Translate this page into:
Effect of Palliative Bronchoscopic Interventions on Symptom Burden in Patients with Central Airway Narrowing: A Retrospective Review
Address for correspondence: Dr. Nishkarsh Gupta, Department of Onco-Anaesthesia and Palliative Medicine, Dr. B.R.A. Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, India. E-mail: drnishkarsh@rediffmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Early integration of palliative interventions in patients with central airway obstruction (CAO) has shown to reduce patients' distress due to breathlessness and achieve better outcomes at lower cost. This retrospective review was performed to determine whether rigid bronchoscopic interventions alleviated the symptom burden and the requirement for continued mechanical ventilation in patients with CAO in a tertiary care hospital.
Materials and Methods:
Detailed records of 105 patients with CAO were retrospectively studied. The Numerical Rating Scale (NRS) score for cough and dyspnea before and after the intervention was noted. A need for an escalation or reduction in level of care was also noted.
Results:
The mean NRS score for dyspnea (n = 84) reduced from 7.5 (4–9) (before procedure) to 2.5 (2–6) after intervention (P < 0.01). The mean NRS score for cough (n = 68) also reduced from 6.5 (4–8) (before procedure) to 4 (3–7) after intervention (P < 0.01). Of these patients, bronchoscopic intervention allowed transfer out of the ICU in 14 patients (42%) and immediate withdrawal of mechanical ventilation in 8 patients (42%).
Conclusion:
There is an instantaneous valuable palliation of symptoms and improved health-care utilization with airway tumor debulking and stenting. Multidisciplinary interventions with emphasis delivery of palliative care provide better care of patients with CAO.
Keywords
Airway
bronchoscopic intervention
palliative
stent
INTRODUCTION
Breathlessness is an overbearing symptom, distressing patients with various malignant and nonmalignant diseases. It leads to substantial misery to patients and their families and is a significant cost to health-care systems. Prompt management of this symptom should, thus, be vital for all clinicians. Managing breathlessness consists of both nonpharmacological and pharmacological interventions as demonstrated by recent randomized controlled trials of multidisciplinary breathlessness support services.[12] Central airway obstruction (CAO) is a potentially life-threatening presentation of mediastinal or lung tumors and may necessitate emergency diagnostic and therapeutic rigid bronchoscopic interventions. Early integration of palliative interventions in patients with CAO has shown to reduce patients' distress due to breathlessness and achieve better outcomes at lower cost. The present study was performed to determine whether rigid bronchoscopic interventions alleviated the symptom burden and the requirement for continued mechanical ventilation in patients with CAO in a tertiary care hospital.
MATERIALS AND METHODS
Details of 227 patients undergoing interventional bronchoscopy procedures (diagnostic, therapeutic, or palliative), between August 2015 and July 2017 were retrospectively reviewed. Records of 105 patients with CAO (malignant conditions or benign inflammatory narrowing) dictating hospitalization before referral for therapeutic bronchoscopic intervention were then extracted for further analysis. The indications and procedures done were noted. The Numerical Rating Scale (NRS) score for cough and dyspnea before and after the intervention was noted. A need for an escalation or reduction in level of care was also noted. Reduction in level of care (defined as transfer from ICU to ward) and escalation in level of care (defined as transfer to the ICU or death) and complication or adverse events if any were noted.
RESULTS
Bronchoscopic interventions (diagnostic, therapeutic, or palliative) were performed in 227 patients. Of these, 105 patients suffered from CAO (malignant conditions or benign inflammatory narrowing) [Table 1].
| Conditions | Number of cases |
|---|---|
| Elective cases | |
| Tracheobronchial stenosis | 21 |
| Carcinoma lung | 14 |
| Fistula | 13 |
| Stent in situ, with stridor | 12 |
| Mediastinal mass | 11 |
| Intratracheal mass | 10 |
| Endobronchial carcinoid | 4 |
| Ca thyroid with tracheal compression | 2 |
| Emergency cases | |
| Bronchial mass with mediastinal shift | 6 |
| Postintubation tracheal stenosis in stridor | 5 |
| Mediastinal mass with tracheal compression | 5 |
| Retrosternal thyroid mass in stridor | 2 |
Eighteen patients required emergency intervention and 87 patients required elective bronchoscopic interventions [Table 2]. Interventions for CAO included laser or cryo debulking and recanalization, mechanical debulking, dilatation, electrocauterization of tracheal webs, and balloon dilatation and stent placement (for tracheoesophageal fistula, tracheobronchial mass, mediastinal mass, and stricture). Mean NRS scores for dyspnea and cough could be recorded for nonventilated patients only. The median NRS score for dyspnea (n = 84) reduced from 7.5 (4–9) (before procedure) to 2.5 (2–6) after intervention (P < 0.01). Similarly, the median NRS score for cough (n = 68) also reduced from 6.5 (4–8) (before procedure) to 4 (3–7) after intervention (P < 0.01) [Figure 1].
| Procedure | Number of cases |
|---|---|
| Tracheal/bronchial stenting | 47 |
| Debulking and tracheal stenting | 11 |
| Balloon dilatation | 10 |
| balloon dilatation and tracheal/bronchial stenting | 8 |
| Recanalization of airway by mechanical/laser/cryo/ | 6 |
| electrosurgical debulking | |
| Granulation tissue removal | 6 |
| Electrosurgical debulking of granulation tissue and | 5 |
| balloon dilatation | |
| Stent removal | 4 |
| Tracheal dilatation and cauterization of web and stenting | 3 |
| Stent repositioning | 2 |
| Bronchoscopic snaring of tumor mass | 2 |
| Coring but procedure abandoned due to bleeding | 1 |

- Effect of intervention on symptom burden
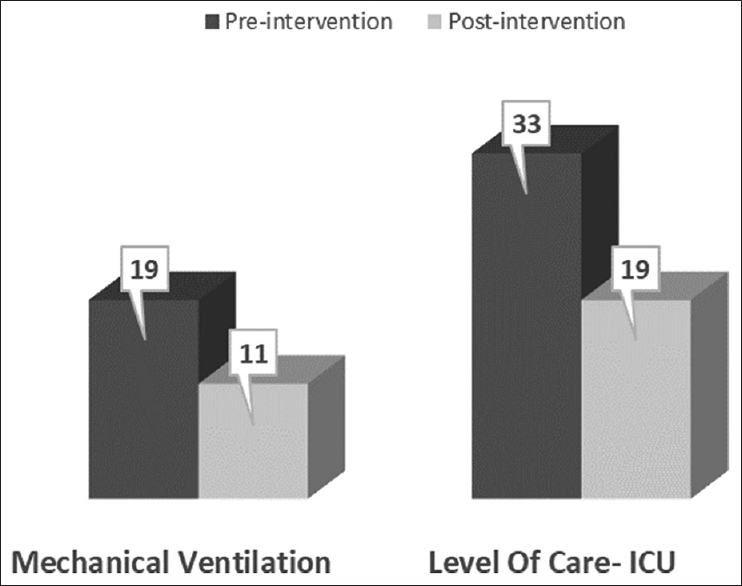
Thirty-three patients were admitted in the ICU and 19 patients required mechanical ventilation before the procedure. Of these patients, bronchoscopic intervention allowed for shifting of the patients from the ICU to general ward in 14 patients (42%) and immediate discontinuation of mechanical ventilation in 8 patients (42%) [Figure 2]. However, two previously nonventilated patients required postoperative ventilation due to intraoperative complications, i.e., posterior tracheal wall tear during stent placement and bleeding during snaring of tumor.
- Effect of intervention on health-care utilization
Other significant complications, (but not requiring escalation in the level of care) included temporary oxygen desaturation, exaggerated hemodynamic fluctuations, stent malpositioning, gross airway edema, and delayed recovery from anesthesia.
DISCUSSION
This retrospective study represents a single-institution experience with the bronchoscopic management of CAO with the interdisciplinary coordination of intervention pulmonologist and anesthesiologists. This series of 105 patients with CAO undergoing therapeutic bronchoscopic interventions between August 2015 and July 2017 evaluates the varied etiology of CAO and validates the findings described in similar series of cases undergoing complex bronchoscopic procedures.[345678] These reports highlighted the diverse approaches to these lesions, leading to substantial palliation of distressing symptoms with a low complication rate.[9] In our study, patients had significant immediate improvement in their respiratory symptoms, i.e., cough and dyspnea. The considerable reduction in symptoms of our patients shows promise. However, further studies are required to ascertain the long-term impact on symptoms and quality of life or death.
Bronchoscopic intervention permitted withdrawal of mechanical ventilation and decreased requirement of intensive care admission in 42% of patients. However, due to complications, two previously nonventilated patients required mechanical ventilation for a brief period after the procedure. These corroborate the findings of other reports, confirming de-escalation in the level of care.[1011]
Studies have shown that health-care expenditures are high at the end of life, more so in the event of a terminal ICU admission, despite the use of hospice- and home-based palliative care services.[1213]
A suitable apportionment of intensive-care beds, especially in a resource-limited setting, forms an indispensable element of managing health-care costs.[14] The results from our study imitate evidence from the previous studies,[10151617] advocating for effective bronchoscopic restoration of airway patency in patients with CAO, forestalling continual mechanical ventilation. Not only do such interventions reduce hospital costs, but also boost communication between patient and physician, providing time to initiate additional therapies,[18] or discussions toward advanced care directives.
CAO causes breathlessness and other distressing symptoms, which increase as the disease progresses. It is associated with shortened life expectancy, anxiety among patient and caregivers, and results in frequent hospital visits and admission. The refractory nature of these symptoms, especially in advanced malignancy, denotes a major unmet palliative care challenge.
Although airway resection and reconstruction are the preferred treatment for both benign and malignant lesions,[19] definitive surgical correction is not possible for several patients either due to the extent of the disease such as a long stenosis, metastatic or unresectable malignancy, or due to patient refusal or high expected morbidity. Hence, palliation of symptoms is of utmost importance in such cases. On the other hand, opioids are frequently used to relieve dyspnea in the practice of palliative medicine.[20] Opioids can perform like an ambiguous weapon against dyspnea, owing to their side effects such as constipation[21] and nausea[22] which may worsen the quality of life. Palliative interventional bronchoscopic procedures in CAO should not be suspended merely based on patients' prognostic status, as they can prove to be an effective substitute to conservative comfort measures, to alleviate suffering in select tertiary care centers. This holds true, especially for patients with longer survival such as benign lesions and regionally advanced cancers.
Various studies focus on the ICU or hospital length of stay, but this quantitative tool, although easier to measure, is constrained as it disregards the quality of patients' and caregivers' lives. Although such interventions cause immediate relief in dyspnea and other symptoms as demonstrated in this study, it would have been valuable to evaluate the long-term impact of interventions on survival and quality of life.[23] Another important limitation of our study was that it embraced an immediate benefit but did not follow-up the patients after discharge from hospital to evaluate the quality of life or death. Therefore, the quality of dying is a valuable tool that needs to be validated in further research.[24]
CONCLUSION
Bronchoscopic interventions for CAO provide immediate palliation of distressing, may offer additional time for systemic therapies to take effect and allow opportunities for end-of-life discussions. It may also help in reducing costs of health-care utilization by reducing the need of higher level of care; the benefits of which should not be disregarded. Further studies are needed to objectively quantify the benefits of these interventions on the quality of life and death.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: A randomised controlled trial. Lancet Respir Med. 2014;2:979-87.
- [Google Scholar]
- The clinical and cost effectiveness of a breathlessness intervention service for patients with advanced non-malignant disease and their informal carers: Mixed findings of a mixed method randomised controlled trial. Trials. 2016;17:185.
- [Google Scholar]
- Endoscopic relief of malignant airway obstruction. Ann Thorac Surg. 1989;48:469-73.
- [Google Scholar]
- Endobronchial management of benign, malignant, and lung transplantation airway stenoses. Ann Thorac Surg. 1995;59:1417-22.
- [Google Scholar]
- Silicone stents in the management of inoperable tracheobronchial stenoses. Indications and limitations. Chest. 1993;104:1653-9.
- [Google Scholar]
- A bifurcated silicone rubber stent for relief of tracheobronchial obstruction. J Thorac Cardiovasc Surg. 1982;83:414-7.
- [Google Scholar]
- Airway stenting for malignant and benign tracheobronchial stenosis. Ann Thorac Surg. 2003;76:167-72.
- [Google Scholar]
- Tracheobronchial stents in palliative care: A case series and literature review. BMJ Support Palliat Care. 2018;8:335-9.
- [Google Scholar]
- Therapeutic rigid bronchoscopy allows level of care changes in patients with acute respiratory failure from central airways obstruction. Chest. 1997;112:202-6.
- [Google Scholar]
- Complications following therapeutic bronchoscopy for malignant central airway obstruction: Results of the AQuIRE registry. Chest. 2015;148:450-71.
- [Google Scholar]
- Use of intensive care at the end of life in the United States: An epidemiologic study. Crit Care Med. 2004;32:638-43.
- [Google Scholar]
- Time to death and health expenditure: An improved model for the impact of demographic change on health care costs. Age Ageing. 2004;33:556-61.
- [Google Scholar]
- Guidelines for intensive care unit admission, discharge, and triage. Task force of the American College of Critical Care Medicine, society of critical care medicine. Crit Care Med. 1999;27:633-8.
- [Google Scholar]
- The use of expandable metal stents to facilitate extubation in patients with large airway obstruction. Chest. 1998;114:1378-82.
- [Google Scholar]
- Bronchoscopic intervention obviates the need for continued mechanical ventilation in patients with airway obstruction and respiratory failure from inoperable non-small-cell lung cancer. Respiration. 2012;84:55-61.
- [Google Scholar]
- Endobronchial stenting in patients requiring mechanical ventilation for major airway obstruction. Ann Acad Med Singapore. 2000;29:66-70.
- [Google Scholar]
- Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol. 2006;1:319-23.
- [Google Scholar]
- Postintubation tracheal stenosis. Treatment and results. J Thorac Cardiovasc Surg. 1995;109:486-92.
- [Google Scholar]
- Opioids for the palliation of refractory breathlessness in adults with advanced disease and terminal illness. Cochrane Database Syst Rev. 2016;3:CD011008.
- [Google Scholar]
- Incidence and health related quality of life of opioid-induced constipation in chronic noncancer pain patients: A prospective multicentre cohort study. Pain Res Treat 2018 2018:5704627.
- [Google Scholar]
- Opioid use and potency are associated with clinical features, quality of life, and use of resources in patients with gastroparesis. Clin Gastroenterol Hepatol 2018:pii: S1542-3565(18)31134-0.
- [Google Scholar]
- Tracheobronchial stenting in the terminal care of cancer patients with central airways obstruction. Chest. 2001;120:1811-4.
- [Google Scholar]
- The quality of dying and death: Is it ready for use as an outcome measure? Chest. 2013;143:289-91.
- [Google Scholar]






