Translate this page into:
Cost Analysis on Total Cost Incurred (Including Out-of-pocket Expenditure and Social Cost) During Palliative Care in Cases of Head-and-Neck Cancer at a Government Regional Cancer Centre in North India
*Corresponding author: Saurabh Singh, MBBS, MD, Department of Hospital Administration, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India. saurabhhsinghh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Harsvardhan R, Arora T, Singh S, Lal P. Cost analysis on the total cost incurred (including out-of-pocket expenditure and social cost) during palliative care in cases of head-and-neck cancer at a Government Regional Cancer Centre in North India. Indian J Palliat Care 2022;28:419-27.
Abstract
Objectives:
Palliative care involves providing symptomatic relief from the pain and stress of a severe illness to markedly improve the quality of life for both the patients and their families. It imposes high indirect costs on the patients. The study was conducted at SGPGIMS, which caters to 500 head-and-neck cancer patients annually. Out of these, 30–40% of cases require dedicated palliative care. Unfortunately, often, when patients reach the stage of palliative care, they have exhausted their all financial reserves. Therefore, a cost analysis of total cost incurred (including out-of-pocket expenditure and social cost) during palliative care in cases of head-and-neck cancer at a Government Regional Cancer Centre was undertaken.
Material and Methods:
The study is a descriptive study and the study sample consisted of (a) patients who had undergone surgery, chemotherapy, or radiotherapy and had recurred/relapsed and were now candidates for palliative care and (b) patients who presented de novo to the Regional Cancer Centre, SGPGIMS with advanced-stage disease, where the cure was not possible. The expenditure incurred was obtained retrospectively and prospectively from the study samples.
Results:
The out-of-pocket expenditure per patient per day was INR 2044.21. The social cost per patient per day was INR 518.21. Out of the total expenditure of INR 2562.42/patient/day, 80% of the cost was out-of-pocket expenditure and the remaining 20% was social cost borne by the patient.
Conclusion:
The study thus added to perspective on the average expenditure on out-of-pocket expenses and social costs being incurred as of date, while getting palliative care for head-and-neck cancer at a Regional Cancer Centre.
Keywords
Cost analysis
Total cost
Out-of-pocket expenditure
Social cost
Palliative care
INTRODUCTION
Globally, head-and-neck cancer is the seventh most common cancer and out of the total burden, a majority is contributed by developing countries.[1] Head-and-neck cancer includes cancers of the paranasal sinuses, nasal cavity, oral cavity, pharynx, and larynx. Consuming alcohol and chewing tobacco are prime risk factors for developing head-and-neck cancers.[2]
India has a high burden of head-and-neck cancer and one-third of the cases are male. A majority (60–80%) of head-and-neck cancer cases report to the healthcare facility when the disease is in an advanced stage.[3,4] In India, one-third out of all the cases of cancers are head-and-neck cancer which is higher as compared to 4–5% in the developed world.[5] In Asia, there has been a drastic increase in the number of deaths due to cancers in past two decades. In the past one and a half decade, India’s population as compared to rest of the world has grown twice as percentage of increase, which has also resulted in the increase in the burden of the cancer in India.[4] Cancer treatment requires a multidisciplinary approach; however, many advanced cancer patients are candidates for palliative treatment.
Primarily, palliative care involves providing symptomatic relief from pain and stress of a severe illness so as to markedly improve the quality of life for both the patients and their families.[6] It is offered either as upfront care when the disease is diagnosed in advanced stages or when the disease has recurred or spread following radical treatment (and when all salvage options have been exhausted).
The treatment of cancers is cost-intensive as it involves the use of multiple modalities, such as surgery, chemotherapy, radiotherapy, imaging, and laboratory services.[7] Therefore, an enormous financial burden is imposed on payers (government or patient and their families) for the provision of treatment and care to cancer patients. In India, out of the total healthcare expenditure, the government contributes around 29% and the rest is contributed by patients or their families as an out-of-pocket expenditure.[8] Annually, in India, 3.5–6.2% of such households go below the poverty line due to such high out-of-pocket expenditure and as compared to communicable diseases, the chances of households going below the poverty line from financial burden due to provisioning cancer care and treatment are sky-high.[9,10]
The treatment of cancer involves massive indirect costs apart from direct treatment costs associated with it. About 70% of cancer deaths reported in India were from the age group 30– 69 years.[11] Various factors such as distance from the medical facility, availability of mode of transportation, and financial condition of the patient and their families burden them, leading to delay in early diagnosis and treatment of cancer. Most of the family budget of cancer patients and their families is utilised in availing treatment of cancer, thereby, imposing a financial burden on them. Apart from that, wage or income loss due to days off from work has an adverse impact on the economic well-being of such households.[12]
According to the WHO, ‘Out-of-pocket expenditures are defined as direct payments made by individuals to health-care providers at the time of service use. It excludes any prepayment for health services, such as taxes or specific insurance premiums or contributions and, where possible, net of any reimbursements to the individual who made the payments.’[13] Therefore, these are the expenses that must be paid directly to the healthcare provider by the insured without a third party (insurer or government).[14]
According to Letter, ‘the social cost is the sum of the private costs resulting from a transaction and the costs imposed on the consumers due to being exposed to the transaction for which they are not compensated or charged.’[15] The costs incurred by the producer to produce goods or services are known as private costs. Social cost includes private costs and external costs which are related to producing goods for which the free market does not account. Therefore, mathematically, social marginal cost is the aggregate of private marginal cost and external costs.[16]
The knowledge regarding the costs associated with the provision of palliative care to patients with head-and-neck cancer, apart from various approaches to record these costs in such cases is sparse.[17] In India, out-of-pocket payments are the predominant way to finance healthcare services, which imposes a financial burden on the households and can lead to impoverishment and catastrophe.[18]
We at SGPGIMS see 500 head-and-neck cancer patients annually. Of these, 30–40% of cases require dedicated palliative care. Unfortunately, often, when patients reach the stage of palliative care, they have exhausted all financial reserves. Therefore, a cost analysis of total cost incurred (including out-of-pocket expenditure and social cost) during palliative care in cases of head-and-neck cancer at a Government Regional Cancer Centre was undertaken.
MATERIAL AND METHODS
Study design
A descriptive study was undertaken in the Palliative Care Clinic of a Government Regional Cancer Centre, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India. The study sample consisted of head-and-neck cancer patients undergoing palliative care at Palliative Care Clinic (SGPGIMS, Lucknow, India).
Data acquisition
Initially, 15 patients were tagged and followed from Palliative Care Clinic to each point of contact from where the patient received the services, to design the structured data acquisition tool. The patients and their caregivers were also interviewed to determine the complete process map of the palliative care pathway for the head-and-neck cancer patients along with the review of records. The study samples were recruited when they reported at Palliative Care Clinic registration. Thereafter, the study samples were followed up at the start of their treatment and were interviewed every time they visited Palliative Care Clinic during the study period. Patients were also interviewed and followed 1-month post the study period when the patient and the accompanying caretaker visited Regional Cancer Centre, SGPGIMS. The study sample consisted of (a) patients who had undergone surgery, chemotherapy, or radiotherapy and had recurred/relapsed and were now candidates for palliative care and (b) patients who presented de novo to the Regional Cancer Centre, SGPGIMS with advanced-stage disease, where the cure was not possible. The expenditure incurred was obtained retrospectively and prospectively from the study samples.
The study samples were interviewed in the Palliative Care Clinic during their follow-up visits. As per the department protocol, patients with head-and-neck cancer were required to visit the Palliative Care Clinic once every month to document the disease status, modify drugs and replenish drugs. In addition, payment receipts and bills were checked, where available, to validate the reported expenditure. A sample size of 50 patients was taken for the study.
Study method
The complete process map of the palliative care pathway for the head-and-neck cancer patients was determined by obtaining information from patients and their caregivers and a review of the record [Figure 1]. Initially, 15 head-and-neck cancer patients visiting Palliative Care Clinic, SGPGIMS were followed from Palliative Care Clinic to each point of contact from where the patient received the services. Their record was evaluated to map the palliative care pathway and finalise the structured data acquisition tool for data acquisition, identifying cost centres, cost sub-centres, and cost elements in the process map of the palliative care pathway.

- Process map of palliative care pathway from cost and accountancy perspective.
The structured data acquisition tool was formulated for estimating the total cost including out-of-pocket expenditure and social costs during palliative care in cases of head-and-neck cancer patients. The patients and their relatives were interviewed on their social demographic characteristics, household expenditure, and out-of-pocket expenditure on diagnosis/treatment of head-and-neck cancer. If the patient had received any treatment before visiting the Palliative Care Clinic, SGPGIMS, the expenditure regarding the same was also recorded to compute the total cost of palliative care using a structured data acquisition tool.
The cost was classified into (a) direct expenses: Which included the expenditure on the diagnosis, drugs/consumables, hospitalisation and procedure fee were considered. Apart from that, the expenses for transportation, boarding, loading and food were taken as a direct non-health-care expenditure and (b) indirect expenses: Which included wage or income loss by the patient and accompanying caretaker during the period of treatment. Thereafter, the total cost was computed from the data obtained from the structured data acquisition tool.
The total cost thus computed using the structured data acquisition tool was analysed to identify the out-of-pocket expenditure and social cost.
Written patient information document was distributed and informed consent was obtained from the study sample before data acquisition.
RESULTS
Sample characteristics
Fifty patients with head-and-neck cancer undergoing palliative care at Palliative Care Clinic aged 33–80 years were recruited for the study. The median age was 47 years [Figure 2]. In the recruited sample, 12 (24%) patients were aged between 30 and 40 years, 16 (32%) patients were aged between 41 and 50 years. At the same time, 10 (20%) were aged 51–60 years. Followed by 7 (14%) patients aged between 61 and 70 years were found, 5 (10%) were 71–80 years [Figure 3]). The patients in the study were majorly males, 44 (88%), with only 6 (12%) females [Figure 4]. Males were younger between 30 and 50 years as compared to females who were 40 years or older [Figure 5]. Eighteen (36%) of the patients had completed secondary school, 16 (32%) of the patients were less than high school [Figure 6]. The state of residence of the patients was Uttar Pradesh in 47 (94%) of the total patients, followed by Bihar in 2 (4%) cases and only 1 (2%) from Madhya Pradesh [Figure 7].

- Age group of the patients.
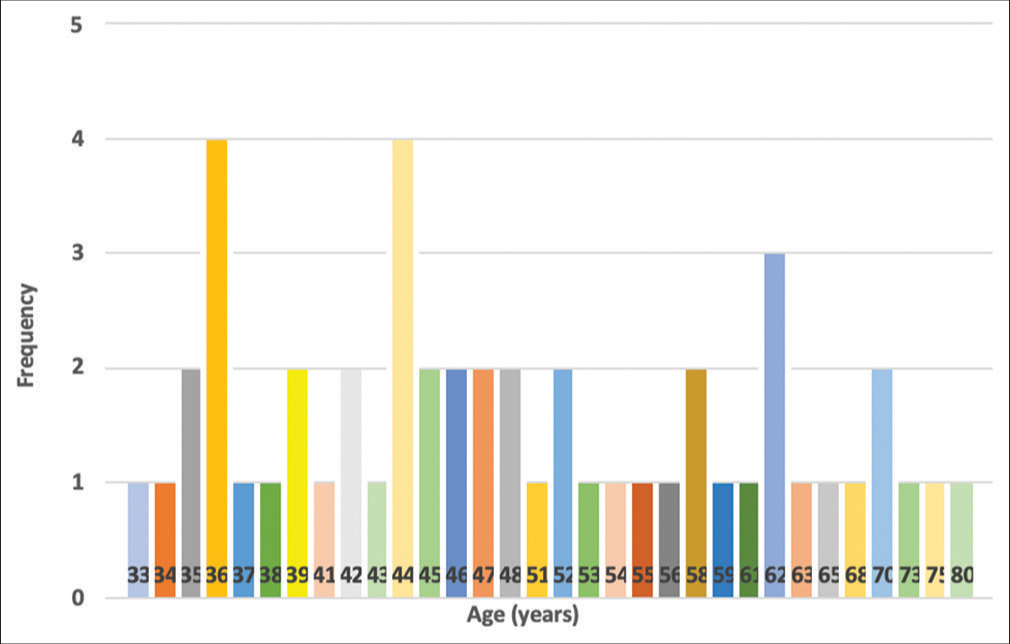
- Age distribution of the patients.
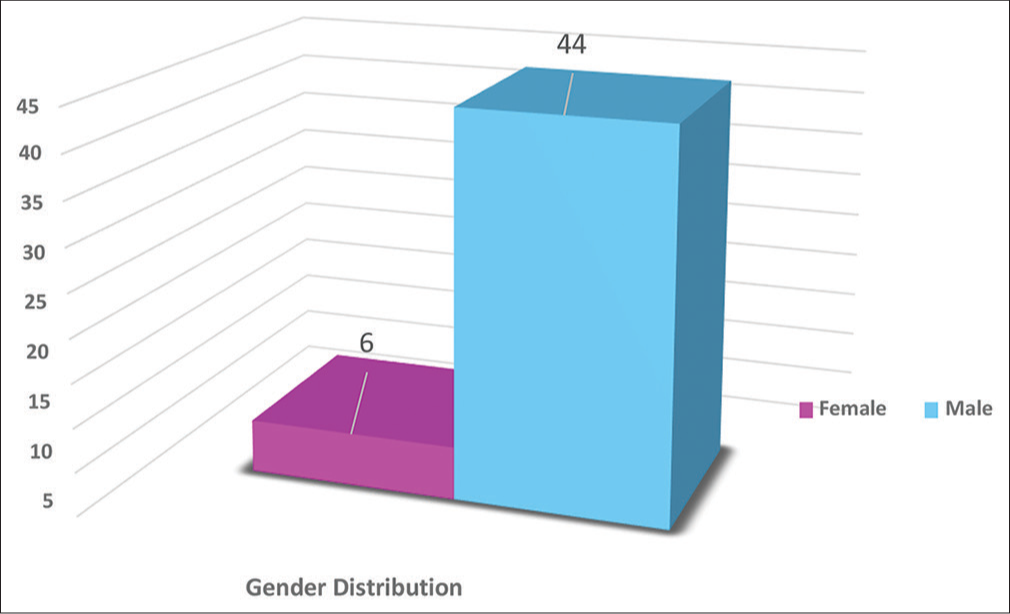
- Gender distribution of the patients.
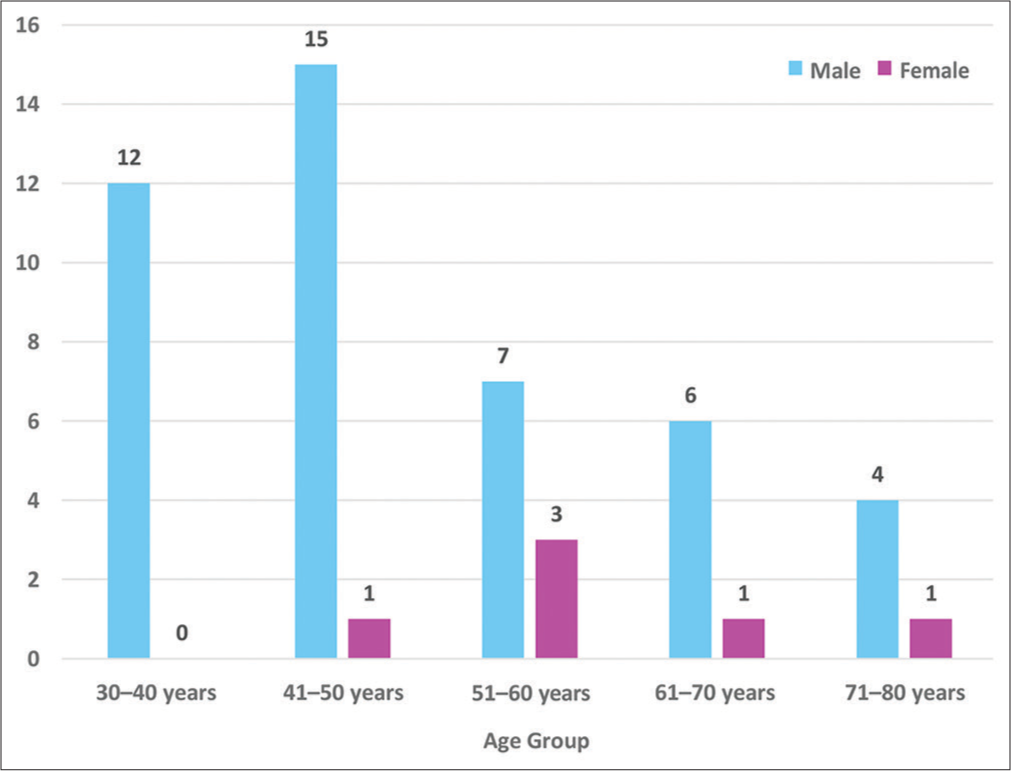
- Age group distribution of the patients.
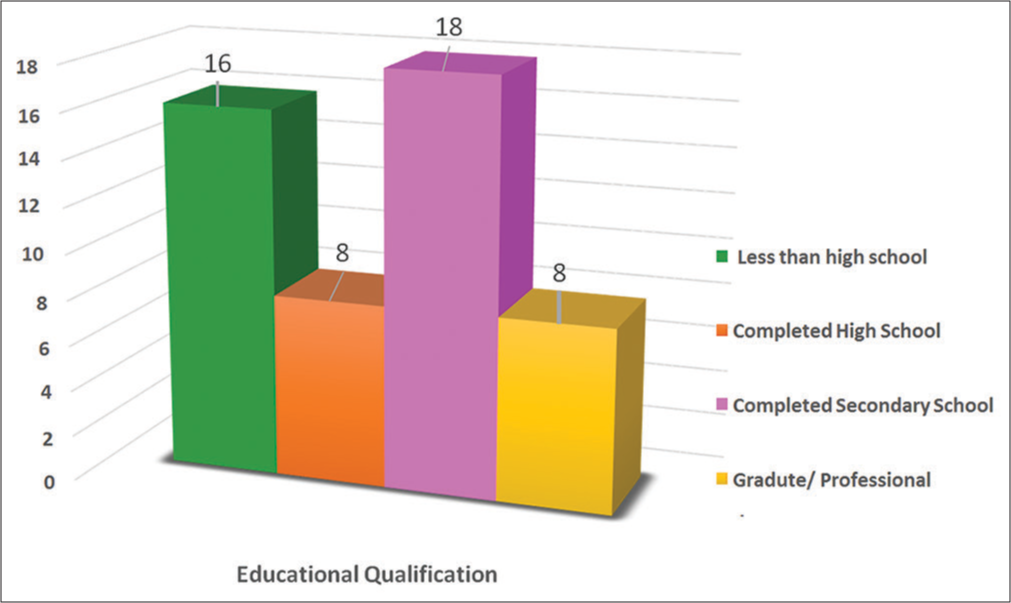
- Educational qualification of the patients.
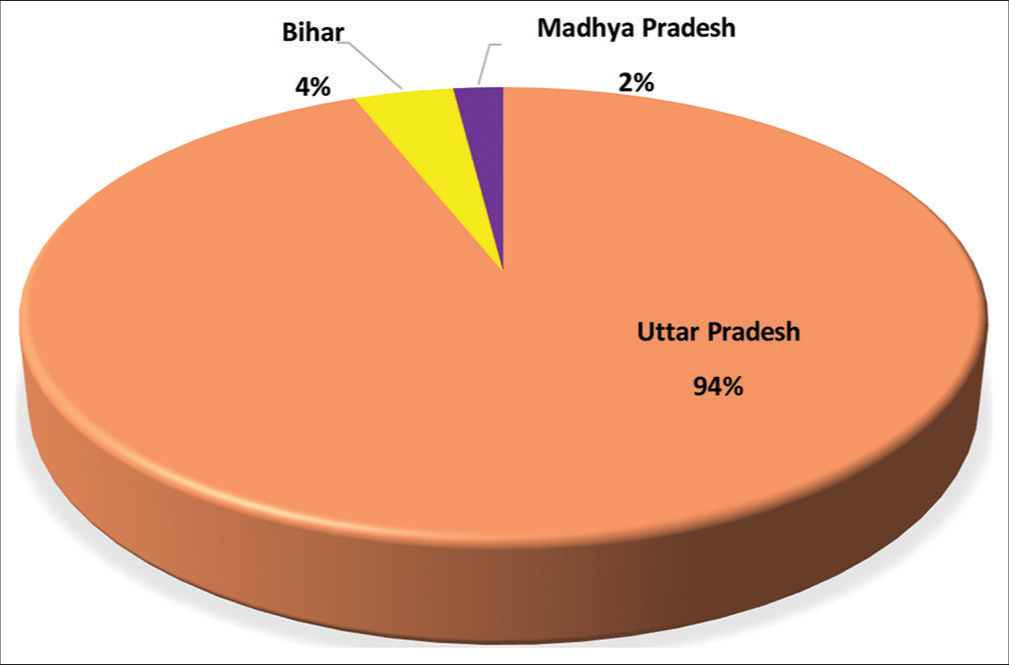
- State of residence of the patients.
Out-of-pocket expenditure per patient per day
The out-of-pocket expenditure borne per patient per day was computed by adding the treatment cost (the expenditure on all the diagnosis, medications, consumables, injections and administration of injection), the expenditure on transportation, the expenditure on accommodation and expenditure on food and consumables borne by the patient for Palliative treatment at Palliative Care Clinic, SGPGIMS. Finally, the total expenditure per day was computed by the per month data collected for all the variables.
The treatment cost (expenditure on all the diagnosis, medications, consumables, injections and administration of the injection, including palliative RT) per patient per day is computed to be INR 1580.76 (77%). The expenditure on transportation per patient per day was INR 375.30 (18%). The expenditure on accommodation paid per patient per day during his/her stay for palliative therapy at Palliative Care Clinic was INR 53.54 (3%). The expenditure on food and consumables paid per patient per day during his/her stay for palliative therapy at Palliative Care Clinic, SGPGIMS was INR 34.61 (2%). Therefore, the out-of-pocket expenditure borne per patient per day was deduced to be INR 2044.21 [Table 1 and Figure 8].
| S. No. | Characteristics | Amount (INR) | % |
|---|---|---|---|
| 1. | Total Treatment Cost (Expenditure on all the diagnosis, medications, consumables, injections and administration of the injection, including Palliative RT) per day (n=50) | 79,038.36 | 77% |
| Treatment Cost (Expenditure on all the diagnosis, medications, consumables, injections and administration of the injection, including Palliative RT) per patient per day | 79,038.36÷50=1580.76 | ||
| 2. | Total Expenditure on transportation per day (n=50) | 18,765.07 | 18% |
| Expenditure on transportation per patient per day | 18,765.07÷50=375.30 | ||
| 3. | Total expenditure on accommodation paid per day during his/her stay for palliative therapy at Palliative Care Clinic (n=50) | 2677.35 | 3% |
| Expenditure on accommodation paid per patient per day during his/her stay for palliative therapy at Palliative Care Clinic | 2677.35÷50=53.54 | ||
| 4. | Total expenditure on food and consumables paid per day during his/her stay for palliative therapy at Palliative Care Clinic (n=50) | 1730.68 | 2% |
| Expenditure on food and consumables paid per patient per day during his/her stay for palliative therapy at Palliative Care Clinic | 1730.68÷50=34.61 | ||
| Total out-of-pocket expenditure per day (n=50) | 102,211.35 | ||
| Out of Pocket expenditure per patient per day (INR) | 102,211.35÷50=2044.21 | ||
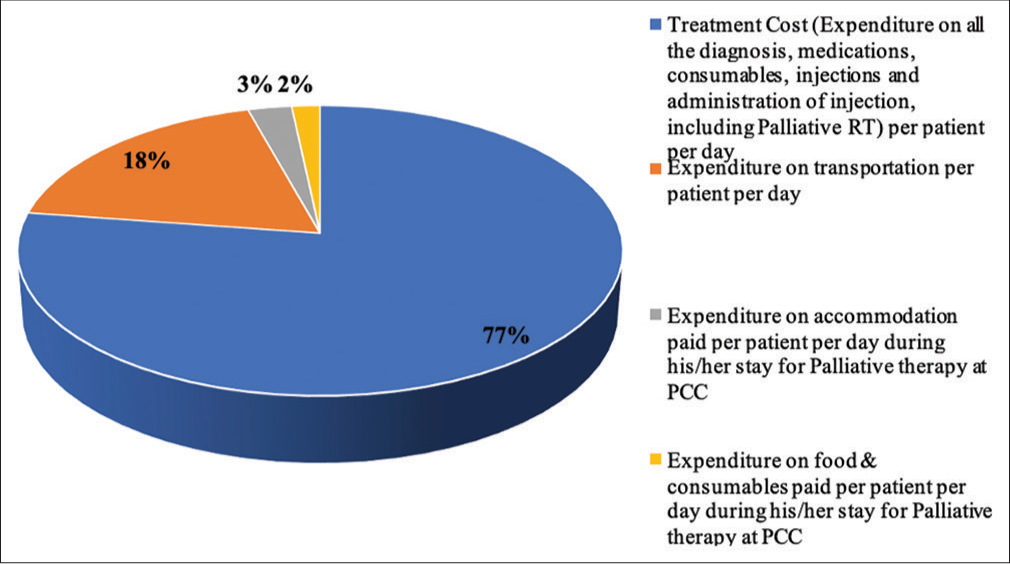
- OOPE per patient per day (INR).
Social cost per patient per day
The social cost per patient per day was computed by subtracting the number of days spent per patient for palliative treatment at Palliative Care Clinic, SGPGIMS from the monthly salary or the wage per day per patient. Therefore, the social cost per day was computed by the per month data collected.
The salary or pension per patient per day was deduced to be INR 522.73. The wage per patient per day was deduced to be INR 318.42. The social cost borne per patient per day was deduced to be INR 518.21 [Table 2].
| S. No. | Characteristics | Amount (INR) |
|---|---|---|
| 1. | Total salary or pension per day (n=44) | 23,000.15 |
| 2. | Salary or pension per patient per day | 23,000.15÷44=522.73 |
| 3. | Total wage per day (n=6) | 1910.52 |
| 4. | Wage per patient per day | 1910.52÷6 =318.42 |
| Total social cost per day (n=50) | 25,910.63 | |
| Social cost per patient per day (INR) | 25,910.63÷50=518.21 | |
Total cost
The total cost per patient per day was computed by adding the out-of-pocket expenditure per patient per day and social cost per day for the palliative treatment at Palliative Care Clinic, SGPGIMS. The total expenditure borne per patient per day was computed to be INR 2562.42 for the palliative treatment at Palliative Care Clinic, SGPGIMS. Out of the total expenditure of INR 2562.42/patient/day, 80% of the cost was out-of-pocket expenditure and the remaining 20% was social cost borne by the patient. Summary of the total cost is listed in [Table 3 and Figure 9].
| S. No. | Characteristics | Amount (INR) | Percentage |
|---|---|---|---|
| 1. | OOPE per patient per day | 2044.21 | 80 |
| 2. | Social cost per patient per day | 518.21 | 20 |
| Total cost per patient per day (INR) | 2562.42 | ||
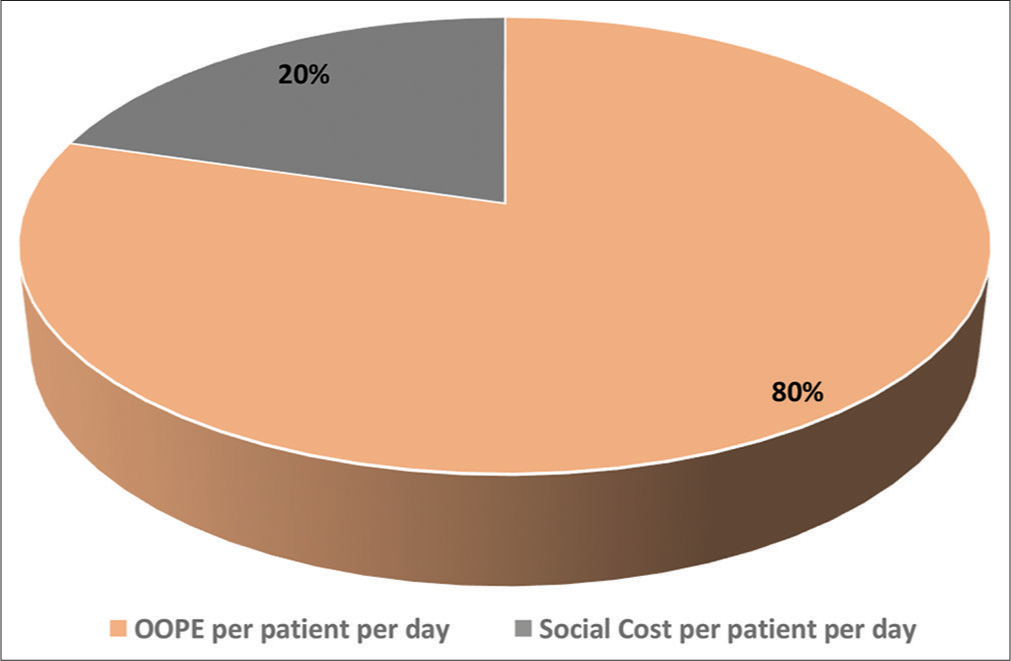
- Total cost per patient per day (INR).
DISCUSSION
An increase in the burden of cancer and the cost-intensive diagnosis and treatment of cancer has led to an increase in the cost of diagnosis, treatment, and palliative care for cancer in India.[8] The diagnosis of cancer is already a burden for the patient. It becomes devastation due to the financial drain faced by the families because of the nature of its treatment. To reduce out-of-pocket expenditure, various publicly sponsored health insurance schemes were introduced by the Indian government across many states. However, the outof-pocket expenditures incurred by the patients were not reduced by these schemes.[12]
This study was undertaken to do the cost analysis of total cost incurred (including out-of-pocket expenditure and social cost) during palliative care in cases of head-and-neck cancer. We found that the total expenditure borne per patient per day was INR 2562.42 for the palliative treatment at Palliative Care Clinic, SGPGIMS. This study was undertaken at a Government Regional Cancer Centre in North India. A total of 50 study samples were recruited for the study, fulfilling the inclusion criteria. All the study samples were followed up at the start of their treatment and were interviewed every time they visited Palliative Care Clinic during the study period. The majority of the patients (88%) in the study were male. Of the 12% of females in the study, 50% were from the age group of 51–60 years. This finding is similar to the findings in the recent study conducted by Chauhan et al., 2019 and Mohanti et al., 2011.[12,17-19] Oral squamous cell carcinoma is the most prevalent cancer in males and the third most prevalent cancer in females in India, due to chewing of tobacco products.[20,21] In the recruited sample, 34% of males were between 41 and 50 years old. This finding is similar to the findings in a recent study conducted by Chauhan et al., 2019 and Mohanti et al., 2011.[12,17-19] The risk of developing head-and-neck squamous cell carcinoma increases as the age advances; therefore, the majority of head-and-neck squamous cell carcinoma develops in patients aged 50 years or more. The average age for developing head-and-neck squamous cell carcinoma related to smoking and smokeless tobacco is 60 and 78 years, respectively.[22]
Regarding educational qualification, 36% of the sample had completed secondary school only. The majority of the patients recruited for the study were Class IV employees (26%), followed by 22% farmers and 12% housewives. A similar study by Al-Dakkak, 2010, shows the high risk of cancer in individuals living in the most deprived areas, unemployed and with a low level of educational attainment.[23] The patients reported at the study hospital are residents from Uttar Pradesh 94%, Bihar 4% and 2% of cases from Madhya Pradesh in the catchment area. The patient had to pay for transportation in an Indian scenario where the patient traveled a long distance to the tertiary care facilities.[19]
In 40% of the patients, the initial treatment received was >12 months before. About 80% of patients reported receiving initial treatment at private health facilities for cancer-related diseases [Figures 10 and 11], which is in line with a study by Nair et al., 2014. This divulges that there is apathy in the primary healthcare system in India for cancer control activities, specifically in rural areas, thereby compelling the patients to visit private healthcare facilities.[24] Private healthcare facilities provide a far better level of comfort to the patient and their relatives as compared to public healthcare facilities.[25]
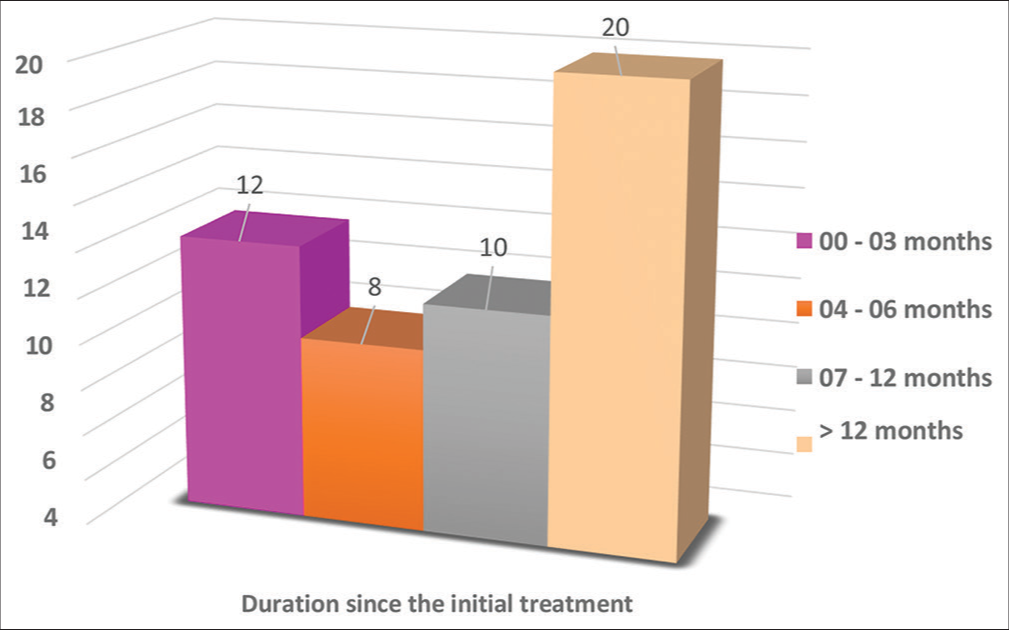
- Duration since the initial treatment received by the patients before reporting to PCC, SGPGIMS.
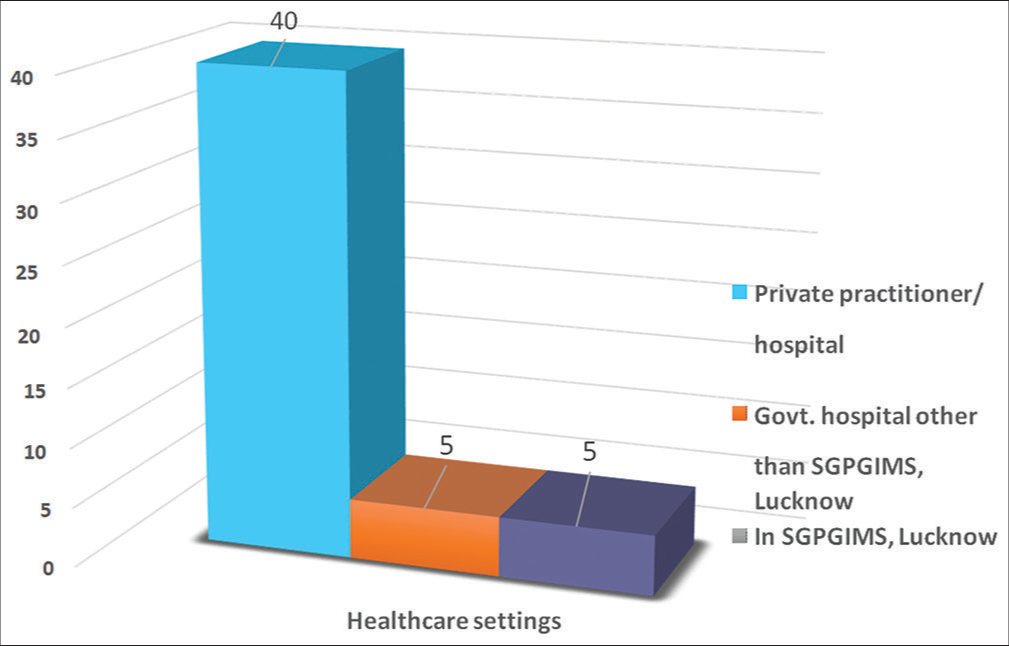
- Health-care settings where the initial treatment was received by the patients before reporting to PCC, SGPGIMS.
The total expenditure incurred in the study was INR 2562.42/ patient/day, out of which 80% constituted the out-of-pocket expenditure, of which 23% was spent on transportation, food and lodging and 77% on medical expenses. As per the study by Himmelstein et al., 2009, excessive out-of-pocket expenditure accelerates the inequitable financial burden and unintended consequences such as sacrificing the spending by the household or incurring debt, which will result in the household becoming bankrupt.[26] Due to excessive out-of-pocket expenditure, patients and their relatives delay, skip or economise the treatment, medicines and other consumables, as shown in the study by Karaca-Mandic et al., 2010; Wang et al., 2011; Balabanova et al., 2012; and Eaddy et al., 2012, which results in poor health outcomes.[27-30] Cost-sharing is typically seen in patients with chronic ailments, the elderly and patients who are poor.[30-36]
According to the NSS 71st round, the average out-of-pocket expenditure in India has doubled from the similar survey conducted in 2004–2005.[37,38] The availability of cancer treatment in India is linked with inequities in access to health care due to scarce resources and irregular distribution of cancer treatment across the country.[39] This is also reflected in 23% of the overall out-of-pocket expenditure incurred on travel, boarding and lodging in the present study. About 40% had to travel by a rented taxi or own car as the patient’s poor health makes him/her unable to travel through public transport. A male attendant mostly accompanied the patients to Palliative Care Clinic, SGPGIMS, which again is an expense due to that person’s time lost or wage lost. In 28% of the cases, the patient was accompanied by the patient’s son and 22% by the patient’s brother. The patient was accompanied by another adult to the Palliative Care Clinic.[40]
Apart from transportation, 34% of the patients had to arrange for lodging in a hotel or a guest house. Furthermore, the food adds up to the burden in 30% of the cases. It leads to the patient paying out of his pocket even if they had health insurance. These expenses are not covered under the insurance. Nearly, 70% of the cancer patients in the study faced a financial burden during the treatment, a finding similar to Nair et al., 2014. The financial problems lead the low-income families to usually delay their treatment decision. The patients belonging to low-income families face financial burdens in the form of debt or loss of family income attributable to excessive out-of-pocket expenditure for availing care and treatment for cancer. The treatment of cancers has become more effective, which is attributable to the improvement in technology over a period of time; however, the high cost of technology has resulted in the rapid increase in the costs of diagnosis and treatment.[18]
In the study, the patient had to borrow money from 60% of the total recruited sample. Based on NSS, 2004–2005 round, 50% of the households borrowed and sold their assets to bear the high out-of-pocket expenditure in availing care and treatment of cancer. This finding is akin to the finding in our study.[41] Further, the high-income households are less dependent on borrowing money or selling their assets to meet their healthcare expenditure as compared to low-income households as shown in the 71st round of NSS.[37] The study by Mohanti et al., 2011 brought out that to continue the treatment patients and their relatives had to sell off their property and borrow heavily. About half of the families in the study faced financial burden and catastrophic expenditure and one-fourth of the family went below the poverty line attributable to excessive out-of-pocket expenditure in availing treatment and care for cancer.[19]
Families with low-income shell out a high percentage of their family income on availing of health care as compared to the families with high income, which validates that outof-pocket expenses are regressive.[42-45] To ensure universal access to curative services at healthcare facilities, financial protection must be provided to poor patients and their families. At present, in India, government-funded health insurance has managed to indemnify the patients and their families with low income. However, these health insurance schemes do not indemnify against out-of-pocket expenditure to avail outpatient care.[12]
More than half (52%) of the patients who had undergone other forms of treatment before undergoing palliative therapy meet an exorbitant expenditure of INR > 60,000. The families of low-income cancer patients are pushed into impoverishment and financial catastrophe due to the excessive cost of treatment for cancer which is multimodal dependent on the type of cancer and stage of cancer.[12]
This study brings out that only 22% of patients had enrolled under any scheme for financial reimbursement for expenditure on the treatment received at Regional Cancer Centre, SGPGIMS. The financial burden on such patients can be markedly reduced, if, the higher number of such patients enroll under any financial assistance schemes. It was also observed that the families with a low income had sparse knowledge regarding financial assistance schemes and procedures to avail benefit from such schemes. Their sparse knowledge can be attributed to families with low income not availing of financial support through such schemes.
The patients (82%) were unemployed when under the care of the palliative team. Many had a salary/pension of INR 10,001–25,000 per month with 03–06 members in the family. In comparison, 12% were daily wage workers. For 84% of the case, patients had 00–02 earning members in their family with a total family income of INR <10,000/month in 46%. Only 10% of the patients had a family income of INR >60,000 per month. Few patients were unable to pay school fees for their children leading to children dropping out of school.
The social cost was INR 518.21/patient/day (20%) of the total cost in this study which is attributable to the loss of wage of the patient and their family members. This finding is similar to the findings in a study by Nair et al., 2014.[24] Out of the total, 36% of patients had paid INR 25,001–60,000 for the palliative therapy, while the highest amount of INR 60,001– 100,000 was paid by 14% of the total.
CONCLUSION
The study aimed to do a cost analysis of total cost incurred (including out-of-pocket expenditure and social cost) during palliative care in cases of head-and-neck cancer at the Government Regional Cancer Centre in North India. The cost centres and sub-centers were identified from the process map and the cost was categorised into health service costs and non-health service costs. The total expenditure borne per patient per day was computed to be INR 2562.42 for the palliative treatment at Palliative Care Centre, SGPGIMS. Out of the total expenditure, 80% of the cost was out-of-pocket expenditure and the remaining 20% was social cost borne by the patient.
This study added to perspective on average expenditure including out-of-pocket expenditure and social cost being incurred as of date, while getting palliative care for head-and-neck cancer, at a Government Medical Institute, where the rate of health-care delivery may not be competitive. A multicentric study across public and private healthcare facilities may help design and recommend an ideal package for palliative care, for financial assistance schemes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-86.
- [CrossRef] [PubMed] [Google Scholar]
- Head and Neck Cancer Risk Factors and Prevention. 2020. Available from: https://www.cancer.net/cancer-types/head-and-neck-cancer/risk-factors-and-prevention [Last accesses on 28 Apr 20]
- [Google Scholar]
- Head and neck cancer: Global burden and regional trends in India. Asian Pac J Cancer Prev. 2014;15:537-50.
- [CrossRef] [PubMed] [Google Scholar]
- Head and neck cancers in developing countries. Rambam Maimonides Med J. 2014;5:e0009.
- [CrossRef] [PubMed] [Google Scholar]
- Head and neck oncology: The Indian scenario. South Asian J Cancer. 2016;5:104-5.
- [CrossRef] [PubMed] [Google Scholar]
- Get Palliative Care. 2020. Available from: https://getpalliativecare.org/whatis [Last accessed on 28 Apr 20]
- [Google Scholar]
- Evidence Based Management of Guidelines in India: Guidelines for Head and Neck Cancer, Vol X1 (Part A) In: General Principles and Outline of Management. Mumbai: Tata Memorial Centre; 2012. p. :1-8.
- [Google Scholar]
- Effect of payments for health care on poverty estimates in 11 countries in Asia: An analysis of household survey data. Lancet. 2006;368:1357-64.
- [CrossRef] [Google Scholar]
- The economic impact of noncommunicable diseases on households in India. Global Health. 2012;8:9.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer mortality in India: A nationally representative survey. Lancet. 2012;379:1807-16.
- [CrossRef] [Google Scholar]
- Economic burden of head and neck cancer treatment. North India Asian Pac J Cancer Prev. 2019;20:403-9.
- [CrossRef] [PubMed] [Google Scholar]
- Geneva: World Health Organization. 2020. Available from: https://www.who.int/health_financing/topics/financial-protection/out-of-pocket-payments/en [Last accessed on 29 Apr 20]
- [Google Scholar]
- Out-of-Pocket Expense. 2020. Available from: https://en.wikipedia.org/wiki/Out-of-pocket_expense [Last accessed on 29 Apr 20]
- [Google Scholar]
- Environmental Economics: An Introduction New York: McGraw-Hill Book Company (UK) Ltd.; 1994. p. :52.
- [Google Scholar]
- What cost components are relevant for economic evaluations of palliative care, and what approaches are used to measure these costs? A systematic review. Palliat Med. 2017;31:323-37.
- [CrossRef] [PubMed] [Google Scholar]
- Equity in health care financing in low and middle-income countries: A systematic review of evidence from studies using benefit and financing incidence analyses. PLoS One. 2016;11:e0152866.
- [CrossRef] [PubMed] [Google Scholar]
- Estimating the Economic Burden of Cancer at a Tertiary Public Hospital: A Study at the All India Institute of Medical Sciences New Delhi, India: Indian Statistical Institute; 2011.
- [Google Scholar]
- Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45:309-16.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in head and neck cancer incidence in relation to smoking prevalence: An emerging epidemic of human papillomavirus-associated cancers? Cancer: Interdisciplinary Int J Am Cancer Soc. 2007;110:1429-35.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral Maxillofac Surg Clin North Am. 2014;26:123-41.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic status and head and neck cancer. Evid Based Dent. 2010;11:57-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cost of treatment for cancer: Experiences of patients in public hospitals in India. Asian Pac J Cancer Prev. 2013;14:5049-54.
- [CrossRef] [PubMed] [Google Scholar]
- Private or Government Hospital: Which one would you Prefer? 2020. Available from: https://www.careerride.com/view/private-or-government-hospital-which-one-would-you-prefer-17663.aspx [Last accessed on 28 Jul 20]
- [Google Scholar]
- Medical bankruptcy in the United States, 2007: Results of a national study. Am J Med. 2009;122:741-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cost sharing, family health care burden, and the use of specialty drugs for rheumatoid arthritis. Health Serv Res. 2010;45:1227-50.
- [CrossRef] [PubMed] [Google Scholar]
- Does medication adherence following a copayment increase differ by disease burden? Health Serv Res. 2011;46:1963-85.
- [CrossRef] [PubMed] [Google Scholar]
- Health care reform in the former Soviet Union: Beyond the transition. Health Serv Res. 2012;47:840-64.
- [CrossRef] [PubMed] [Google Scholar]
- How patient cost-sharing trends affect adherence and outcomes: A literature review. P T. 2012;37:45-55.
- [Google Scholar]
- Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285:421-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of increased patient cost sharing on socioeconomic disparities in health care. J Gen Intern Med. 2008;23:1131-6.
- [CrossRef] [PubMed] [Google Scholar]
- Is the level of patient co-payment for medicines associated with refill adherence in Sweden? Eur J Public Health. 2014;24:85-90.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Medicaid drug-payment limits on admission to hospitals and nursing homes. N Engl J Med. 1991;325:1072-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: A longitudinal analysis. Med Care. 2010;48:87-94.
- [CrossRef] [PubMed] [Google Scholar]
- Key Indicators of Social Consumption in India Health. NSS 71st Round (January to June 2014) National Sample Survey Organisation.
- [Google Scholar]
- Morbidity, Health Care and the Condition of the Aged In: NSS Sixtieth Round, January-June 2004 (Report No. 507). 2006.
- [Google Scholar]
- National cancer control programme in india: proposal for organization of chemotherapy and systemic therapy services. J Glob Oncol. 2017;3:271-4.
- [CrossRef] [PubMed] [Google Scholar]
- Economic cost analysis in cancer management and its relevance today. Indian J Cancer. 2009;46:184-9.
- [CrossRef] [PubMed] [Google Scholar]
- The economic burden of cancers on Indian households. PLoS One. 2013;8:e71853.
- [CrossRef] [PubMed] [Google Scholar]
- Increasing expenditure on health care incurred by diabetic subjects in a developing country: A study from India. Diabetes Care. 2007;30:252-6.
- [CrossRef] [PubMed] [Google Scholar]
- Coping with health-care costs: Implications for the measurement of catastrophic expenditures and poverty. Health Econ. 2008;17:1393-412.
- [CrossRef] [PubMed] [Google Scholar]
- A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low-and middle-income countries. PLoS One. 2011;6:e20821.
- [CrossRef] [PubMed] [Google Scholar]
- Economic burden of coronary heart disease in North India. Int J Noncommun Dis. 2016;1:18.
- [CrossRef] [Google Scholar]






