Translate this page into:
Early Intervention for the Management of Chronic Pain in a Patient with Recurrent Schwannoma Foot
Address for correspondence: Dr. Tuhin Mistry, 3rd Floor, B209, Lajpat Nagar 1, New Delhi - 110 024, India. E-mail: dr.tuhin2014@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Schwannoma or neurilemoma is a rare soft tissue tumor originating from the Schwann cells of peripheral nerve sheath. It rarely affects the foot.[1] The recurrence rate is very low (1%), and malignant transformation is extremely rare.[2] We describe successful management of chronic pain in a case of recurrent schwannoma foot.
A 30-year-old woman attended our pain clinic with history of swelling and pain over the medial aspect of right foot [Figure 1a and b]. The swelling gradually increased in size over a period of 4 months. She had a similar type of swelling at the same site which was surgically removed 2 years back. On examination, a 9 cm × 5 cm loculated swelling was noted on the medial and plantar aspect of the right foot with a 3-cm scar. There was loss of flexion of great toe and claw deformity of the second toe. The pain was sharp, aching, nonradiating in nature which was getting exaggerated on movements. It was associated with tingling sensation and not radiating to any other area. She had reported her pain as 5/10 at the time of presentation (day time) and 10/10 during night rated on 11-point numerical rating scale (NRS) score. She received medical treatment including paracetamol, ibuprofen, and gabapentin but without much relief. The patient has no history of other medical comorbidities. Blood investigations were unremarkable. Magnetic resonance imaging showed a large (9.7 cm × 5.5 cm), well-defined elongated soft tissue mass with cystic changes and encasing flexor tendons of foot as wells as plantar aponeuroses. The lesion was surrounding the first, second, and third metatarsals along with large extraosseous component involving plantar interosseous muscles. Flexion deformity of the second digit was seen due to encasement of flexor digitorum longus tendon. Histopathological examination of the needle core biopsy specimen confirmed the diagnosis of recurrent schwannoma.
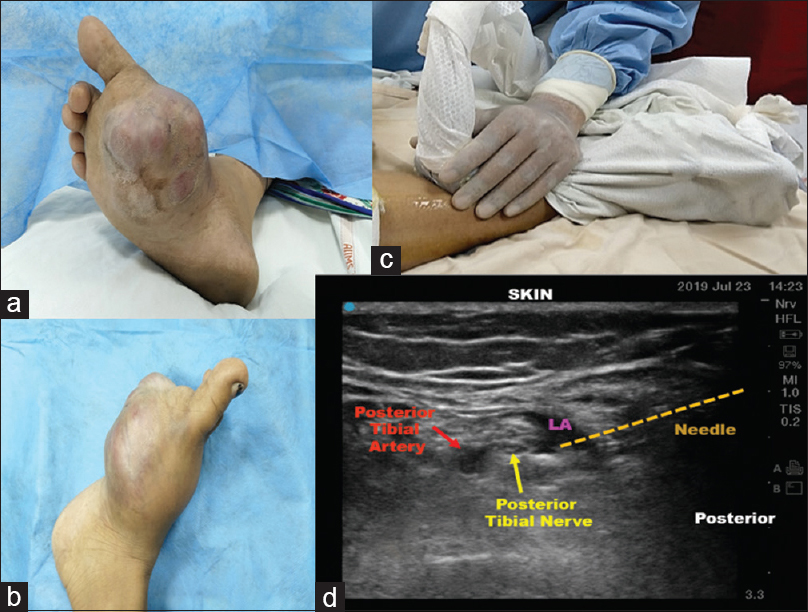
- (a and b) Schwannoma of right foot, (c) probe position, (d) posterior tibial nerve block. LA = Local anesthetic.
The tumor mass and pain were noted in the distribution of the dermatome supplied by medial plantar (L4, L5), lateral plantar (S1, S2), and saphenous (L3, L4) nerves. We decided to perform selective posterior tibial nerve (PTN) and saphenous nerve (SN) blocks to interrupt the pain cycle. Management plan was discussed with the patient, and informed and written consent was obtained. In the procedure room, intravenous cannula and basic American Society of Anesthesiologists monitors were attached. She was placed in supine position with the right leg flexed at knee, abducted, and externally rotated with a pillow under the leg to be blocked. Selective PTN and SN were blocked under all aseptic precautions. A high-frequency linear transducer (8–13 MHz) was placed transversely, slightly cephalad and posterior to the medial malleolus [Figure 1c]. The posterior tibial vessels were identified, and PTN was located posterolateral to artery. A 5-cm 21-G needle (Stimuplex® A, B. Braun Melsungen AG, Germany) was inserted in-plane until the tip penetrated the paraneural sheath. Five milliliters of local anesthetic (LA, 0.25% ropivacaine) and 4 mg of dexamethasone was injected [Figure 1d]. In addition, subcutaneous ring of LA (5 ml) infiltration was given at the level of medial malleolus with a 1.5-inch, 26-G hypodermic needle to block the SN. Within 5 min of nerve block, her pain score decreased to 0/10. Oral medicines were tapered on weekly follow-up, after which the patient was taken up for wide local excision of the tumor.
In schwannoma, pain in the involved area is mainly due to mass effect and direct involvement of the nerve and surrounding tissue.[3] Early intervention (peripheral nerve blocks) can be highly effective and ease the pain by offering immediate as well as longer-term relief. It can be used as the sole or even the principal treatment. PTN block has been used before for the management of painful calcaneal spur and neuropathic foot pain due to sarcoidosis.[45] With the help of basic anatomical knowledge and ultrasound-guided site-specific selective peripheral nerve blocks (PTN and SN), we could offer significant pain relief to our patient and improvement in her quality of life.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Imaging of peripheral nerve sheath tumors with pathologic correlation: Pictorial review. Eur J Radiol. 2004;52:229-39.
- [Google Scholar]
- Solitary benign peripheral-nerve tumours. Review of 32 years' experience. J Bone Joint Surg Br. 1995;77:497-500.
- [Google Scholar]
- Schwannoma of the foot: Report of four cases and literature review. Acta Biomed. 2019;90:214-20.
- [Google Scholar]
- Posterior tibial nerve block in the therapeutic management of painful calcaneal spur (plantar fasciitis): A preliminary experience. Can J Anaesth. 2003;50:862-3.
- [Google Scholar]
- Ultrasound guided posterior tibial nerve block for the management of chronic peripheral neuropathic foot pain secondary to sarcoidosis. J Pain. 2018;19:S79.
- [Google Scholar]





