Translate this page into:
Developing a Training Course for Spiritual Counselors in Health Care: Evidence from Iran
Address for correspondence: Dr. Alireza Heidari, Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran. E-mail: alirezaheidari7@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Spiritual health can cause mental health promotion and well-being of the people's lives but it is still neglected in practice so that there is no trace of spiritual training in medical education in Iran. This study was conducted to develop a training course for spiritual counselors in the Iranian health-care system.
Methods:
In this qualitative study, senior managers of the Ministry of Health (MOH) and experts in the related fields were purposively selected as the participants. Semi-structured interviews and focused group discussions (FGDs) were conducted to collect the data. After transcription of the interviews and FGDs, the data were analyzed using content analysis.
Results:
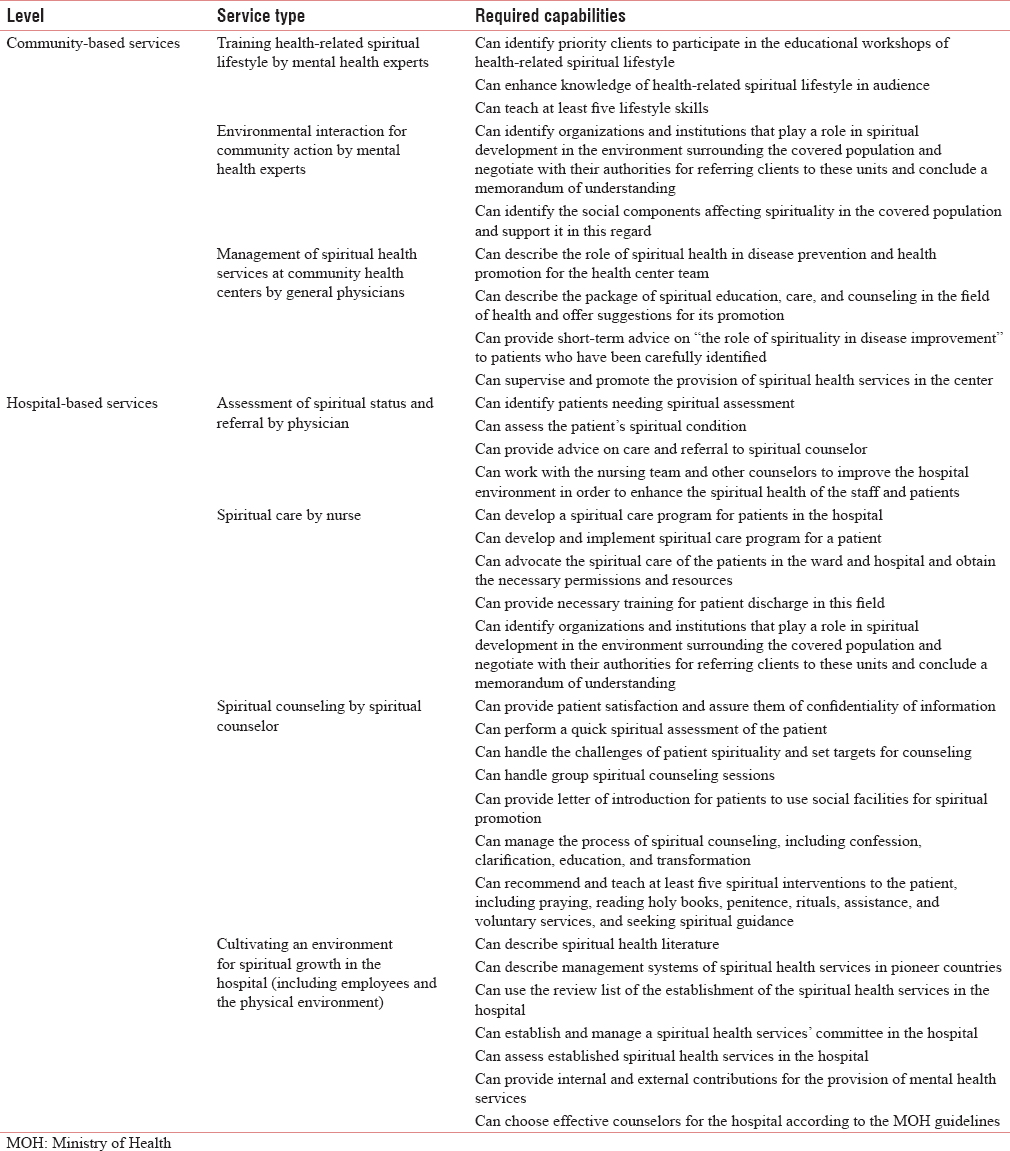
In this package, community-based spiritual health services are offered in three forms of spiritual lifestyle education, introducing social facilities, and collaborating with the related organizations. Hospital services are offered in four forms of assessment of the spiritual status and referral, spiritual care, spiritual counseling, and providing a spiritual environment in the hospital.
Conclusion:
According to the results of the study, it is suggested that a strategic committee be established at the MOH level for establishment of these training courses as well as another strategic committee for evaluation, review, and service package promotion, and its training courses should be formed. In addition, a set of skills for spiritual assessment of patients and the related interventions should be designed for clinical skill centers of the country in the form of skill training packages.
Keywords
Health care
religion
spiritual counseling
spiritual health
training course
INTRODUCTION
Spiritual health, with social, psychological, and physical dimensions, is known as the fourth dimension of health and includes existential and religious dimensions of life. Religious health is the satisfaction that comes from being associated with God, and the existential health is defined as attempts to understand the meaning and purpose of life and obtain satisfaction from it.[12]
Religion and spirituality have a positive impact on health outcomes, including improving depression and protecting against chronic depression. Spiritual health has a positive and significant correlation with better mental health and a reverse relationship with loneliness, frustration, and alcohol and drug abuse; it also improves the ability to manage stress [3] and is considered a common strategy to deal with problems.[4] The importance of spirituality in health care has increased in the recent years. Researchers and practitioners now perceive spirituality as a patient's need that requires a special attention, especially for interdisciplinary palliative services. Strong evidence has shown that patients with serious illnesses and those who live at the end of life may have a strong desire to access and enrich the spiritual aspect of their lives. According to the National Cancer Network, religious and spiritual support is associated with improved patient satisfaction with medical care. On the contrary, spiritual distress is associated with poor physical outcomes and higher rates of illness. In addition, lack of spirituality in severe patients may lead to more emotional anxiety, severe pain, and fatigue, increased burden of the disease, and decreased quality of life.[5]
Although according to the World Health Organization (WHO) definition of palliative care, spiritual care is a major component of palliative care and patients have spiritual needs and are willing to discuss their spiritual beliefs with their physicians, the spiritual dimension of patients and the provision of spiritual care remains one of the neglected aspects. While people have little experience about the balance of the mind, body, and spirit in dealing with emotional stress, physical illness, or death, they try to maintain their faith in their values and beliefs in dealing with illnesses. Therefore, it is very important to provide patients with their spiritual needs to achieve mental health and improve the quality of life.[678] The health-care system needs to provide spiritual responses and pay attention to this aspect of the patients' health. This is confirmed by studies that show patients' needs in this regard.[9] When patients enter an unfamiliar environment, the care system should appoint a person for this purpose and give him/her the necessary training. Patients should be aware of the person who can help them. When a patient is involved in treatment activities, (s)he spends a lot of time thinking about the meaning of life and the experience of the disease. Physical interactions can dramatically change the patient's experiences and his/her future attitude and behavior. In every group and culture, there is a relationship with God and common sources of power that defines the purpose of the patient's life and by which the patient tolerates the sufferings of the disease.[10] Due to a clinical relationship between spirituality and its strong effects on health outcomes, it is essential for all health-care professionals on the palliative care team (doctors, nurses, clergies, therapists, and social workers) to be well educated about the spiritual concerns of patients.[5]
Although Iran has been among active countries in the field of science production in the recent years, it ranks sixth in health and spirituality publications. However, there is no evidence that these studies have led to health-care programs in the health-care system. One of the reasons for not paying attention to spirituality in the field of health services is lack of training in this field. Accordingly, the entry and integration of spirituality in existing curricula has long been emphasized as a serious need. Despite the importance of this issue and the presence of related values in Iran's strategic plans, it is still neglected in practice, so there is no trace of spiritual training in Iranian medical education. The development of such training programs requires the establishment of a coherent framework that is consistent with the national and regional requirements of each country.[11]
Today, many countries in the world, including the UK, Sweden, and Canada, have service packages for providing spiritual health services, but there is still no clear definition of the spiritual health service to be provided in Iran, and no curative training program has been developed for spiritual health counseling. This study was conducted to develop a joint educational program for spiritual counselors for providing evidence-based spiritual services in accordance with Iranian conditions and culture in health-care centers.
METHODS
The present study was a qualitative study with a content analysis approach. The participants were senior managers of health, medical, social, nursing, and educational departments and experts in the field of religious sciences, psychology, psychiatry, and social medicine in the Ministry of Health (MOH). In this research, a purposive sampling approach was applied using the snowball method. The participants' knowledge and experience in providing spiritual services and their interest in participating in research were used as the inclusion criteria. To design a data collection tool, an interview guideline was employed based on the results of the review of the literature as well as the conceptual framework of the study.
The data were collected using focused group discussions (FGDs) and individual in-depth interviews. Authenticity and rigor of the data were confirmed by some criteria such as credibility, dependability, conformability, and transferability. To increase credibility, triangulation, member checks and the allocation of sufficient time to data collection were used. The transcripts were reviewed again and additional comments were received from controllers. To increase transferability, appropriate samples were selected and the data were collected and analyzed simultaneously. To improve dependability, the data were analyzed by different researchers and external observers, and similar results were obtained. To increase conformability, the participants were explained about the entire research process, from the beginning to the end.
To conduct FGDs, the research team invited participants and announced the topic of the meeting, the objectives, and time and place of the group discussion sessions. Participants freely expressed their views during the sessions. A coordinator balanced the discussions, guided them, and focused on the dynamics of the group. To conduct the interviews, after making arrangements for the interviewees, an appointment was scheduled. The place of the interview was selected in such a way that the participants felt comfortable. The interviews were conducted at the predetermined time and place by the researchers. Before the interview, the purpose of the study was fully explained to the participants.
The criteria for completing FGDs and interviews were data saturation and failure to collect new data. The participants were assured about data confidentiality before the interviews were recorded. The interviews were recorded with the permission of the interviewees. The participants were assured of the confidentiality of their information. During FGDs and interviews, issues such as time control for each question, the rhythm of the discussion, and attention to nonverbal communications were considered to assist in data analysis. The recordings were transcribed as soon as possible. Finally, data were analyzed using content analysis and thematic analysis.
RESULTS
The package of “spiritual education, care, and counseling services” was designed in two basic and specialized sections.
In the basic section, community-based spiritual health services are provided in three forms in the health posts, health houses, and community health service centers:
-
Teaching health-related spiritual lifestyle to the covered population, individuals at risk, and chronic patients
-
Introducing social facilities related to clients, training nongovernmental organizations, charity foundations, and volunteers
-
Collaboration of the center with organizations and institutions responsible for planning and monitoring spiritual services affecting health and creating popular social networks.
In the specialized section, spiritual health services are presented in four forms in hospitals and clinics:
-
Identifying patients requiring spiritual counseling by general physicians and specialists
-
Providing spiritual care for patients and facilitating it by nurses
-
Training the hospital staff by reference groups
-
Counseling in the spiritual counseling unit.
The spiritual health services and the required capabilities in health centers are presented in Table 1.
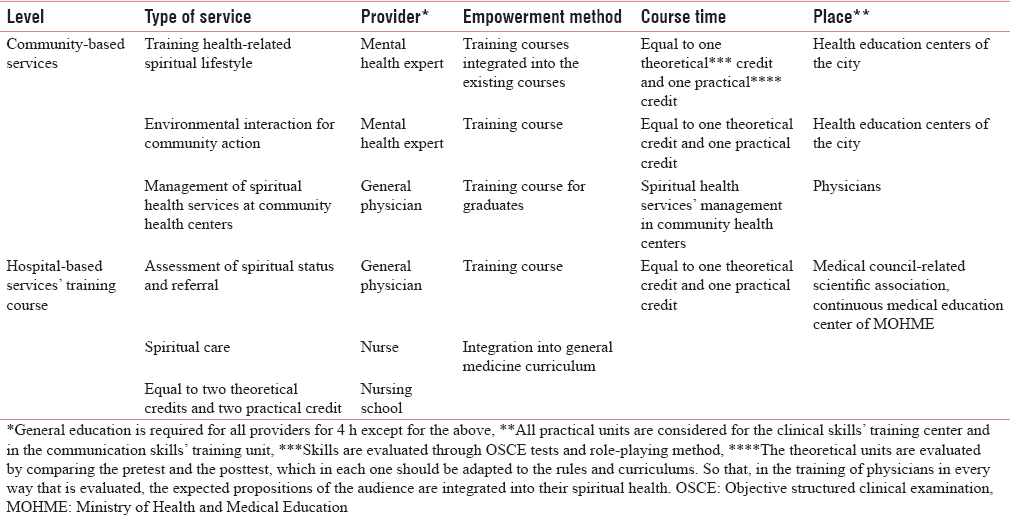
This service package includes training objectives and mode and time of service delivery and evaluation. Personnel involved in spiritual services are mental health experts and general physicians in community health centers, as well as specialist physicians, nurses, and hospital managers in specialized centers. Table 2 shows the empowerment and training of the providers of spiritual health services in health centers.
DISCUSSION
In this package, community-based spiritual health services are offered in three forms of spiritual lifestyle education, introducing social facilities, and collaborating with related organizations. Previous studies have also showed that spirituality promotes the mental health and well-being of people.[12131415] As cultural variables, spirituality and religious participation affect attitudes, behaviors, and health choices (e.g., alcohol consumption, food choices, organ donation, and concepts of guilt and care), communication with providers, and health promotion. With the initiation of research on spirituality and health and codification of ethical and professional guidelines for comprehensive patient-centered care, the medical schools began integrating spirituality and health courses into their curricula. The American College of Medical Colleges (AAMCs), the WHO, and the Joint Accreditation Commission for Health Services recommend spirituality in clinical care and education.[16] Many Western medical universities have integrated spirituality into their curriculum. Religious institutions can be used as a venue for organizing health programs or can be considered active partners in health promotion programs. Religious organizations may have committees that are dedicated to health-related issues. Providers can collaborate with these organizations to help people to increase health information by sponsoring health exhibitions.[17] Most of the patients in a study by Balboni et al. reported that they were strongly supported by religious associations.[18] Spirituality should have a place in the health-care system and be part of the usual care.[19]
In this package, hospital services are offered in four forms of assessment of the spiritual status and referral, spiritual care, spiritual counseling, and providing a spiritual environment in the hospital. In a study by Puchalski et al. in the United States in 2014, the capabilities and expectations of medical students included spirituality in patient care, spiritual evaluation, issues related to spiritual care of patients, and referral to religious experts.[20] One of the main goals of the AAMC for students is to learn how to take spiritual history as part of the patient's history and use it for diagnosis of the disease.[11]
Physicians who are aware of spiritual health strategies as health-care facilitators can encourage patients to play a more prominent role in the overall health. Since the debate about spiritual concerns related to health issues is controversial and is not an official part of clinical education, physicians may feel that they are not prepared for such discussions with patients.[16] Deal stipulates that spiritual care requires a patient-centered approach that does not require complex interventions and can only be provided with simple interventions such as listening to the patient, praying, and not imposing beliefs on the patient to respond to spiritual needs.[21] However, a study conducted in Brazil showed that lack of time and awareness, lack of proper education, and fear of worsening the patient's problems were the main obstacles to the implementation of such programs.[22] Saad and de Medeiros suggest five stages to implement spiritual support programs: deep institutional involvement, official staff training, infrastructures, fund adjustment of organizational politics, and agreement with religious leaders.[23]
This study also had limitations. Access to all stakeholders and experts was not possible. Since there may be resistances at the time of establishment, an action research method should be used in order to overcome this problem. Moreover, service providers were not included in the study; however, their viewpoints may not be relevant and precise in the design level due to their low level of knowledge about spirituality. However, later in the implementation phase, periodic evaluations can be used to attract the participation of all service providers.
CONCLUSION
According to the results, it is suggested that a strategic committee be established at the level of the MOH for establishment of these training courses under the title “Integration of Spiritual Care in the Health System.” Since no specific structure is responsible for spiritual health promotion in the MOH and this task has been distributed among deputies and units in the MOH, a strategic committee should be responsible for evaluation, review, and service package promotion and its training courses. Furthermore, a set of skills for spiritual assessment of patients and related interventions should be designed for Clinical Skills Centers in the form of skill training packages.
Financial support and sponsorship
This study was financially supported by the mental health department of the Ministry of Health and Medical Education (MOHME) and School of Behavioral Sciences and Mental Health of Iran University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to thank the mental health department of the MOH and Medical Education and Faculty of Behavioral Sciences and Mental Health for their financial and management supports.
REFERENCES
- Inequalities in the spiritual health of young Canadians: A national, cross-sectional study. BMC Public Health. 2016;16:1200.
- [Google Scholar]
- Relationship between spiritual health and quality of life in patients with cancer. Asian Pac J Cancer Prev. 2015;16:7321-6.
- [Google Scholar]
- An exploration of the status of spiritual health among nursing students in Taiwan. Nurse Educ Today. 2010;30:386-92.
- [Google Scholar]
- Relationship between different dimensions of prayer and spiritual health of patients treated with hemodialysis. Iran J Crit Care Nurs. 2010;2:149-52.
- [Google Scholar]
- Increasing the number of outpatients receiving spiritual assessment: A Pain and palliative care service quality improvement project. J Pain Symptom Manage. 2015;50:724-9.
- [Google Scholar]
- Spirituality and spiritual care perspectives among baccalaureate nursing students in Saudi Arabia: A cross-sectional study. Nurse Educ Today. 2017;49:156-62.
- [Google Scholar]
- Research priorities in spiritual care: An international survey of palliative care researchers and clinicians. J Pain Symptom Manage. 2014;48:518-31.
- [Google Scholar]
- The effect of spiritual care on spiritual health of patients with cardiac ischemia. Iran J Nurs Midwifery Res. 2012;17:195-9.
- [Google Scholar]
- Effect of a spiritual care program on levels of anxiety in patients with leukemia. Iran J Nurs Midwifery Res. 2014;19:88-93.
- [Google Scholar]
- Spiritual care in hospitalized patients. Iran J Nurs Midwifery Res. 2011;16:125-32.
- [Google Scholar]
- Integration of spirituality in medical education in Iran: A Qualitative exploration of requirements. Evid Based Complement Alternat Med 2015 2015:793085.
- [Google Scholar]
- Impact of religion and spirituality on older adulthood. J Religion Spiritual Aging. 2014;27:16-33.
- [Google Scholar]
- Integrating religion and spirituality into mental health care, psychiatry and psychotherapy. Religions. 2011;2:611-27.
- [Google Scholar]
- Spirituality and spiritual care in and around childbirth. Women Birth. 2015;28:173-8.
- [Google Scholar]
- The effects of education on spirituality through virtual social media on the spiritual well-being of the public health students of Isfahan University of medical sciences in 2015. Int J Community Based Nurs Midwifery. 2016;4:168-75.
- [Google Scholar]
- Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Intern Med. 2013;173:1109-17.
- [Google Scholar]
- Improving the quality of spiritual care as a dimension of palliative care: The report of the consensus conference. J Palliat Med. 2009;12:885-904.
- [Google Scholar]
- A pilot study of nurses' experience of giving spiritual care. Qual Rep. 2010;15:852-63.
- [Google Scholar]
- Spirituality and health in the curricula of medical schools in Brazil. BMC Med Educ. 2012;12:78.
- [Google Scholar]
- Programs of religious/spiritual support in hospitals – Five “Whies” and five “Hows”. Philos Ethics Humanit Med. 2016;11:5.
- [Google Scholar]






