Translate this page into:
Economics of Palliative and End-of-Life Care in India: A Concept Paper
Address for correspondence: Dr. Arunangshu Ghoshal, Department of Palliative Medicine, Tata Memorial Centre, Mumbai - 400 012, Maharashtra, India. E-mail: arun.bata@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Only a few studies have assessed the economic outcomes of palliative care in India. The major areas of interest include hospice care, the process and structure of care, symptom management, and palliative chemotherapy compared to best supportive care. At present, there is no definite health-care system followed in India. Medical bankruptcy is common. In situations where patients bear most of the costs, medical decision-making might have significant implications on economics of health care. Game theory might help in deciphering the underlying complexities of decision-making when considered as a two person nonzero sum game. Overall, interdisciplinary communication and cooperation between health economists and palliative care team seem necessary. This will lead to enhanced understanding of the challenges faced by each other and hopefully help develop ways to create meaningful, accurate, and reliable health economic data. These results can then be used as powerful advocacy tools to convince governments to allocate more funds for the cause of palliative care. Eventually, this will save overall costs and avoid unnecessary health-care spending.
Keywords
Decision-making
economics
India
logic traps
palliative medicine
INTRODUCTION
Palliative care services are expanding worldwide with the aim of improving the experience of patients with terminal illness at the end of life through better symptom control, coordination of care, and improved communication between professionals and the patient and family.[12] The application of economic evaluation to palliative care has been slow to develop and the evidence base remains small. There are challenges in applying the standard economic evaluation techniques to palliative care, such as difficulties in capturing all relevant data (e.g., informal care costs) and with conceptual issues of valuing benefits. There are also concerns of the full impact of the interventions not being captured. The appropriateness of applying standard economic evaluation techniques such as quality-adjusted life year (QALY) to measure outcomes in palliative care has been questioned.[3] The duration of effect is inevitably limited in many palliative interventions, but a short good experience may be given a high value and this is not captured in the standard approach of adding up QALYs.[4] Some studies show that care at the end of life can consume a large proportion of health-care resources, whereas, it has been shown to be cost-saving in others.[5] These are reasons why studies in this area do not undertake formal cost-effectiveness analyses, but rather assess implications of palliative care interventions on costs separately from outcomes. As a result, methodological approaches are varied and often rely on relatively small observational studies.[1] It is important to keep these challenges in mind when reviewing economic studies in this field. In countries with limited resources, service allocation needs to be cost-effective to suit health-care budget. The purpose of this paper is to bring about the various concepts of economic analysis for palliative care in Indian context.
HEALTH-CARE SYSTEM IN INDIA
At present, there is no uniform health-care system followed in India like in some developed countries; there is no nationalized prescription service as well. The universal health insurance system in government and private sector is still in its infancy and most of the population remains uninsured.[6] Only 3%–5% of Indians are covered under any form of health insurance – 4 million beneficiaries under the Central Government Health Scheme, 1.2 million under Railway Health Scheme, and 0.3 million under the Employees State Insurance Scheme. Private health insurance covers around 11.2 million individuals, but they tend to cater to the affluent classes, covering the healthiest and the wealthiest. It cannot fulfill India's objective of equity, efficiency, and quality in health because it results in limited social gain. In India, despite improvements in access to health care, inequalities are related to socioeconomic status, geography, and gender and are compounded by high out-of-pocket expenditures, with more than three-quarters of the increasing financial burden of health care being met by households. Health-care expenditures exacerbate poverty, and about 39 million additional people are falling into poverty every year because of such expenditures.[7] The magnitude of out of pocket expenditure is shown in Figure 1.[8]

- Out-of-pocket health expenditure (% of private expenditure on health) over the years in India (adapted from the World Health Organization Global Health Expenditure Database)
There is a wide difference in care costs in the country due to varied local clinical practices which leaves much of the population vulnerable. In 2003, the Indian government took an initiative to implement a universal health insurance scheme, but it failed reportedly because of its failure to cover the poor.[9] Then, in April 2008, the Union Ministry of Labor and Employment in India launched a Rashtriya Swasthya Bima Yojna (RSBY) smart card to combat the so-called “health-based poverty trap” in the country to provide health insurance coverage for people below poverty line. At present, there are 28.6 million RSBY card holders and their 115 million family members across India and have been found to be beneficial.[10] There are many challenges for the achievement of equity in service provision and equity in financing and financial risk protection in India. These challenges include an imbalance in resource allocation, inadequate physical access to high-quality health services and human resources for health, high out-of-pocket health expenditures, inflation in health spending, and behavioral factors that affect the demand for appropriate health care. Use of equity metrics in monitoring, assessment, and strategic planning; investment in development of a rigorous knowledge base of health-systems research; development of a refined equity-focused process of deliberative decision-making in health reform; and redefinition of the specific responsibilities and accountabilities of key actors are needed to try to achieve equity in health care in India.[7] The implementation of these principles with strengthened public health and primary-care services will help to ensure a more equitable health care for India's population. Health follows closely the developments in social and economic status of the general population and such holistic development is a major challenge for policymakers in India. Although linked with acute illness, catastrophic health-care spending is clearly prevalent in chronic conditions and more so in life-limiting illnesses. In fact, the palliative care physician might have to handle both an acute and a chronic illness, at a time in a dynamic manner. The high incidence of acute complications in the disease trajectory of chronic illnesses creates dual challenges.
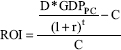
Proper utilization of the economics tools is paramount to bring efficiency in existing health-care systems to provide quality palliative care for all. In a market economy, where global competition is intense, pharmaceutical researchers, manufacturers, and marketers must explore the need for evaluating resources vis-à-vis outcomes for drugs used in palliative care. This could indeed be a valuable instrument in designing and implementing strategies in the current business world. The knowledge can then be utilized by government organizations for the reimbursement of pharmaceutical drugs and services to ensure the continuity of care. The Economist Intelligence Unit of Lien Foundation report in 2015 adds some valuable insight to this [Table 1].[11]
INTERSPECIALTY EXCHANGE
Palliative care skills are useful in a wide variety of medical and surgical specialties. As the scope of palliative care strengthens in India, the distinctions between different related medical subspecialties are getting blurred. Examples of clinical disciplines which intermingle with palliative medicine include nephrology, cardiology, geriatrics, pediatrics, neurology, and so on; all of them care for patients suffering from incurable illnesses at some stage.[1213] The paraclinical subjects also contribute to the growth of palliative medicine as a science: public health, pharmacology, occupational therapy, physical therapy, nursing, and psychology are but a few examples.[14] Yet other, classically nonmedical, ways of thinking, however, are enriching clinical science as well. These specialties bring with them the strength to expand its impact far beyond the walls of the outdoor patient clinic, the laboratory, the indoor ward, and the community home care. They allow to contribute toward influencing policy decisions and resource allocation, at national and regional levels. Thus, these sciences help to raise voice for the benefit of persons suffering from incurable illnesses. In this way, we as palliative care physicians live up to the promise made in the Hippocratic Oath: To work “for the benefit of the sick.”[15]
HEALTH ECONOMICS
One such specialty is health economics. Although not a component of traditional learning or teaching in medicine, health economics is gradually making inroads as an integral part of the pedagogy and praxis of palliative care. Faced with an ever-growing multitude of investigations for consultation and follow-up, multiple therapeutic drugs and devices, intensive counseling, and pledge for holistic care of the whole person; we need to know which one is the most cost-effective approach. This information is necessary at the individual, as well as community and national level. Respected as a source of updated knowledge by peers in the medical profession, our words (and actions) have an impact beyond practice. Thus, we need to be conversant with all laterally related fields of science. The specialty of health economics is a relatively young one. Its growth in developing countries, including India, is hindered by a lack of trained workforce, and by suboptimal collaboration between health care professionals and economists. The ever-increasing burden of noncommunicable diseases with many of them having a protracted course eventually straining on individual as well as national economy, however, are adequate stimulus to drive change.
OVERVIEW OF ECONOMICS OF PALLIATIVE MEDICINE
In a retrospective cohort study done on cancer patients in 7 developed nations, it was found that hospital expenditures near the end of life were higher in the United States, Norway, and Canada, intermediate in Germany and Belgium, and lower in the Netherlands and England.[16] However, as mentioned earlier, the results of cost analysis varies based on the methods used. For instance, study findings on cost data suggest that the costs of palliative care intervention can be significantly lower,[171819] can be indifferent[20212223] or even mistakenly higher.[24] In these studies, costs were computed for all health services used within 6 months following index hospitalization discharge (e.g., hospital outpatient, home health visits, hospital readmissions, and skilled nursing facility admissions). Cost savings were largely driven by a significant difference in hospital readmission costs. A systematic review focusing on the cost components and approaches for economic evaluation of palliative care, reported these aspects in greater details.[25] Briefly, it reports that the components of palliative care costs are incurred within four broad domains: hospital care, community or home-based care, hospice care and informal care. The costs incurred in providing palliative care can be considered from the economic perspective of three providers: state or government, insurers/third-party/not-for-profit organizations and patient and family and/or society. Finally, it concludes that a wide variety of costing approaches are used to derive costs and the majority are country specific.
TAKING DECISIONS IN PALLIATIVE CARE HAS ECONOMIC IMPLICATIONS – MEDICAL ETHICS, LOGIC TRAPS, GAME THEORY
A frequent theme in medical ethics of palliative care is that of making decisions and choices. Such decisions can drive the costs associated with care. A novel approach of exploring this relationship is with the application of game theory. Game theory is “the study of mathematical models of conflict and cooperation between intelligent rational decision-makers.”[26] Game theory is based on modeled decision-making. The goal of game theory is to describe frames of reference from which problems, issues, or dilemmas can be better understood or appreciated. As such, game theory may have relevance to medical ethics. As per game theory, the case of investment in palliative and end-of-life care can be considered as a two person nonzero sum game. Here, a gain for one participant does not necessarily reflect a loss for the other participant. In clinical practice, there are many two person games going on simultaneously; for example, patient–physician, physician–family, physician–hospital, and physician–insurance carrier. Few decisions are made with foreknowledge of the actual benefits and risks associated with those decisions. Typically, decisions are made with only estimates of the benefits and risks associated with those decisions. In game theory, the payoffs in decision-making are best thought of as ''utility functions.''[27] In practice, situations of dilemma are typically constructed or framed in a manner that encourages a limited perspective on the part of the participants. These concepts can be formally modeled. Figure 2 describes a generic game theory model depicting the situations when the physician must decide whether to recommend certain health-care intervention in the circumstance when obtaining further information is not feasible (e.g., to give a treatment when all diagnostic testing is exhausted). There is also a possibility that the patient/caregiver may demand treatment, which the doctor does not recommend. The two situations are then analyzed: (i) the patient does not get a treatment he wanted and (ii) the patient gets the therapy he demanded. The model is both simple to allow easier exposition of the conceptual model that we are proposing but also realistic enough to allow us to draw some conclusions important for health policy. It satisfies two key assumptions of game theory:[28] common knowledge and rationality. Common knowledge assumes both players can deduce what the other will do contingent on each player's move, that is, each player knows the consequences of each action, knows that both know it, knows that both know that both know it, etc. This assumption is particularly evident in trust version of game, which insists on its maximum transparency. Rationality assumes that the players are instrumentally rational in the sense that they will always choose strategies that maximize their own individual payoffs, relative to their knowledge, and beliefs about benefits and harms of each chosen strategy. There have been few concept papers where game theory concepts have been applied to palliative care.[29]
- Strengths, weaknesses, opportunities, and threats analysis (adapted from situational analysis in health-care industry)
PROPOSED MODELS FOR ECONOMIC ANALYSIS
Quantifying the value of any health-care intervention is difficult and complex and has significant data requirements. This is particularly true of interventions involving palliative care because benefits may be realized over the course of a time and well-beyond death rather than in the short term. The economics of palliative care can be analyzed in many ways. One of them is Return on Investment (ROI) analysis as the way future benefits would compare with initial “investments”[30] [Supplementary Material]. Although this model requires many assumptions and represents a great simplification of the dynamic costs and benefits of any health intervention over time, it is nevertheless a useful tool and starting point from which to begin comparing different programs and estimating the future benefits. In general terms, ROI depends on the costs and associated net benefits of an investment, with appropriate adjustments for the period within which costs are incurred and benefits realized. To compare benefits and costs of a health program, health benefits must be translated in monetary terms. The World Health Organization (WHO) Commission on Macroeconomics and Health proposes valuing one Disability-Adjusted Life Year (DALY) at 1–3 times the value of a given country's per capita Gross domestic product (GDP) (WHO, 2001).[31] Since these benefits will not be realized until far in the future, a discount rate needs to be applied to adjust them to their present value, accounting for the economic preference of a sum of money today over that same sum of money in the future. Data on current interventions are limited; for many, data are only available for costs and not for benefits. Therefore, the ROI equation must be modified to calculate the health benefit that a program must achieve to reap a favorable return on the initial investment.
-
Identify the intervention's economic costs:
-
Cost of materials
-
Cost of personnel
-
Value of time of patients participating in the intervention
-
Other overhead.
-
-
Identify the intervention's intended outcomes and benefits. Divide these into different categories that can be converted into a monetary benefit:
-
Health gains (e.g. cases of a disease, death rates, life expectancy, and DALYs averted)
-
Medical care savings (costs of diagnosis, treatment, and care)
-
Productivity savings (lost wages due to missed work).
-
-
Establish the period needed to achieve/see these outcomes.
-
Identify other indicators to measure along the way to the desired outcome (e.g. hypertension, prediabetes, and cervical lesions), and the activities needed to achieve them (e.g. screening, education, and distribution of testing strips). This will help in crafting program activities that will lead to the desired outcome
-
Identify a control group. If this is not possible, conduct a before-after study in the same group
-
Collect baseline data to measure outcomes and preintervention
-
Collect outcome data to measure those benefits attributable to the program
-
Exercise caution in generalizing results.
ROI equations are pretty much akin to doing Cost-benefit analysis (CBA), and the difficulty is always in expressing “health returns” in monetary terms.
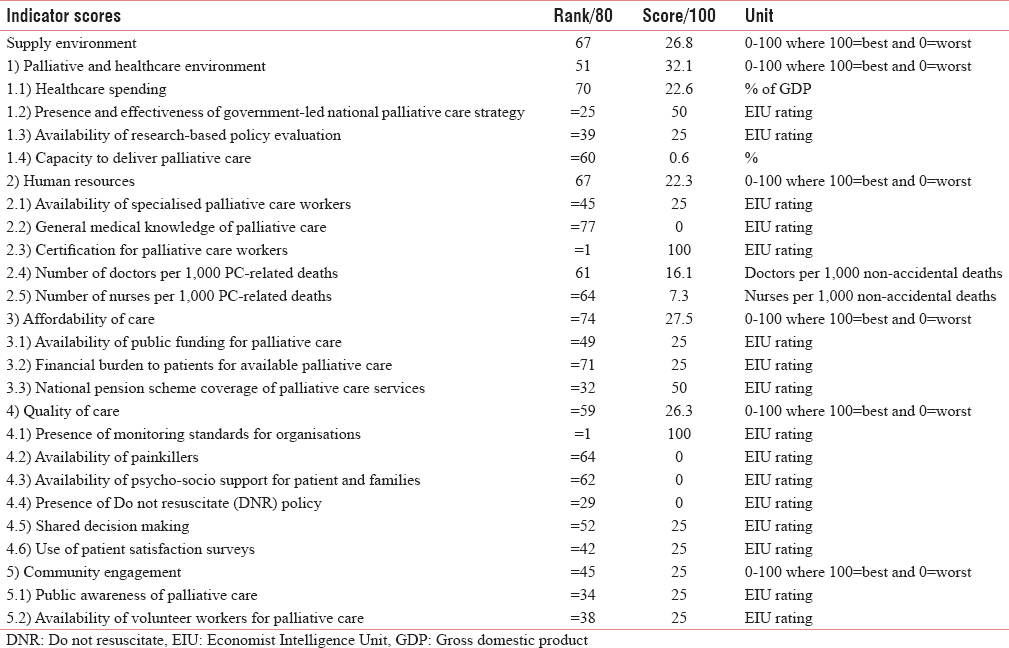
Another method is the SWOT analysis approach for understanding the strengths, weaknesses, opportunities, and threats in the fields of health economics. However, this approach has mostly been used in big data analysis of health-care companies and establishments.[32]
Some methods consider the costs and clinical outcomes together such as follows:
-
Cost minimization which assumes that alternative therapies have demonstrably equivalent clinical effectiveness and the lowest cost strategy is preferred[33]
-
Cost-effectiveness analysis (CEA), which helps to identify neglected opportunities by highlighting interventions that are relatively inexpensive, but with the potential to reduce the disease burden substantially. CEA helps identify ways to redirect resources to achieve more. It demonstrates not only the utility of allocating resources from ineffective to effective interventions but also the utility of allocating resources from less to more cost-effective interventions[34]
-
Cost-utility which assigns $ per additional life year saved by strategy then estimates the quality of that benefit in $/QALY[35]
-
CBA which compares two strategies but converts the clinical benefit to money, for example, a year of life is worth $100,000.[36]
Some are novel methods such as follows:
-
Cost avoidance which measures the costs saved by not doing procedures or by moving from an expensive place of care to a less expensive place[37]
-
Opportunity cost which analyze the cost of performing one action rather than another, such as the opportunity cost of a patient staying in the Intensive Care Unit (ICU) when appropriate for palliative care end of life is the high cost of that day plus the lost revenue of the ICU day plus the lost opportunity if a potential patient did not get appropriate trauma or ICU care[38]
-
Palliative care development currency to group patients' health-care needs into units that are clinically similar and have broadly similar resource needs and costs.[39]
THE WAY FORWARD
Health economics should focus on the case of palliative care in India. Interdisciplinary communication and cooperation between health economists and palliative care team are necessary. This will lead to enhanced understanding of the challenges faced by each other and hopefully help develop ways to create meaningful, accurate, and reliable health economic data. These results can then be used as powerful advocacy tools to convince governments to allocate more funds for the cause of palliative care. Eventually, this will save overall costs and avoid unnecessary health-care spending leading to medical bankruptcies. In this context, it is also important to discuss that some proponents of hospital-based palliative care have suggested that palliative care consultations reduce length of stay in ICUs or in the hospital in general. This adds to the operational/financial incentive for hospitals, a justification for them to invest in palliative care programs, and similar to the incentive of lower costs per day.[40]
Better data are needed to reduce the uncertainty about the true impact of palliative care, both economic and otherwise. Furthermore, more data are needed on the impact of palliative care programs on the whole health system, not on individual silos. The field would benefit from more research designs that assess inputs and outputs at a patient level or population level (rather than at an admission level), from prospective and longitudinal studies that can determine at which point and for which patients palliative care is presented as an option and actually implemented, from multicenter and comparative studies that can assess whether consultative services have the same kind and degree of clinical and financial impact (or for the same kinds of patients) as dedicated units; or whether other aspects of program design are important, such as the degree of clinical control that the palliative care team has after its initial consultation. These kinds of research designs are especially important as palliative care begins to address care from diagnosis forward and not just a few hours or days before death.
There is not any single method for the economic analysis of palliative care available at the moment and development work for appropriate methods is still underway.[41] Hence, despite their limitations, these methods coupled with some sensitivity analysis might be our way forward.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank patients and their relatives for their kind participation and also supporting staff of the Department of Palliative Medicine.
REFERENCES
- Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? J Pain Symptom Manage. 2003;25:150-68.
- [Google Scholar]
- Effectiveness of specialized palliative care: A systematic review. JAMA. 2008;299:1698-709.
- [Google Scholar]
- Optimal approaches to the health economics of palliative care: Report of an international think tank. J Pain Symptom Manage. 2009;38:4-10.
- [Google Scholar]
- Setting priorities in and for end-of-life care: Challenges in the application of economic evaluation. Health Econ Policy Law. 2012;7:431-9.
- [Google Scholar]
- Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliat Med. 2014;28:130-50.
- [Google Scholar]
- Universal health insurance in India: Ensuring equity, efficiency, and quality. Indian J Community Med. 2012;37:142-9.
- [Google Scholar]
- Out-of-Pocket Health Expenditure (% of Private Expenditure on Health) | Data. Available from: http://www.data.worldbank.org/indicator/SH.XPD.OOPC.ZS?contextual=default&end=2014&locations=IN&start=1995&view=chart
- Poor Risk Cover under Govt. Health Scheme – The Hindu. Available from: http://www.thehindu.com/data/poor-risk-cover-under-govt-health-scheme/article7793554.ece
- Pharmacoeconomics- Regulatory perspective and its relevance in Indian Context. Pharma Times. 2013;45:18-20.
- [Google Scholar]
- The Economist and Intelligence Unit. 2015. The 2015 Quality of Death– Ranking end-of-life care across the world. Available from: https://www.eiuperspectives.economist.com/sites/default/files/2015%20EIU%20Quality%20of%20Death%20Index%20Oct%2029%20FINAL.pdf
- [Google Scholar]
- Higginson, Jonathan Koffman, Public Health and Palliative Care, Clinics in Geriatric Medicine. 2005;21:45-55.
- Greek Medicine – The Hippocratic Oath. U.S. National Library of Medicine. Available from: https://www.nlm.nih.gov/hmd/greek/greek_oath.html
- Comparison of Site of Death, Health Care Utilization, and Hospital Expenditures for Patients Dying With Cancer in 7 Developed Countries. JAMA. 2016;315:272-83.
- [Google Scholar]
- Impact of an inpatient palliative care team: A randomized control trial. J Palliat Med. 2008;11:180-90.
- [Google Scholar]
- Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55:993-1000.
- [Google Scholar]
- Is short-term palliative care cost-effective in multiple sclerosis? A randomized phase II trial. J Pain Symptom Manage. 2009;38:816-26.
- [Google Scholar]
- Effects of a program for coordinated care of advanced illness on patients, surrogates, and healthcare costs: A randomized trial. Am J Manag Care. 2006;12:93-100.
- [Google Scholar]
- The comprehensive care team: A controlled trial of outpatient palliative medicine consultation. Arch Intern Med. 2004;164:83-91.
- [Google Scholar]
- Utilization and costs of the introduction of system-wide palliative care in Alberta, 1993-2000. Palliat Med. 2005;19:513-20.
- [Google Scholar]
- The Myth Regarding the High Cost of End-of-Life Care. Am J Public Health. 2015;105:2411-5.
- [Google Scholar]
- What cost components are relevant for economic evaluations of palliative care, and what approaches are used to measure these costs? A systematic review. Palliative Medicine. 2017;31:323-37.
- [Google Scholar]
- Game Theory: Analysis of Conflict. Harvard University Press; 1991.
- Game theory, a nontechnical introduction. Mineola: Dover Publications, Inc; 1970.
- Medical ethics, logic traps, and game theory: An illustrative tale of brain death. J Med Ethics. 2004;30:359-61.
- [Google Scholar]
- Economics of Non-Communicable Diseases in India: The Costs and Returns on Investment of Interventions 2014. Economics of Non-Communicable Diseases in India. Public Health 2014 November
- [Google Scholar]
- Commission on Macroeconomics and Health. Macroeconomics and Health: Investing in Health for Economic Development. 2001. Prepared for the World Health Organization. Available from: http://www.who.int/iris/handle/10665/42463
- [Google Scholar]
- Big data and health economics: Strengths, weaknesses, opportunities and threats. Pharmacoeconomics. 2016;34:101-6.
- [Google Scholar]
- A cost-minimization analysis comparing azithromycin-based and levofloxacin-based protocols for the treatment of patients hospitalized with community-acquired pneumonia: Results from the CAP-IN trial. Chest. 2005;128:3246-54.
- [Google Scholar]
- Measuring Preferences for Cost-Utility Analysis: How Choice of Method May Influence Decision-Making. Pharmacoeconomics. 2007;25:93-106.
- [Google Scholar]
- Cost-Benefit Analysis of a Medical Emergency Team in a Children's Hospital Christopher P. Bonafide, A. Russell Localio, Lihai Song, Kathryn E. Roberts, Vinay M. Nadkarni, Margaret Priestley, Christine W. Paine, Miriam Zander, Meaghan Lutts, Patrick W. Brady, Ron Keren Pediatrics Aug. 2014;134:235-41.
- Analysis of Cost Avoidance From Pharmacy Students' Clinical Interventions at a Psychiatric Hospital. Am J Pharm Educ. 2011;75:8.
- [Google Scholar]
- Opportunity costs and local health service spending decisions: A qualitative study from Wales. BMC Health Serv Res. 2016;16:103.
- [Google Scholar]
- NHS England. Developing a New Approach to Palliative Care Funding. Available from: https://www.england.nhs.uk/2015/03/palliative-care-funding/
- Cost and non-clinical outcomes of palliative care. J Pain Symptom Manage. 2009;38:32-44.
- [Google Scholar]
- An economic view on the current state of the economics of palliative and end-of-life care. Palliat Med. 2017;31:291-2.
- [Google Scholar]
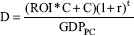
SUPPLEMENTARY MATERIAL: Return on investment: Equations
Return on investment (ROI) can be calculated as equal to the present value of benefits assumed to be realized in the future (BPV) minus initial costs (C), divided by initial costs. The benefits are assumed to result from the initial costs and we assume no other additional benefits:

To find the present value of benefits, the future value of the benefits is calculated first. This is done by multiplying the number of DALYs averted (D) by per-capita GDP (GDPPC). Then, a chosen discount rate (r) is applied by dividing this value by (1 + r) raised to t, where t equals the number of time periods over which these benefits will accrue (in this case, we take 20 years as an example). Cost is not discounted in this case because the assumption is that the money is spent today, all at once. This is a conservative estimate of the present value of the future benefits. It is assumed that all benefits will appear at the end of the 20th year after intervention, not during the 20-year period after intervention or beyond:
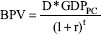
To find the number of DALYs that will achieve a specific ROI, solution for D: