Translate this page into:
Aspiring Pain Practitioners in India: Assessing Challenges and Building Opportunities
Address for correspondence: Dr. Sushma Bhatnagar, Department of Onco-Anaesthesia and Palliative Medicine, Dr. B.R.A. Institue Rotary Cancer Hospital, All India Institutes of Medical Sciences, New Delhi, India. E-mail: sushmabhatnagar1@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Pain medicine is a developing specialty, aimed at relieving pain and suffering, enhancing function, and improving the quality of life of patients. Pain is often ignored, under-reported and mismanaged by health-care providers. Aspiring pain physicians in India face many challenges and barriers in advancing their specialty.
Objectives:
The objective of this study is to determine the challenges in establishing a pain practice in India and to discuss the opportunities and strategies to overcome these barriers.
Subjects and Methods:
Face-to-face interactive sessions were held with 60 aspiring pain physicians of India who were chosen as registrants to an International Association for the Study of Pain-Indian Society for Study of Pain multidisciplinary evidence-based pain management program conducted at Delhi and Mumbai. The available opportunities, practical issues and the hurdles in becoming a pain specialist were analyzed and summarized in this commentary.
Results:
The major barriers identified were: (1) Inadequate knowledge and absence of structured, educational and training courses, (2) bureaucratic hurdles, and (3) concerns of opioid misuse and addiction. The opportunities for personal growth and that of the specialty that could be utilized include the creation of a pain resource team, increasing community awareness, changing attitudes of other physicians toward pain specialty, and research and evidence building of the effectiveness of pain management strategies.
Conclusion:
India needs a structured teaching and training program in the area of pain medicine that is affiliated by the Medical Council of India or other reputed boards of medical education and certification. There is an urgent need to include pain management in the undergraduate and postgraduate medical curriculum. Enhancing community level awareness by public health education campaigns, developing networks of pain physicians, and appropriate marketing of the specialty is needed to make pain medicine recognized and utilized as a valuable specialty.
Keywords
Barriers
challenges
opportunities
pain
INTRODUCTION
In 2017, the International Association for the Study of Pain (IASP)-Indian Society for Study of Pain (ISSP) Multidisciplinary evidence-based pain management program was conducted for the first time in India, at Mumbai and Delhi. Fifty-five physicians, aspiring to be pain consultants, were chosen to participate in the program which was a unique educational venture that extended for 5 months and included three 2-day face-to-face interactive sessions. The interactive sessions included formal discussions with the aspiring pain physicians of India on the available opportunities and challenges in becoming a pain specialist. Participants represented a range of medical specialties, including, anesthesiology, internal medicine, oral medicine, orofacial pain, oncology, and orthopedics. This article provides an overview of the information gathered from the program participants on practical issues, challenges, and opportunities for future pain medicine aspirants.
PAIN PREVALENCE AND ITS CONSEQUENCES
Pain is often ignored, under-reported, and mismanaged.[12] The worldwide prevalence of pain in the adult population is 20%.[3] As per the World Health Organization (WHO), 15%–17% of Indians suffer from arthritis, 30% have chronic pain, and 25%–30% experience backache. Pain is the most common symptom encountered in cancer and palliative care unit. One-third of patients referred to a tertiary cancer center in India suffer with severe pain.[4] About 70%–80% of cancer patients suffer from moderate to severe pain in their terminal stage.[5] Untreated chronic pain can result in unemployment, disrupted marital status, depression, insomnia, social isolation, financial issues, and loss of self-esteem and have a negative impact on activities of daily living and overall quality of life.[6] Pain is a silent epidemic affecting both the family as well as caregivers.[7] Therefore, timely referral of chronic resistant pain to a pain specialist is important but is often delayed.
Pain relief is a basic human right. It has been termed as the fifth vital sign and should be routinely assessed along with pulse rate, blood pressure, temperature, and respiratory rate.[89] While other vitals can be monitored and managed efficiently by most physicians, the careful assessment, and management of pain require a trained pain specialist. Dealing with the biopsychosocial problems of pain is a challenging task. Despite the critical role of pain medicine in the well-being of the patient, this specialty is under-utilized and under-appreciated. Flowchart 1 describes the vicious cycle of delayed referral and under-utilization of pain specialists.
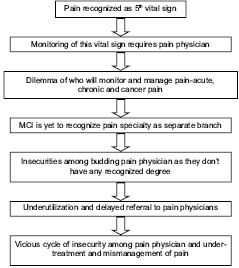
- Vicious cycle of delayed referral and underutilization of pain specialty
PAIN MEDICINE AS A SPECIALTY
Pain medicine is the specialized branch of healthcare that deals with providing comprehensive management of acute, chronic and cancer pain, using multidisciplinary strategies that include pharmacological, interventional, and psychological approaches. The main goal of this specialty is to improve the overall quality of life and the functional status of the patient with pain. In developed nations, physicians with a variety of backgrounds can be trained in "pain medicine," but its proper definition and which branch or physician is responsible for it is still unclear in India.
A major advance in the field of pain was the description of the gate control theory in 1965 by Patrick Wall and Ronald Melzack. With the establishment of the IASP in 1975, Pain Medicine has made considerable advances and has attracted many young physicians to this field. The introduction of the WHO three-step analgesic ladder for pain relief in 1986, has been a significant step in the development of the concept of pain medicine as an individual specialty.[10]
CONCEPT OF THE PAIN CLINIC
A pain clinic fulfills the unmet needs of patients in the current medical system and helps patients to deal with their chronic and difficult pain that has not responded to the conventional treatments. It provides a holistic approach and deals with all the components of pain-physical, social, psychological, financial, cognitive, and vocational aspects.
Pain clinics should be able to utilize a vast range of applications, ranging from simple outpatient department medical management to interventional modalities. Anatomically, pain may present in any location from head to toe, and can have varying etiologies and present as headache, postherpes zoster, post-stroke pain spasticity, trigeminal neuralgia, neck pain, cancer pain, neuropathic pain, shoulder pain, chronic abdominal pain, back pain, sciatica, herniated disc, and failed back surgery syndrome.
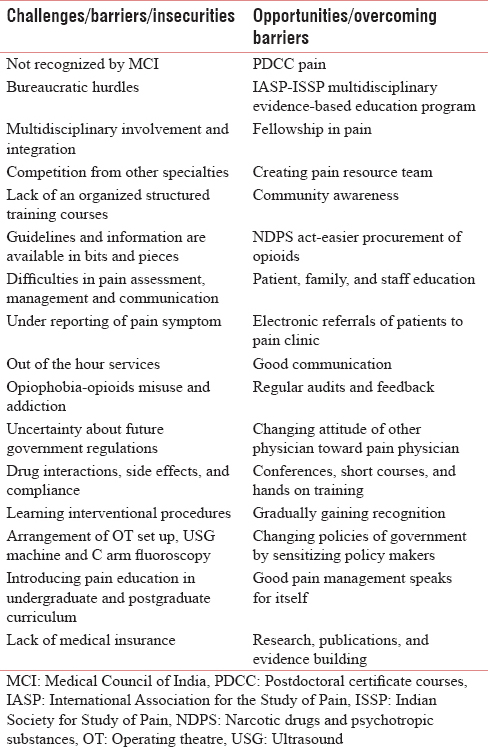
As shown in Table 1, a summary of the practical issues and the challenges and the opportunities to overcome such hurdles that were voiced by many of the aspiring pain physicians and discussed by the faculty at IASP-ISSP multidisciplinary evidence-based pain management program.
CHALLENGES, INSECURITIES, AND BARRIERS IN BECOMING A PAIN SPECIALIST
Pain Medicine is not recognized by MCI as a specialty
The Medical Council of India (MCI) is yet to recognize pain medicine as a separate specialty. This results in insecurity among the pain physicians as they do not have any recognized degree. Moreover, pain medicine is not considered as a worthwhile independent branch as pain is considered as a symptom and not a disease. Moreover, most physicians practicing pain management are early in their careers, and the branch is yet to be established.
Bureaucratic hurdles
Pain management is not well supported by the hospital administration or bureaucracy. Changing the thought process of the medical fraternity is a major hurdle. Communication and learning to convince family, patients, colleagues, policymakers, and administrative department plays a major role in establishing supportive patients and loyal teams.
Multidisciplinary involvement and integration
Pain physicians are rightly labeled as "jack of all trades and master of none." It is a shared branch. Multidisciplinary integration of the pain clinic is required with psychology, anesthesiology, neurology, neurosurgery, rheumatology, orthopedics, interventional radiology, palliative medicine, and oncology. It requires back up support from physiotherapy, nursing, clinical psychology, occupational therapy, behavior science, and physical medical rehabilitation being represented. Collaborating with home-care team is also required. Thus, pain clinic should be accessible and working within the complex of multidisciplinary teams. Recruitment of new patients is facilitated by collaborating with nearby medical practitioners, but building this team is a challenging job. Moreover, patients have more confidence in their primary treating physicians and developing their trust and confidence takes significant effort.
Competition from other specialties
Because of the overlap of this branch, there may be competition from other specialties and reluctance to refer patients to the pain clinic. Pain physicians are also looked down by other branches and recognized as an underrated field.
Lack of organized structured training courses
Most pain physicians in India are anesthetists as they are trained to manage acute postoperative surgical pain. The anesthetists have to come out of their comfort zone of the operation theatre and move to a completely different environment that requires face-to-face interaction with the patients. Leaving their core branch and moving onto a new unrecognized specialty requires considerable courage, struggle, and determination. The anesthetists have to face the challenge of obtain training in pain as there is presently no structured format for learning in pain medicine. Some anesthetists practice both anesthesia and pain medicine and hence have to divide their time among both professions. This may lead to instability in their profession. Setting up an independent pain clinic is an enormous task. The first hurdle for the budding pain physicians is to obtain adequate training and knowledge for practicing pain medicine.[11]
Guidelines and information are available in bits and pieces
Pain medicine is an evolving specialty and pain physicians have to constantly update their knowledge as the guidelines and evidence keep changing. Pain physicians should also have expertise regarding nonpharmacological and complementary management of pain. Inadequate knowledge presents a significant barrier in treating difficult pain problems.[5] The practicing pain consultant should be competent and up-to-date on new developments, advances in the medical practice or changes in medical or legal regulations. Information booklets or pamphlets to both the patients and the physicians should be made available to create an awareness regarding pain clinics.
Difficulties in pain assessment, management, and communication
Pain is a neurophysiological process with psychosocial consequences and its mechanisms are complex. Pain physicians face difficulties in pain assessment, clinical examination, diagnosis, management, and counseling.[12] Pain assessment is perceived to be the most common barrier in pain optimization by 49.7% physicians.[13] Pain may have multiple etiologies, diffuse effects, and numerous management strategies. Long-term follow-up is required for chronic pain patients. Every patient is unique and different, and this introduces dilemmas in treating the individual patient based on existing evidence. A single disease has varied treatment choices and there may be difference in opinion regarding management. The pain physician has to deal with the patient suffering from pain, rather than physical pain alone. This includes the additional role of counseling and prognosticating which are challenging and time-consuming tasks.
Under reporting of pain symptom
Pain is not considered as a life-threatening condition and thus ignored by patients until it becomes persistent and significantly affects their daily life.
After hour services
Pain specialist has to make their own identity and maintain that reputation by proving their work to patients and families. Pain physician should provide informed decision-making, psychological support and counsel patients at each contact time. Sincere efforts and hard work by pain physicians are needed to provide after hour services. Feedback, self-reflection, and self-motivation should be done regularly. Gordon et al. have concluded that the regular audit of benefits of pain management should be done to improve the quality of pain treatment.[14]
Opiophobia-opioid misuse and addiction
The pain clinic is often misperceived as an opioid clinic. Pain management encompasses many other options and interventions, rather than prescribing morphine alone. Opioid availability, government regulations, and its associated stigma are barriers for opioid prescription.[1516] Dealing with the myth regarding morphine as a symbol of terminal stage of cancer is another issue. These kind of superstitious beliefs stop patients from climbing the ladder of pain relief. Widespread opioid abuse and misuse has been reported recently, hindering the free prescription of opioids in the USA and many other countries. Opioid addiction is spreading like an epidemic and hence these drugs must be prescribed safely with precautions. There may be under prescription of drugs because of associated side effects. Fear of undue side effects of analgesics is the most common reported barrier (45%) in practicing pain medicine.[17] Patients and their family members must be educated regarding opioids misuse, addiction, and proper storage of drugs.
Uncertainty about future government regulations
Procurement of opioids was very difficult until the amendment of the Narcotic Drugs and Psychotropic Substances Act. Still, there is uncertainty about future government regulations. Thus, proper documentation, record keeping and follow-up is required for safe and effective use of morphine.
Drug interactions, side effects and compliance
Analgesics, such as nonsteroidal anti-inflammatory drugs, are also misused and lead to side effects such as gastritis, gastric bleeding, and kidney failure. Combination of drugs may also lead to drug interactions, additive side effects, and difficulty in maintaining compliance to multiple drugs.
Learning interventional procedures
Interventional pain procedures have several potential advantages such as immediate pain relief that could last for long duration, procedures as an outpatient or daycare, no requirement of anesthesia, can be repeated and performed in patients who are high-risk candidates for surgery. Newer technologies include intrathecal implants, neurostimulation, vertebroplasty, and drug delivery pumps. Learning interventional procedure is an art. It requires focus, patience, and experience. In a study, the major barriers in cancer pain management education were interventional procedures, palliative interventions, and dealing with the postoperative and procedural pain.[18] Certain pharmacological and interventional procedures are experimental, and benefits are yet to be documented. Moreover, satisfying patients expectations and demand of their magical relief of pain is a big challenge.
Arrangement of operation theater set up, ultrasound machine and C-arm
Considerable capital expense and administrative procedures are needed for the purchase of C-arm fluoroscopy and obtaining permission to use ultrasound machine as per Preconception and Prenatal Diagnostic Techniques Act.
Introducing pain education in undergraduate and postgraduate curriculum
There is a dearth of pain education at undergraduate and postgraduate levels and hence a big challenge in India is improving education in pain among medical professionals.[1920] Similarly, Mezei et al. concluded that pain education is provided in fragmented manner and they proposed integration of pain subjects in medical colleges.[21]
Lack of medical insurance
Pain physicians also have to face the problem of maintaining reimbursement for interventional procedure for chronic pain as there is lack of medical insurance for these procedures.
SOURCES OF LEARNING FOR ASPIRING PAIN PHYSICIANS
The sources of learning for young pain physicians are cadaveric workshops, lectures, learning labs, panel discussion, continuing medical educations, web-based teaching, conferences, programs, short courses, meetings, expert guest lectures, newsletters, seminars and hands-on training. However, at present, there is a lack of organized, structured training courses, and definite guidelines in India.[13]
AVAILABLE OPPORTUNITIES
Postdoctoral certificate courses in Pain recognized by MCI is being provided only at two places in India-Banaras Hindu University, Varanasi that started in 2008 and Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow which was started in 2010. A 1-year fellowship in pain has been started this year (2017) by ISSP and will train only 2 candidates per year. Hence, one would have to be exceptionally talented to be selected for this fellowship.
FUTURE RECOMMENDATIONS
India needs a structured teaching and training program in the area of Pain Medicine which needs to be affiliated and recognized by the Medical Council of India or other reputed boards of medical education and certification. For the initial 5-year period, we can utilize a selected group of existing trained and experienced pain physicians as faculty for this program till core group of pain physician recognized by this course are available.
There is an urgent need to create our own protocols and policies that are developed based on high-quality multicenter research in areas of chronic pain management protocols and policies established on studies in western populations may need to adapted to our patient populations, based on studies in the Indian population. Additional prospective, randomized, double-blind studies to provide high-quality evidence to support the use of various interventions in a specific population of patients with chronic pain are needed.
For the endorsement by Government of India, we can propose to merge pain management programs with existing palliative care programs as it has already been proven that integration of pain and palliative care improves quality of life.[22]
There is an urgent need to include pain management in undergraduate and postgraduate curriculum.
CONCLUSION
Pain management is a fundamental human right. It should be treated as the fifth vital sign throughout the country as it is the most common presenting complaint in the majority of the ailments resulting in visits to the hospital. It is a moral duty of every physician to follow the path of humanity to decrease sufferings among cancer and chronic pain patients. Although there are many challenges and problems, pain specialty is growing slowly day–by-day in this country. However, we are a long way from having pain medicine blossom into a successful recognized specialty. Spreading community level awareness by public health education campaigns and developing networks of pain physician and proper marketing is needed to make this important specialty recognized and utilized appropriately. Hopefully, pain medicine will be recognized in the near future and would help improve the life of patients with intractable pain. Let's fight together and follow the motto of-"Drain the pain for better tomorrow."
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge the IASP and ISSP for starting this wonderful initiative. We also want to thanks all the participants of IASP-ISSP Multidisciplinary Evidence-Based Pain Management Program and the faculties involved in the conduct of the program for giving their time and support and making this program successful.
REFERENCES
- Physician attitudes and practice in cancer pain management. A survey from the eastern cooperative oncology group. Ann Intern Med. 1993;119:121-6.
- [Google Scholar]
- Cancer pain management by radiotherapists: A survey of radiation therapy oncology group physicians. Int J Radiat Oncol Biol Phys. 2000;47:203-8.
- [Google Scholar]
- International Association for the Study of Pain, Unrelieved pain is a major global healthcare problem. 2012. Available from http://www.iasp-pain.org/AM/Template.cfm?Section=Home&Template=/CM/ContentDisplay.cfm&ContentID=2908
- [Google Scholar]
- The prevalence of severe pain, its etiopathological characteristics and treatment profile of patients referred to a tertiary cancer care pain clinic. Indian J Palliat Care. 2015;21:148-51.
- [Google Scholar]
- Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol. 2008;19:1985-91.
- [Google Scholar]
- Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11:1859-71.
- [Google Scholar]
- Pain intensity, quality of life, quality of palliative care, and satisfaction in outpatients with metastatic or recurrent cancer: A Japanese, nationwide, region-based, multicenter survey. J Pain Symptom Manage. 2012;43:503-14.
- [Google Scholar]
- Pain as a human right: The 2004 global day against pain. J Pain Palliat Care Pharmacother. 2005;19:85-100.
- [Google Scholar]
- Palliative care as an international human right. J Pain Symptom Manage. 2007;33:494-9.
- [Google Scholar]
- Validation of World Health Organization guidelines for cancer pain relief: A 10-year prospective study. Pain. 1995;63:65-76.
- [Google Scholar]
- Provision of training in chronic pain management for specialist registrars in the United Kingdom. Anaesthesia. 1999;54:761-8.
- [Google Scholar]
- Pain assessment: The cornerstone to optimal pain management. Proceedings (Bayl Univ Med Cent). 2000;13:236-9.
- [Google Scholar]
- Current practices in cancer pain management in Asia: A survey of patients and physicians across 10 countries. Cancer Med. 2015;4:1196-204.
- [Google Scholar]
- American pain society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med. 2005;165:1574-80.
- [Google Scholar]
- A survey on physician knowledge and attitudes towards clinical use of morphine for cancer pain treatment in China. Support Care Cancer. 2010;18:1455-60.
- [Google Scholar]
- Physicians’ attitudes to clinical pain management and education: Survey from a Middle Eastern Country. Pain Res Manag 2016 2016:1358593.
- [Google Scholar]
- Minding the gaps in cancer pain management education: A multicentre study of clinical residents and fellows in a low versus high-resource setting. J Glob Oncol. 2016;2:387-96.
- [Google Scholar]
- Current pain education within undergraduate medical studies across Europe: Advancing the provision of pain education and learning (APPEAL) study. BMJ Open. 2015;5:e006984.
- [Google Scholar]
- Training medical students to manage a chronic pain patient: Both knowledge and communication skills are needed. Eur J Pain. 2006;10:167-70.
- [Google Scholar]






