Translate this page into:
Effect of Supportive Psychotherapy on Mental Health Status and Quality of Life of Female Cancer Patients Receiving Chemotherapy for Recurrent Disease
Address for correspondence: Dr. Koustav Mazumder, Department of Radiotherapy and Oncology, Post Graduate Institute of Medical Education and Research, Nehru Hospital, B Block, Chandigarh - 160 012, India. E-mail: koustavmajumder1986@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Cancer patients receiving chemotherapy for their recurrent disease often report the presence of anxiety and depression.
Aims:
In the study, we intended to find out the mental health status and overall quality of life (QOL) of such patients and to identify the effect of supportive psychotherapy.
Subjects and Methods:
Forty cancer patients undergoing second or subsequent line chemotherapy(CCT) were selected for psychotherapy session. Pre- and post-psychotherapy evaluation of anxiety and depression was determined by hospital anxiety depression scale. The QOL was measured before and after psychotherapy sessions by using WHO QOL-BREF scale.
Statistical Analysis Used:
Statistical analysis was done by paired t-test, using SPSS V.20.
Results:
Among 40 patients, 17 patients had breast cancer, and the remaining had ovarian cancer. All breast cancer and 19 ovarian cancer patients were receiving 2nd line CCT. Four ovarian cancer patients were undergoing 3rd line CCT. Results indicated that mean scores (± standard deviation) of anxiety 13.95 (±4) and depression 15.5 (±4.4) both exceeded the cut-off score of 11 and mean score of QOL physical health 29.77 (±10.1), psychological health 31.3 (±10.1), social relationship 35.1 (±9.6), and environmental condition 25.9 (±9.9) was below cut-off score of 60. After psychotherapy, there was significant reduction in anxiety (P < 0.01), depression (P < 0.01) and improvement on QOL physical heath (P = 0.02), psychological health (P < 0.01), environmental condition (P < 0.01), and social relationship (P < 0.01).
Conclusions:
Supportive psychotherapy helps to reduce the level of anxiety, depression, and increase the QOL. Therefore, psychotherapeutic intervention should be encouraged along with chemotherapy to promote positive mental health and to obtain full benefit of their physical treatment.
Keywords
Chemotherapy
mental health
quality of life
recurrent disease
supportive psychotherapy
INTRODUCTION
Being diagnosed with a long-term terminal illness like cancer has an important impact on mental health status of a patient causing low mood, excessive anxiety, and impairment in quality of life (QOL). With better screening and advanced management, there has been a decline in the mortality rate from cancer,[1] especially in ovarian, breast, and lung cancer. However, these solid tumors are known for their recurrence which might lead to offering the patients to undergo second or subsequent lines of chemotherapy. Psychosocial impacts of patients with cancer who fail to respond or have relapse after first-line chemotherapy are even worse. Facing a recurrence of cancer can be extremely challenging, potentially having significant impact on QOL and might result in psychological distress such as symptoms of anxiety and depression. Despite decades of clinical cancer research, the actual impact of second and subsequent lines of chemotherapy on the mental health status of cancer patients is still unknown. To design early therapeutic interventions that can improve QOL in this population, a better understanding is needed about various factors that are associated with QOL, for example, psychological, physiological, social, and environmental factors.[2] Psychotherapy offers the cancer patient a place to express their worries and help them to regain hope to live as some patients start to separate themselves from society after the diagnosis. One of the most commonly used therapies while working with chronically ill patients is the supportive psychotherapy which involves the integration of behavioral therapy, cognitive behavior therapy, family therapy, group therapy, and psychodynamic therapy.[3] In short-term supportive psychotherapy, clinicians must accurately diagnose persons suffering from depression and use structured psychotherapeutic and psychopharmacologic interventions for the depressed cancer patient.[4] Supportive psychotherapy reduces psychological distress by providing emotional support to the patients and/or caregivers and also helps them to accept the present situation rationally.[567] Supportive group psychotherapy helps cancer patients to face and accept their physical concerns, manage uncontrolled emotions, and enhance social support and family relationship.[8]
This study was planned to determine the mental health status and overall QOL of patients with breast and ovarian cancer receiving chemotherapy for recurrence of disease and to identify if there is any effect of supportive psychotherapy on the change in the level of anxiety, depression, and QOL among them.
SUBJECTS AND METHODS
In the present study, the technique of purposive sampling has been used. Forty female cancer patients, belonging to low and medium socioeconomic status, aging between 40 and 60 years undergoing second or subsequent lines of chemotherapy were studied between April and October 2016. Patients who were already on psychiatric medication were excluded from the study.
At first, consent was taken from the patients. Psychological distress was assessed by the Hindi version of hospital anxiety and depression scale (HADS).[9] According to the scoring system, scores ≥11 on the anxiety HADS and depression HADS scales were taken as “abnormal (case).”[10] QOL of the patients was assessed by WHO QOL-BREF scale.[11] This has four different domains: Physical health, psychological, social relationship, and environment. According to the literature, the cutoff score in all domains is 60.[12] Thus, any score below 60 was regarded as poor QOL.
On the basis of need of persons, management plan was prepared and supportive psychotherapy was given to each individual for four sessions (30–45 min/session) at 1 week interval. Therapeutic structure per session includes Session 1: Establishment of rapport and psychoeducation about acceptance of physical health status, psychological distress, effectiveness of supportive psychotherapy, and mindfulness were introduced. Session 2: Active listening for emotional catharsis with empathetic approach and unconditional positive regards. Activity scheduling was prepared with pleasure and mastery. Interaction with caregiver was done to provide emotional support for psychological burnout. Session 3: Deep breathing relaxation with visual imagery was demonstrated and active involvement with spirituality was encouraged. Session 4: Terminations of therapy and relapse prevention techniques were explained.
Postpsychotherapy evaluation was done after completion of the 4th session of the therapy. Pre- and post-psychotherapeutic assessments and supportive psychotherapy were conducted by registered clinical psychologist under individual administration condition. Standard scoring procedures were followed. To determine the central tendency and the variability of the scores, the mean and standard deviation (SD) were calculated for all participants. To test the significance of difference between pre- and post-psychotherapeutic session, parametric statistic paired sample t-test has been done. Statistical analysis was done using SPSS V20 software (IBM, Armonk, NY). P < 0.05 was considered as statistically significant.
RESULTS
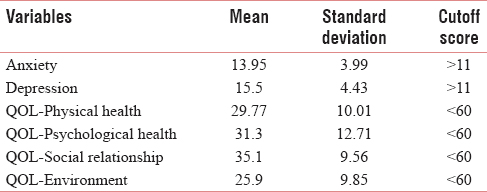
Among 40 patients, 17 patients were suffering from breast cancer and the remaining had ovarian cancer. All breast cancer and 19 ovarian cancer patients were receiving 2nd line chemotherapy(CCT). Four ovarian cancer patients underwent 3rd line CCT. On prepsychotherapy evaluation, it was seen that mean scores (± SD) of anxiety 13.95 (±3.99) and depression 15.5 (±4.43) both exceed the cutoff point (11) [Table 1], which indicates depressive or anxiety symptoms are present among this group of patients. It was also seen that mean score (± SD) of the 4 domains of QOL, namely, physical heath 29.77 (±10.01), psychological health 31.3 (±12.71), social relationship 35.1 (±9.56), and environmental condition 25.9 (±9.85) were below cutoff score (60) [Table 1]. This is certainly indicative of poor QOL of these patients on all domains.
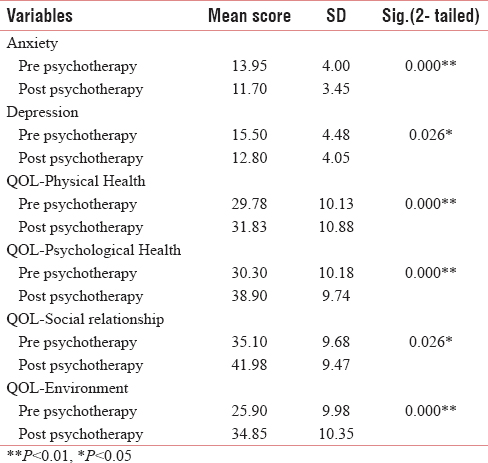
After psychotherapy, it was seen that the mean scores (± SD) of anxiety 11.7 (±3.45) and depression 12.80 (±4.05) have been decreased. On analysis by paired t-test, it was seen that after psychotherapy, there was a significant improvement in both anxiety (P < 0.001) and depression (P = 0.026). Postpsychotherapy, the mean score (± SD) of QOL physical health, psychological health, social relationship, and environment was 31.83 (±10.88), 38.9 (±9.74), 41.98 (±9.47), and 34.85 (±10.35), respectively. On analysis, it was seen that in the all domains, there was significant effect of supportive psychotherapy [Table 2].
DISCUSSION
We can no longer overlook the psychological, psychosocial, and behavioral consequences of cancer. The patient's psychological distress (depression and anxiety) is the source of more suffering, pain, or trauma than the disease itself could give rise to.[13] Treatments of cancer are aggressive in their impact on the physical, social, and emotional life of patients.[14] Surgery is at times very mutilating; radiotherapy has significant secondary effects such as skin problems, hair loss, anxiety, and depression; chemotherapy, often induces significant toxicity such as nausea, vomiting, digestive problems, hair loss, and anxiety.[15] For most people with cancer, finding out that cancer came back causes the hopelessness and depression.[16] Fear of the treatment and associated problems might increase apprehension or anxiety and is definitely a major cause of depression.
For many women, the diagnosis of breast cancer or ovarian cancer represents not only a major physical battle but also the ultimate emotional challenge – one that affects every relationship in persons' life. In Indian context, woman plays a vital role to keep the integrity of the family. Hence, when they are suffering from such disease, not only the mental status of that person gets deranged but also social position, physical and mental health, and QOL of the whole family get affected.[17] Family members of patients also face a time of readjustment after diagnosis and treatment of cancer. Any well-adjusted family relation is based on communication, trust, empathy, and emotional support. Side effects of cancer treatment sometimes wipe out patients' ability to communicate, especially about emotional issues. Unexpressed emotions can affect them even more which might eventually decrease QOL. It is found from the result of the present study that QOL is poor in the concerned group. There may be many contributing factors such as the needs and demands of children and dependent members of the family, problems of finance and housing; the lack of a near relation or of adequate support at difficult times; a sociocultural system that inhibits the expression of feelings; family or marital conflicts, and resulting disputes which were not resolved.
In the present study, it can be seen from Table 1 that persons suffering from cancer and undergoing second or subsequent lines of chemotherapy experience high level of anxiety, depression, and their QOL is poor. One of the great difficulties in diagnosing a state of anxiety and depression in a cancer patient is that of distinguishing it from the secondary manifestations of the disease or its treatments. Depression is commonly associated with approximately 15%–25% of cancer patients.[18]
Excessive anxiety, depression, fear of side effects, and behavioral change in patients before administration of the second or subsequent lines of chemotherapy often leads to refusal of further treatment which eventually reduces QOL. There is evidence that diagnosis and treatment of breast and ovarian cancer can place strains on a relationship, potentially leading to marital discord,[1920] and the perception of lack of support can adversely influence the woman's emotional well-being. From Table 2, it can be seen that supportive psychotherapy reduces anxiety and depression and increases levels of QOL (physical health, psychological health, social relationship, and environmental domains). The major objectives of supportive psychotherapy are care and support for patients and their caregiver. Supportive psychotherapy can be as effective as medications in the initial treatment of moderate to severe depression.[21] Results of many studies indicate supportive psychotherapy helps to enhance positive mental health by reducing anxiety and depression level and improves QOL of cancer patients.[52223242526] The goal of supportive psychotherapy is to help the person manage and cope with limitations which come along with cancer as well as help them to view their life in a more meaningful way.[27] People with chronic illness undergoing supportive psychotherapy have a better chance to be able to release the built-up tension and anxiety. According to Hochberg et al., 1979, psychotherapeutic relationship provides the patient a state of comfort, respect, and value which enhance their perspective about life.[28] It involves psychological, educational, and psychosocial intervention which provides empathy, mental support and promotes the persons' positive healthy lifestyle, resulting in reduction of the level of anxiety, depression, and enhancement of positive QOL after psychotherapy session.
The result of this study should be considered carefully as studies of this kind demand longitudinal method across months, but the present study did not fulfill this demand. It is also important to state that this is an exploratory study with a small sample. Again, during this study, various other sociodemographic factors, for example, income level, family type, socioeconomic status, marital status, and occupation were not considered. For future research, it would be better to replicate the present design with a larger sample and to include all other confounding variables. However, findings of the study highlighted a very important aspect that is psychosocial factor associated with female cancer patients as their preexisting mental health condition influences subsequent health-seeking behavior. Moreover, considering the large number of possibly depressed, anxious persons with poor QOL within this special sample, it would be useful to keep in mind the psychiatric issues as well so that care may be taken from this aspect also to obtain full benefit of their physical treatment.
CONCLUSION
From this study, it is evident that patients with breast cancer and ovarian cancer who are receiving chemotherapy for recurrent disease suffer from high level of depression, anxiety, their QOL is poor, and there is a significant effect of psychotherapeutic intervention on reduction of anxiety, depression, and enhancement of QOL of the patients. Hence, psychotherapeutic evaluation and intervention should be encouraged and promoted by the government in oncology departments to increase the awareness and to promote positive mental health.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank all the patients who participated in the study suffering from recurrent breast and ovarian cancer.
REFERENCES
- Population-based cancer survival trends in England and wales up to 2007: An assessment of the NHS cancer plan for England. Lancet Oncol. 2009;10:351-69.
- [Google Scholar]
- American Cancer Society. Cancer Facts and Statistics. Available from: http://www.cancer.org/research/cancerfactsstatistics/index
- [Google Scholar]
- The effects of psychoeducational care provided to adults with cancer: Meta-analysis of 116 studies. Oncol Nurs Forum. 1995;22:1369-81.
- [Google Scholar]
- Systematic review of psychological therapies for cancer patients: Overview and recommendations for future research. J Natl Cancer Inst. 2002;94:558-84.
- [Google Scholar]
- Mind and cancer: Does psychosocial intervention improve survival and psychological well-being? Eur J Cancer. 2002;38:1447-57.
- [Google Scholar]
- Supportive-expressive group therapy and distress in patients with metastatic breast cancer: A randomized clinical intervention trial. Arch Gen Psychiatry. 2001;58:494-501.
- [Google Scholar]
- QOL and psychiatric co-morbidity in Indian migraine patients: A headache clinic sample. Neurol India. 2013;61:355-9.
- [Google Scholar]
- Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551-8.
- [Google Scholar]
- Cut-off point for WHOQOL-bref as a measure of QOL of older adults. Rev Saude Publica. 2014;48:390-7.
- [Google Scholar]
- Psychosocial correlates of breast cancer and its treatments. Psychol Bull. 1980;87:108-31.
- [Google Scholar]
- Emotional distress in cancer patients at the beginning of chemotherapy and its relation to quality of life. J BUON. 2008;13:217-22.
- [Google Scholar]
- Evaluation of quality of life in patients receiving treatment for advanced breast cancer. Lancet. 1976;1:899-900.
- [Google Scholar]
- Depression, anxiety, and quality of life in patients with epithelial ovarian cancer. Gynecol Oncol. 2000;78:302-8.
- [Google Scholar]
- Psychological predictors of marital adjustment in breast cancer patients. Psychol Health Med. 2002;7:37-51.
- [Google Scholar]
- Depression assessment and classification in palliative cancer patients: A systematic literature review. Palliat Med. 2009;23:739-53.
- [Google Scholar]
- Cognitive therapy vs. medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62:409-16.
- [Google Scholar]
- Relaxation and imagery for anxiety and depression control in community patients with advanced cancer. Cancer Nurs. 2002;25:432-5.
- [Google Scholar]
- Psychotherapy improving depression and anxiety of patients treated with chemotherapy combined with radiotherapy. Chin J Clin Rehabil. 2003;7:2462-3.
- [Google Scholar]
- Effect of therapeutic touch on the well-being of persons with terminal cancer. J Holist Nurs. 1998;16:383-98.
- [Google Scholar]
- Evaluation by multidimensional instruments of health-related quality of life of elderly cancer patients undergoing three different “psychosocial” treatment approaches. A randomized clinical trial. Support Care Cancer. 1996;4:129-40.
- [Google Scholar]
- Psychotherapy for depression among incurable cancer patients. Cochrane Database Syst Rev. 2008;2:CD005537.
- [Google Scholar]
- Quality and duration of survival in glioblastoma multiforme. Combined surgical, radiation, and lomustine therapy. JAMA. 1979;241:1016-8.
- [Google Scholar]






