergency of international concern.[1] Not only has it majorly impacted the global health; it has brought the economic, social, and political processes around the world to its brink.[23] As a response to this global crisis, the Government of India announced a nationwide lockdown to contain the spread of infection.[45] These events have compromised equitable health care (HC) to an extent and has specifically jeopardized the health of chronically ill, such as cancer patients.
Pain is highly prevalent in cancer and managing pain is an integral part of caring for cancer patients. 55% of patients on active treatment and 66% with advanced disease experience pain. Of these, >50% patients suffer with moderate to severe pain.[6] Poorly managed pain negatively impacts quality of life, adversely affects adherence to treatment, worsens prognosis, and should be prevented.[789]
Cancer patients have higher vulnerability for COVID-19 infection as they are immune compromised and have greater morbidity and mortality once infected.[1011] Hospitals act as hotspots and become sources of very high transmission. To thwart the increased COVID-related morbidity and mortality within hospital environment, cancer care guidelines have emerged with prioritization criteria including risk versus benefit ration for withholding or postponement of cancer treatment. Oncology treatment protocols that caused immune suppression have also been modified.[121314] Yet, the guidelines have no clear recommendation for managing cancer pain management within the modified dynamics of the present situation. The management guidelines for chronic pain, specific to COVID-19 pandemic, also have not addressed the specific concerns of managing pain in cancer patients.[1516]
This paper is the result of structured interactions among pain and palliative care teams at 7 tertiary cancer hospitals of the National Cancer Grid-India network. The participating centers were located in tier one or two cities, with five of them situated in the “red zones”[16] with a substantial number of COVID-19-positive cases and high level of infectivity in the region. The challenges and mitigating practices at the seven centers were sought, and collated, along with scoping of literature. The teams provided information on their practices specifically related to managing cancer pain as per their institutional policies, modifications for patient interactions, systems in-place for evaluation, criteria and planning for patient admissions, alterations in drug regimens and methods for review. They also shared experiences on using virtual platforms, on the challenges faced and approaches found useful in providing psychosocial care.
The unique challenges in managing cancer pain in tertiary cancer care settings, during COVID-19 pandemic contextual to the Indian sociocultural-economic settings listed in Box 1, are described in detail.
| Access to an appropriate health-care facility |
| At the health-care facility |
| Ethical challenges |
| Challenges related to in-person patient-professional interactions |
| Challenges related to virtual consultations |
| Challenges related to analgesic medications |
| Choice of medications, prescriptions, and regulatory mandates |
| Access and availability of medications, medicines refills |
| Review, monitoring medication, adverse effects |
| Challenges multidisciplinary pain management |
| Managing cancer pain in special population |
| Challenges with cancer pain related academic and research activities |
Each section below describes a challenge along with approaches to find solutions and improve care with best practices where relevant.
ACCESS TO AN APPROPRIATE HEALTH-CARE FACILITY
The government has acquired and reserved a substantial percentage of out-patient consultation space and hospital beds in both the government and private sector, for caring of COVID-19 patients. The prolonged lockdown in many regions has affected all movements, including public and private transport facilities. There is a paucity of available means of transport for sick patients who must travel long distances to access a palliative care specialist service. They often depend on taxis, private vehicles, and ambulances, which have increased their charges due to surge in demand, and suffer financially.[17] The hospices, homecare services, and private nursing homes have scaled down their services, worsening the already limited access to pain and symptom management for cancer patients.[18]
This impacted access to competent care for homebound advanced cancer patients with poor general status, suffering with severe pain.[19]
APPROACHES, SOLUTIONS, BEST PRACTICES
A simple system of online issue of electronic passes (e-pass) for travel[20] is currently active in 17 states of India. Various community-based organizations have also extended support with provision for free or low-cost ambulance services to and from hospitals. Informing and supporting families on using this method has resolved transport issues for some patients. For those patients who require in-person consultation, but are unable to travel in spite of these provisions, liaison with a local family physician over teleconsultations (described below) has been valuable.[21] There is a need and scope for better and more robust solutions to address these challenges.
AT THE HEALTH-CARE FACILITY
Ethical challenges
During the current stage of pandemic with high community level transmission, suggesting in-person visits to outpatient departments or admitting to inpatients have become much more of a grey area than ever before. The focus of HC facilities on COVID-19 infected patients has impacted access to specialist-consultation, in-patient (IP) admissions, and the overall care for distressed patients with cancer pain.[131822] Patients requiring laboratory or radiological investigations for establishing a pain diagnosis and those who need disease modifying treatments for managing emergencies do require in-person visits to hospitals. Recurrent hospital visits for uncontrolled symptoms increases the risk of contracting COVID-19 infection and causes financial burden for the patients. The case example described in Box 2 illustrates how these issues compound together and aggravate the situation for individual patients.
| 61-year-old Mrs. K, suffering from metastatic adenocarcinoma of lung, presented to Palliative Care Out Patient Department in the cancer hospital, with severe pain on her right lower limb, which was red and swollen for past 10 days. There was bluish discoloration of her right toes for 3 days. The pain was not controlled with Morphine 20 mg PO q4h and Paracetamol 650 mg PO q6h. There was no preceding history of trauma. The pain was managed in the OPD using IV paracetamol 1 g in addition to her ongoing medicines. Investigations revealed raised neutrophil counts, deep venous thromboembolism of right lower limb |
| Conventionally, she would have been admitted for management of pain, anticoagulation and infection control. Due to infectivity risk, altered admission criteria, lack of available beds, she and her accompanying son were provided with the prescription and advised to take the required injections and further management near her home while registering for phone follow-up |
| The affordable public hospitals were full and the private hospitals and nursing homes were expensive. Moreover, the costly COVID-19 testing was mandated before any form of care. The patient was left with no choice but to visit the PC unit at the same cancer hospital, to take the daily injections. As this involved 50 km travel daily, costing INR 2000 per day, Mrs. K decided to stay on the footpath near the hospital for the days required to complete her treatment |
IV: Intravenous, COVID: Corona virus disease, OPD: Out Patient Department
CHALLENGES RELATED TO IN-PERSON PATIENT-PROFESSIONAL INTERACTIONS
Challenges due to mandated social distancing, time constraints, and minimizing interactions impacted detailed nursing assessment, physical assessment, history taking, verbal and nonverbal communications, and counseling. This caused difficulties in establishing a pain diagnosis. Requirements for personal protective equipment (PPE), skeletal staffing, and the need to avoid congested workspaces led to reduction of the number of ongoing consultations at any point in time. This affected privacy, increased the waiting period for patients, and affected therapeutic relationship with the patient. These problems were enhanced by the fear of contagion in health-care professionals (HCPs) as well as patients and caregivers.
APPROACHES, SOLUTIONS, BEST PRACTICES
Various steps were taken at multiple levels during a patient's journey in the hospital to minimize transmission and to prevent risk of infection of HCPs, patients, and their relatives [Box 3].
| Reduce patient-professional in-person contact | |
|---|---|
| Use telephonic interactions to schedule both new patient and follow-up appointments | |
| Choose appropriate platforms for teleconsultations. E.g., visual platforms preferred for initial consultations, or for new symptom related or psycho-social consultations | |
| Protocols for triaging to different settings lowers patient load, prevents congestion | |
| Better coordination is achieved by clear demarcation of roles and responsibilities | |
| Adequate distancing can be maintained by modifying seating arrangements in waiting halls | |
| Use of PPEs and transparent screens – to ensure safe in-person interactions | |
| Modified nursing assessment, with brief, focused history taking and recording | |
| Limit in-person contact time through | |
| Direct contact reduced by self-assessment by the patient – e.g., thermometer, pulse-oximeter | |
| Sharing details of treatment/investigations/medication as scans or photographs | |
| Meticulous documentation for regulatory and contact tracing purposes | |
| Use of sign boards - for instructions to declare symptoms, hygiene requirements, for indicating directions | |
| Videos for patient education and guidance | |
| Infection control protocols | Communications |
| One relative per patient. Allowance beyond waiting room decided on individual needs, e.g., disability, pediatric patient etc. | In-person counseling affected due to PPE as well as the time constraints for one to one interaction |
| Separate entry and exit point | Transparent screens preferred during in-person counseling sessions rather than using face masks |
| Screening all patients/caregivers for COVID-19 contact/travel history, symptoms | When using face masks - ensure verbal expressions of empathy and eye contact during communication to build trust and therapeutic relationships |
| Advocacy, awareness and information provision Compulsory use of face masks by everyone and provisions for it | |
| Educating on appropriate use of PPE | Elicit fears and doubts of patients and caregivers, verbally |
| Regular drills for HCPs at different settings, to emphasize infection control protocols | Activate mechanism for routine updates on authentic information about policies, and schemes relevant to their care. E.g., E-pass for public transport |
| Clear waste disposal protocols | |
| Modified HR policy | |
| Workforce segregation to reduce overall exposure | |
| Ensure availability of workers across shifts | |
| This also supports stand-by staff in the event of infection of one of the HCPs | |
| Allowing work from home for at risk HCPs | |
PPE: Personal protective equipment, HCPs: Health-care professionals, COVID: Corona virus disease, HR: Human Resource
Although every situation needs to be judiciously examined with risks/benefits and empathetic communication, an institutional policy guided by the cardinal principles of medical ethics was used to support decision-making.
Limiting patient movements within the hospital was one strategy adopted. Guidelines with generalist competencies for managing cancer pain were activated to enable oncology professionals to treat cancer pain as a part of comprehensive cancer management plan. Indicators for referrals based on the complexity of the pain or patient's distress helped triage those requiring specialists palliative care.
Inpatient admissions protocols were adapted from ESMO guidelines for managing emergency pain situation.[12] The choice for aggressive interventions was guided by NHS guidelines that featured prognostication, frailty score, and patient wishes for individual decision-making.[1213232425]
All institutions had their own protocols-based urgency of situation, which guided the need for laboratory or radiological investigations and for prioritizing for disease modifying treatments such as radiotherapy. For example, patients with pathological fractures requiring emergency surgical stabilization or those with spinal cord compression or symptomatic brain metastasis needing urgent radiotherapy were prioritized for early interventions.
VIRTUAL CONSULTATIONS
Virtual care was adopted as an interim solution to social distancing policies. According to 2019 Telecom statistics, 90% Indians have access to telephone connections.[26] This penetration of telephones supported the implementation of telemedicine guidelines put forth by the Ministry of Health and Family Welfare in collaboration with Medical Council of India (MCI), to ensure timely, quick, effort, and cost-saving HC provision to people across the country during pandemic situation.[21]
The guidelines encompass audio, video, text-based, and asynchronous (emails/fax/recordings) consultations. Video consultation is a viable option for the urban population as 97% have access to internet connection. However, this is not an option for those who live in rural India, as 75% population do not have internet access.[26] The advantages and concerns about of virtual consultations are mentioned in Box 4.
| Advantages of virtual consultation |
| Quick, low cost alternative to access to health-care services backed by clear processes and guidelines by MOHFW/MCI for telemedicine consultations |
| Avoidance of travel is advantageous to the pandemic situation |
| Access to telephonic consultation is equitable, due to the high |
| penetration of phones within rural India |
| Concerns regarding teleconsultations |
| Unfamiliarity, technological and technical difficulties |
| Very poor patients may not have access to mobile phones or internet connection |
| The development of rapport is more difficult than when consulting in-person |
| Extra efforts are needed to develop adequate systems for scheduling telephonic appointments and for satisfactory documentations |
MOHFW: Ministry of Health and Family Welfare, MCI: Medical Council of India
BEST PRACTICES AND APPROACH TO USING TELECONSULTATIONS
The best practices adapted for assessing, triaging, and managing pains and for monitoring impact of pain management through virtual care are depicted in Figure 1 and Table 1.
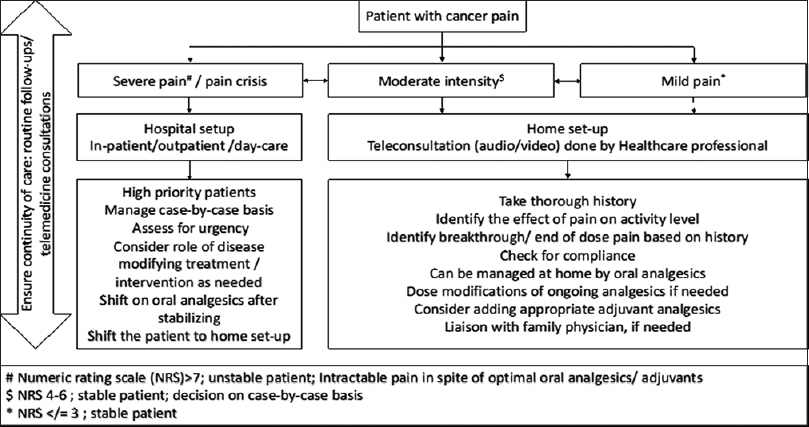
- Triaging patients with cancer pain
| Items | Description |
|---|---|
| Context | Patients with cancer having mild-moderate pain |
| Appropriate for telemedicine consultation, based on triaging and judgment of RMP/HCP | |
| Review of hospital records/available patient related data-previous prescription records, investigations, imaging, etc. | |
| Mode of communication | Video/audio/text depending upon the feasibility and access |
| Video/audio consultations are preferred as they are real-time | |
| Type of consultation | New consultation (on records of previous consultation/previous consultation >6 months back) - Identifying the reason for consultation, discussion with referring specialist and reviewing the past records where feasible |
| Follow-up (previous consultation done within past 6 months) - review the previous records, medicines prescribed, documented response to previous treatment | |
| Identification of HCP and patient | HCP is RMP, Nurse, Allied Health Professional, Mid-level health provider, ANM or any other health worker designated by an appropriate authority |
| Patient’s identity is verified by confirming the name, age, address, hospital registration ID If patient’s relative is the contact person- identification of the relative and his/her relationship with the patient | |
| Identity and designation of the HCP are disclosed at the beginning of the conversation | |
| Consent | Explicit consent of patient for telemedicine consultation is taken in form of text/email/audio/video and documented for records by the HCP for every call initiated by HCP or caregiver |
| Consent is implied if call is initiated by the patient | |
| Patient evaluation (communication pearls: Uninterrupted attention, empathy, acknowledging restraints for nonverbal communication, focused questioning and summarizing) | Detailed pain history (directly from patient, if possible): Onset of pain, intensity (use of verbal rating scale*), quality descriptors, site, radiation/referral of pain, duration, aggravating or relieving factors, variability with time, effect of pain on activity, mood and cognition of patient |
| Other relevant history: Trauma, fall, any wound, redness/swelling, skin changes, compliance, check pain diary*, associated symptoms (constipation, drowsiness, urinary retention, etc.), adverse effects of ongoing medications* | |
| Examination (video based consults): Limited inspection and guided physical examination with the help of caregiver if possible | |
| Identify the psychosocial impact of pain | |
| Identify need for a multidisciplinary team approach/intervention | |
| Patient management | Establish a pain diagnosis based on history and clinical judgment |
| Establish a realistic pain goal for the patient | |
| Educate and empower patient and caregiver about self-management techniques | |
| Decide on modifying the ongoing analgesics or prescribe appropriate analgesics or other medications as per the regulations laid by the telemedicine guidelines of MOHFW[22] | |
| Prescription in appropriate format issued by RMP as per Indian Medical Council Regulations provided as photo, scan, digital copy of a signed prescription or e-prescription via messaging or email[22] | |
| Fix the follow-up teleconsultation appointment date and time and provide contacts for reaching out |
HCP: Health-care professionals, RMP: Registered medical practitioner, MOHFW: Ministry of Health and Family Welfare
The elements of telemedicine consultation that are considered and adapted for cancer pain management are described in Table 1.
This structured process accompanied with meticulous documentation is a solution to overcome challenges in virtual pain assessment and management. The process teleconsultation may further be facilitated using simple follow-up tools such as scanned notes, reports, or E-mails to the patients.
MANAGEMENT OF CANCER PAIN
The general principles that guide cancer pain management during the COVID-19 crisis are listed in Box 5.
| Endeavor to maintain satisfactory pain relief, irrespective of circumstances to allow an acceptable QoL |
| Modify guidelines that limit access to cancer pain relief by engaging government agencies and the civil society during the pandemic, e.g., teleconsultation guidelines that included narcotic analgesics under “prohibited list” |
| Every attempt to adhere to the dictum recommended by the WHO in administering Analgesic Medicine: “By Mouth,” “By the Clock,” “For the Individual” and with “Attention to Detail” |
| Avoiding intravenous route and substituting with oral, transdermal and occasionally subcutaneous is all the more important in these times of difficult access to institutions |
| Maintain uninterrupted supply of analgesics by sending medications by post, fulfilling the requirements mandated by the NDPS rules |
| Anticipate and plan early to maintain stocks to prevent interruption in supply |
| Maintain affordability and availability of analgesics for vulnerable populations, through advocacy with the concerned regulatory authorities |
| Ensure safe and rational use through planned reviews on analgesia, activities, adverse effects to titrate |
QoL: Quality of life
The specific challenges to managing cancer pain are categorized under (i) choice of medications, (ii) prescribing practice, (iii) regulatory mandates, (iv) accessing medications, (v) reviews and titrations, and switching of medication, and (vi) ensuring uninterrupted supply of narcotic medications.
WHO STEP 1 ANALGESICS AND ADJUVANTS
Paracetamol and NSAIDs are approved as over-the-counter medications through teleconsultation, easy to access for patients.[21] Adjuvant analgesics such as steroids, anticonvulsants, antidepressants, antispasmodics, and bisphosphonates are required alone or in combination to manage complex cancer pain syndromes.[2728] Their use reduces the overall opioid requirement[2930] [Table 2].
| Challenges | Approaches, solutions, best practices |
|---|---|
| Use of round-the-clock paracetamol or NSAIDs can mask critical symptoms like fever, and affect early diagnosis of COVID-19 infection | When the step 1 analgesics are deemed necessary, the total dose and frequency of dosing is maintained lower than the usual round the clock regime, to help detect any underlying inflammatory symptoms and signs |
| Steroids can suppress immunity, increasing vulnerability to infections | Use of steroids however, was restricted to very specific cancer pain conditions or emergencies such as spinal cord compression, brain metastasis |
| Difficulty with detailed assessment of the patient impeded diagnosis of neuropathic contributors to pain, the requirement and use of adjuvant analgesic | A modified protocol for history taking, assessment with focused questions establishing a pain goal presence of a personal care-giver |
COVID: Corona virus disease, NSAIDs: Nonsteroidal anti-inflammatory drugs
WHO STEP 2 ANALGESICS
Although WHO Step 2 analgesics work partly through opioid receptors, most drugs from this group which are available in India, such as tramadol, tapentadol, and buprenorphine are included in Schedule H class of prescription drugs in India, and hence prescription only drugs.[31] with exception of codeine, they are not prohibited for use through teleconsultation[32] [Table 3].
| Challenges | Approaches, solutions, best practices |
|---|---|
| Monitoring of therapeutic and adverse drug effects (if any) | Telemedicine follow-up every alternate day to review pain relief, and titrate to maximum permittable dose depending on the patient metabolic profile, pain diagnosis, risk of drug interactions to balancing analgesic benefit and risk of adverse effects. This is followed by planned teleconsultation regularly |
| They are schedule H drugs | Detailed e-prescriptions as per mandates are issued for ease of access from chemists |
| Step 2 narcotics share the side effect profile of all narcotics | Anticipatory prescriptions for avoiding adverse effects |
| Tramadol has risk of lowering the seizure threshold for patients who are more prone to have seizures and risk of drug interactions like serotonin toxicity[43] | Tapentadol does not have seizure potential and has more potent opioid receptor action as compared to tramadol.[44] This is a preferred step 2 drug when managing patient remotely |
| Buprenorphine is available as injectable, sublingual tablets and transdermal patch formulation. However, the evidence for clear benefit for buprenorphine for management of cancer pain is unclear[45] |
WHO STEP 3 ANALGESICS
Morphine, fentanyl, and methadone are the step 3 narcotic analgesics available in India. These are safe, economic, and effective for the management of severe cancer pain when used rationally. They have no ceiling dose.[3435] In India, morphine is available as immediate release and controlled release tablets and injections, fentanyl as transdermal patches and injections and methadone is available as oral liquid and tablets. The narcotic drug law categorizes them under Essential Narcotic Drugs (ENDs) and mandates certain regulatory requirements when using them.
The current guidelines for telemedicine consultations categorize them under 'prohibited drugs' for prescription. This has impacted follow-up opioid refills for patients with stable pain relief with opioid therapy and maintaining the continuity of care.
Another concern specifically in the pandemic is the potential of high-dose opioids for immune suppression, if continued for several weeks. This effect is highest with morphine and fentanyl and least with buprenorphine.[3336373839]
BEST PRACTICES, APPROACHES, AND SOLUTIONS
In-person consultation is mandated for initiating step 3 opioids. Best practices for selecting the right patient for opioid therapy based on type and severity of pain are continued along with screening for abuse potential and stablishing pain goal. Patients are counseled at length to clarify their questions, misconceptions, and fears about the drug. They are sensitized about side effects that may be expected and need for compliance, self-monitoring, keeping the pain diary [Appendix 1]. They are also provided with helpline contacts numbers for asking questions, reporting of adverse effects, or any other serious symptoms.
Monitoring of patients and dose titrations are done with the help of teleconsultations, reviewing of pain diaries using technological solutions such as scans, e-versions, or photographs of pain diaries. Patients can get stock of pain medications for 100 doses.
The petition by the Indian Association of Palliative Care to allow use of teleconsultations for refills and switching of ENDs to treat severe cancer pain condition, is under consideration by the Board of Governors of the MCI.[40]
The article 52E of NDPS act provides certain guidelines on transport of ENDs by post, courier, rail, or road [Box 6]. This provision is now utilized for delivering the medicines to patients who do not have access to these controlled medicines within their locality for their medicine refills.
| Article 52E, Narcotic Drugs and Psychotropic Substances NDPS (Third Amendment) Rules, 2015 |
|---|
| The transmission of ENDs by in-land post or courier or by rail or by road by a manufacturer, licensed dealer or licensed chemist is permitted, subject to the following conditions namely |
| The parcel of the ENDs when sent by post shall be sent by registered post |
| The parcel of ENDs shall be accompanied by a declaration showing the names of consignor and consignee, the contents of the parcel in detail, the number of license or authorization or recognition held by the consignee |
| The consignee shall show distinctly in his account books, if he is a licensee, the name of the consignee and the consignor respectively; and the quantity of the ENDs imported inter-state, exported inter-state or transported by and to him, as the case may be, from time to time, by post or by courier or by road or by rail |
ENDs: Essential narcotic drugs, NDPS: Narcotic Drugs and Psychotropic Substances
CONTINUITY OF CARE AND FOLLOW-UPS
It is irresponsible to start opioid analgesics without provision for regular follow-up. The lockdown has become a significant hurdle for regular reviews. However, prompt publishing of telemedicine guidelines came as a huge support. The guidelines have clear provisions for liaison with local physicians and for cross-consultations with specialists, and these provisions have been used when relevant.
MULTIDISCIPLINARY PAIN MANAGEMENT
Some of the important approaches to multidisciplinary pain management are assessing and managing “total pain,” cognitive-behavior therapy, counseling, provision of psychosocial and spiritual support, physiotherapy, acupuncture, etc.[8] Approximately 8% of patients with cancer pain may benefit from interventional pain management procedures for nerve blocks.[4142]
Need for physical closeness or contact for certain multidisciplinary pain-relief inputs and difficulties with intervention pain management procedures are some of the challenges during the pandemic situations.
Concerns such as anxiety, social isolation, stigmatization, job loss, poverty, fears related to discontinuity of cancer treatment, disease progression, uncertainty, and fear of contracting COVID infection are all biopsychosocial factors that can interact with pain in a complex manner and enhance it to a state of “total pain.” These challenges can be addressed through telehealth consultations for psycho-socio-spiritual support, especially when using videos or video-based consultations. This mode of communication to express empathy and empower patients and caregivers by the counseling team member is useful even when patients visit the HC facility, to shorten the in-person meeting time.
Elective pain management procedures such as nerve blocks are deferred during the period of pandemic. If the indications are considered apt, and the required competencies are present in the locality of the patient, cross consultation facility provided by teleconsultation guidelines may be utilized to connect the patient with the intervention specialists to facilitate mitigation of pain.
SPECIAL CONSIDERATIONS
Managing pain in pediatric population and at end-of-life is specifically challenging during pandemic. Using virtual teleconsultation platforms to liaise with family physicians, educate and support parents and family members, regular and frequent phone calls, and being available for any emergency teleconsultation are some of the implemented solutions. For families of deceased patients, bereavement support is extended in form of phone calls.
ACADEMIC AND RESEARCH ACTIVITIES
Ongoing clinical trials and research are facing challenges, due to the unanticipated pandemic situation. Acknowledging the long-term nature of the current situation, the research committees and regulatory authorities have developed pragmatic guidelines. For example, approval processes for studies focused on patients suffering from COVID-19 infection have been expedited. The participant information documents, and informed consent forms have been appraised and modified to reduce risk of visiting HC facility for the patients/research participants.
The educational and training activities for trainees and students as well as evaluations are using video-based platforms to ensure continuation of training and graduations. The IAPC initiated a nine weeklong ECHO-based interactive sessions on subjects relevant to the practice palliative care in India within the constraints of COVID-19 pandemic. One of the sessions dealt with for awareness about policies, regulations, and provisions for prescribing and dispensing ENDs and ensuring adequate access to cancer pain management.
SUMMARY OF KEY LEARNINGS
General
-
Although the pandemic has created unique challenges for managing patients with cancer pain, with diligence, many of the concerns can be overcome to continue to provide quality care
-
Discussions among teams facing common problems pave the pathway to solutions
-
The PC team needs to provide whole person care within the safety policies, and with some patience and teamwork, it is possible
-
There are team several support systems available in each locality – both government and non-governmental. Problems that may appear unique may be solved through focused search. E.g. list of 1200 post offices maintained for essential services by the Indian post on their website came into use for delivering medicine refills to patients living remotely
-
The teleconsultations guidelines are be adapted for providing quality cancer pain management
-
With collective effort and diligent pursuit, even regulatory restrictions can be modified for a worthy cause. For example, the petition signed by a few hundred prescribers has been submitted by the IAPC to the board of governors at MCI. This seeks permission to prescribe ENDs refills through teleconsultation for maintaining pain relief in a cancer patient and has received an initial positive response.
Specific to managing cancer pain
-
All patients are preferably screened through telephone to decide who may need in-person visits
-
Appropriate PPEs and universal hygiene measures are to be accepted as routine for in-person consultation
-
The duration of in-person consultations can be reduced using simple patient intake self-fill forms or using telephone to fill the form by an HCP
-
Teleconsultation guidelines by the MCI provide opportunity for detailed evaluation, through virtual platforms
-
All medications, especially opioids, need to be dispensed for longer periods, to reduce frequency of travel by the patient/family during these challenging times
-
Along with this, counseling the patient on the prescribed drugs and educating on details of storing, using, and returning the drug need to be even more stringent
-
Planned reviews for analgesia, activities, adverse effects, and abuse potential are vital for ensuring safe and rational opioid therapy
-
Pain diaries are excellent aids to assess effectiveness of dose, guide titration, ensure compliance, side effects, and continuity of care, and provide documentation for discussions
-
The opioid transportation norms provided in the NDPS Rules 2015 can be applied to ensure continuity of pain management IPs who are already on opioid analgesics and have stable pain relief
-
Education, training, and awareness activities can be continued without break, using virtual platforms
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2020. COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum [Internet]. World Health Organization; :7. Available from: https://wwwwhoint/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum Last cited 2020 Jun 17
- Available from: https://wwwundporg/content/undp/en/home/coronavirus/socio-economic-impact-of-covid-19html Last cited 2020 Jun 17
- COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci Total Environ. 2020;728:138882.
- [Google Scholar]
- India under COVID-19 lockdown? Lancet. 2020;395:1315. doi: 10.1016/S0140-6736(20)30938-7. PMID: 32334687; PMCID: PMC7180023
- [Google Scholar]
- Covid-19: India imposes lockdown for 21 days and cases rise. BMJ 2020:368. m1251 Published 2020 Mar 26 doi:101136/bmjm1251
- [Google Scholar]
- Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. J Pain Symptom Manage. 2016;51:1070-90e9.
- [Google Scholar]
- Cancer pain and psychosocial factors: A critical review of the literature. J Pain Symptom Manage. 2002;24:526-42.
- [Google Scholar]
- National Comprehensive Cancer Network? Adult cancer pain. J Natl Compr Canc Netw. 2013;11:992-1022. doi: 10.6004/jnccn.2013.0119. PMID: 23946177; PMCID: PMC5915297
- [Google Scholar]
- Burden of cancer pain in developing countries: A narrative literature review. Clin Outcomes Res. 2018;10:675-91.
- [Google Scholar]
- Cancer patients and research during COVID-19 pandemic: A systematic review of current evidence. Crit Rev Oncol Hematol. 2020;150:102972.
- [Google Scholar]
- Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335-7.
- [Google Scholar]
- eBook on palliative care guidelines for Covid-19 Pandemic 2020 [Internet]. Available from: https://palliumindiaorg/wp-content/uploads/2020/05/Palliative-Care-in-COVID19-Resource-Toolkit-Ebook-V3-1pdf Last cited 2020 Jun 17
- Managing cancer care during the COVID-19 pandemic and beyond Trends. Cancer 2020 pii: S2405-8033 (20) 30135-7
- [Google Scholar]
- Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia. 2020;75:935-44.
- [Google Scholar]
- Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf
- The socio-economic implications of the coronavirus and COVID-19 pandemic: A review. Int J Surg. 2020;78:185-93.
- [Google Scholar]
- Palliative care for advanced cancer patients in the COVID-19 pandemic: Challenges and adaptations. Cancer Res Stat Treat. 2020;3:127.
- [Google Scholar]
- Cancer Management Cancer Control 2015:57.
- Government of India | e-Pass for Movement During Lockdown [Internet]. Available from: http://serviceonlinegovin/epass/ Last cited 2020 Jun 16
- Board of Governors in Supersession of the Medical Council of India Telemedicine Practice Guidelines Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine 2020
- Cancer Care Delivery Challenges Amidst Coronavirus Disease - 19 (COVID-19) Outbreak: Specific Precautions for Cancer Patients and Cancer Care Providers to Prevent Spread. Asian Pac J Cancer Prev. 2020;21:569-73. Published 2020 Mar 1 doi:1031557/APJCP2020213569
- [Google Scholar]
- Recommendations for triage, prioritization and treatment of breast cancer patients during the COVID-19 pandemic. Breast. 2020;52:8-16.
- [Google Scholar]
- The Need for Prioritizing Cancer Surgeries Amidst the COVID-19 Pandemic [published online ahead of print, 2020 Apr 29]? Indian J Surg Oncol. 2020;11:1-2. doi:10.1007/s13193-020-01080-z
- [Google Scholar]
- Coronavirus guidance for clinicians and NHS managers. [Internet]. Available from: https://www.england.nhs.uk/coronavirus/ Last cited 2020 Jun 17
- Teledensity (Per 100 Inhabitants) 2014 [Internet]. Available from: https://dotgovin/sites/default/files/Telecom%20Statistics%20India-2019pdf Last cited 2020 Jun 17
- Adjuvant analgesics in cancer pain: A review. Am J Hosp Palliat Care. 2012;29:70-9.
- [Google Scholar]
- Pharmacological treatment of pain in cancer patients: The role of adjuvant analgesics, a systematic review. Pain Pract. 2017;17:409-19.
- [Google Scholar]
- Nonsteroidal anti-inflammatory drugs and pain in cancer patients: A systematic review and reappraisal of the evidence. Br J Anaesth. 2019;123:e412-e423.
- [Google Scholar]
- The role of paracetamol and nonsteroidal anti-inflammatory drugs in addition to WHO Step III opioids in the control of pain in advanced cancer. A systematic review of the literature. Palliat Med. 2012;26:305-12.
- [Google Scholar]
- A review on the current classification and regulatory provisions for medicines in drug and cosmetic Act, in the light of present day context. Int Arch BioMed Clin Res. 2017;3 I-VIIDOI:1021276/iabcr20173326
- [Google Scholar]
- G.S.R. 359(E) Dated 5th May 2015 Issued Amending the Narcotic Drugs and Psychotropic Substances Rules, 1985, Namely Called the Narcotic Drugs and Psychotropic Substances (Third Amendment) Rules. 2015
- [Google Scholar]
- Evidence for central opioid receptors in the immunomodulatory effects of morphine: Review of potential mechanism (s) of action. J Neuroimmunol. 1998;83:19-28.
- [Google Scholar]
- Going beyond efficacy: Strategies for cancer pain management. Curr Oncol. 2008;15:S41-9.
- [Google Scholar]
- Available from: https://dor.gov.in/link/notification cited 2020 Jun 17
- The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162:276-86.
- [Google Scholar]
- Effects of fentanyl on natural killer cell activity and on resistance to tumor metastasis in rats. Dose and timing study. Neuroimmunomodulation. 2004;11:255-60.
- [Google Scholar]
- Opioids and the management of chronic severe pain in the elderly: Consensus statement of an international expert panel with focus on the six clinically most often used world health organization step III opioids (Buprenorphine, Fentanyl, Hydromorphone, Met. Pain Pract. 2008;8:287-313.
- [Google Scholar]
- Opioid endocrinopathy: A clinical problem in patients with chronic pain and long-term oral opioid treatment. Clin J Pain. 2010;26:374-80.
- [Google Scholar]
- Petition IAPC Letter to MCI Board of Governors. [Internet]. Available from: http://chng.it/gXm88DdMSN Last cited 2020 Jun 17
- Interventional management of cancer pain. Curr Opin Support Palliat Care. 2012;6:1-9.
- [Google Scholar]
- Interventional techniques for cancer pain management. Clin Oncol (R Coll Radiol). 2011;23:407-17.
- [Google Scholar]
- Tramadol? CMAJ. 2013;185:E352. doi: 10.1503/cmaj.121592. Epub 2013 Mar 18. PMID: 23509136; PMCID: PMC3652964
- [Google Scholar]
- Tapentadol hydrochloride: A novel analgesic. Saudi J Anaesth. 2013;7:322-6. doi: 10.4103/1658-354X.115319. PMID: 24015138; PMCID: PMC3757808
- [Google Scholar]
- Treatment of Chronic Pain With Various Buprenorphine Formulations: A Systematic Review of Clinical Studies? Anesth Analg. 2018;127:529-538. doi:10.1213/ANE.0000000000002718
- [Google Scholar]
Appendix

A. Tool for self-reporting of pain intensity score
| “not | “as bad as you can imagine”” | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Nausea, vomiting, and/or lack of appetite | |||||||||||
| Fatigue, sleepiness, trouble concentrating, hallucinations, and/or drowsiness/somnolence | |||||||||||
| Constipation | |||||||||||
| Itching | |||||||||||
| Decreased sexual desire/function and/or diminished libido | |||||||||||
| Dry mouth | |||||||||||
| Abdominal pain or discomfort/ cramping or bloating | |||||||||||
| Sweating | |||||||||||
| Headache and/or dizziness | |||||||||||
| Urinary retention | |||||||||||
(Adapted from: Howard S. Smith, MD. In Smith and Kirsh (2007). Documentation and potential tools in long-term opioid therapy for pain. The Medical Clinics of North America, 91, p. 220-222.)
| …………………………. (Patient’s Name/ Hospital ID number) …………………… | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Date | Average Pain score in NRS | Name and scheduled doses of prescribed medicines/ opioids | Breakthrough dose | Extra dose | ||||||
| Time | Time | Time | Time | Time | Pain Score/ quality | Time | ||||
| Activity check-list: Sleep□Bathe□Feed□Talk□Sit□Work□Stand/Walk Mood………………(description)………………….. | ||||||||||
| Constipation□Any other side effects:……………………………………………………………………………. | ||||||||||
| Pain Goals : Achieved□Variance□ | ||||||||||
| Notes: ……………………………………………………………………………………………………………………………………………………………………………………………………… | ||||||||||






