Translate this page into:
Effects of Yoga in Managing Fatigue in Breast Cancer Patients: A Randomized Controlled Trial
Address for correspondence: Dr. Raghavendra Mohan Rao, Healthcare Global Enterprises Ltd., No. 8, HCG Towers, P Kalinga Rao Road, Sampangiramnagar, Bengaluru - 560 027, Karnataka, India. E-mail: raghav.hcgrf@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Cancer-related fatigue is widely prevalent in cancer patients and affects quality of life in advanced cancer patients. Fatigue is caused due to both psychologic distress and physiological sequel following cancer progression and its treatment. In this study, we evaluate the effects of yogic intervention in managing fatigue in metastatic breast cancer patients.
Methods:
Ninety-one patients with metastatic breast cancer were randomized to receive integrated yoga program (n = 46) or supportive therapy and education (n = 45) over a 3-month period. Assessments such as perceived stress, fatigue symptom inventory, diurnal salivary cortisol, and natural killer cell counts were carried out before and after intervention. Analysis was done using an intention-to-treat approach. Postmeasures for the above outcomes were assessed using ANCOVA with respective baseline measure as a covariate.
Results:
The results suggest that yoga reduces perceived stress (P = 0.001), fatigue frequency (P < 0.001), fatigue severity (P < 0.001), interference (P < 0.001), and diurnal variation (P < 0.001) when compared to supportive therapy. There was a positive correlation of change in fatigue severity with 9 a.m. salivary cortisol levels.
Conclusion:
The results suggest that yoga reduces fatigue in advanced breast cancer patients.
Keywords
Cortisol
fatigue
stress
supportive therapy
yoga
INTRODUCTION
The diagnosis and treatment of cancer can pose serious side effects and distress in cancer patients. This is more so when the cancer is at an advanced stage.[1] Among these manageable treatment-related symptoms associated with distress include menopausal/vasomotor symptoms, pain, fatigue, and sleep disturbance. There is a wide prevalence in fatigue symptoms among breast cancer patients ranging from 70% to 100%.[23] Cancer-related fatigue is perceived as being of greater magnitude, disproportionate to activity or exertion, and not completely relieved by rest, leaving the patient with an overwhelming and sustained sense of exhaustion.[4] Fatigue is an umbrella term used to describe various sensations or feelings, and a variety of expressions of reduced capacity at physical, mental, emotional, or social levels.[5]
Both physiological and psychosocial factors play a part in the development of fatigue. The physiological reasons for fatigue have been attributed to anemia, cancer therapy, nutritional deficiency, electrolyte disturbances, pain, neuropathy, sarcopenia, and cachexia. The biopsychosocial model attributes fatigue to psychologic distress that is known to exacerbate fatigue due to other causes as well. Cancer-related fatigue is associated with psychosocial factors, such as anxiety and depression,[67] difficulty in sleeping,[8] full-time employment status,[9] and low degrees of physical functioning.[10] However, whether it is a cause or an effect of these factors is unknown. Fatigue is also linked to high amounts of other unmanaged symptoms, especially pain.[11]
Perceived stress has been shown to be related to fatigue and treatment-related distress in cancer survivors.[12] Several others studies have shown a direct link between stress, insomnia, fatigue, and diurnal salivary cortisol rhythms.[13141516] Studies have shown that diurnal cortisol slope is an important predictor of survival in advanced breast cancer patients and is directly linked to depression.[17] Peak cortisol levels are also known to cause soft tissue pains and fatigue as seen in fibromyalgia. The hypothalamo-pituitary axes dysregulation is known to cause this change in rhythm as seen in both fibromyalgia patients and those with cancer due to chronic stress and allostatic load.[1518]
Evidence suggests that pain, fatigue, and depression are frequently undertreated. Patients and health-care providers have reported depression and persistent lack of energy as the aggressiveness of therapy has been increased and/or the underlying malignancy has worsened.[19] Cancer symptom management would benefit if an integrated intervention plan existed for a cluster of symptoms based on a clear understanding of which symptoms are likely to cluster, when clustering is likely to occur, and how a symptom cluster affects patient outcomes at different stages of treatment. Most of these symptom clusters are influenced by patients’ perception, awareness, education, mood states, and can be explained through various biologic, psychological, behavioral, and sociocultural mechanisms that constitute a symptom interaction network and symptom experience.[20] The experience of multiple simultaneous symptoms has a synergistic effect on symptom distress.[21]
Management of symptoms, therefore, requires a holistic approach that integrates behavioral and mind–body strategies, this is more so emphasized in earlier studies that have shown several stress reduction and mind–body approaches to reduce distressful symptoms and mood states in cancer patients.
Several studies have shown psychotherapeutic interventions such as supportive therapy, counseling, social support, and cognitive behavior therapy to reduce fatigue in cancer patients.[1422232425] Several other studies have shown exercise, physical activity, and energy conservation therapy to reduce fatigue in cancer survivors.[102627] Mind–body interventions such as yoga have been shown to reduce fatigue in early breast cancer survivors during treatment.[282930] Our earlier studies with yoga showed reduction in fatigue in early breast cancer patients undergoing radiotherapy.[3132] Earlier studies with yoga intervention are varied with different types of yogic intervention and duration. However, there is a paucity of studies showing effects of yogic intervention in reducing fatigue in advanced breast cancer patients.[3334]
In this study, we evaluated the effects of an integrated yoga program versus supportive therapy on perceived stress, fatigue in patients with advanced breast cancer. We also evaluated the relationship between fatigue and cortisol rhythms in metastatic breast cancer.
METHODS
In this study, 91 patients with metastatic breast cancer were recruited to participate in a trial comparing integrated yoga program with education and supportive therapy sessions from January 2004 to June 2007. Institutional Review Board of the participating institution approved the study. The participants were recruited if they satisfied the selection criteria and gave written consent to participate in the study. Patients were included in the study if they were diagnosed to have metastatic breast cancer and were between 30 and 70 years of age and had adequate performance status (ambulatory >50% of time). Patients were excluded from the study if they had brain metastases, underwent chemotherapy treatment with exception of bisphosphonate therapy, were pregnant or lactating, on hydrocortisone medications, participated in clinical trials involving investigational new drugs, etc., This was a prospective, two-arm, randomized controlled study comparing integrated yoga program with supportive therapy with randomization done using computer-generated random numbers and opaque envelopes with group assignments. More details regarding study procedure are mentioned elsewhere.
Sample size
The sample size was calculated based on an earlier study with Mindfulness Based Stress Reduction Program (MBSR) that had shown a modest effect size (ES = 0.38) on EORTC QLC30 global quality of life measure.[35] Based on an ES of 0.38 for ANOVA between factor effects with α = 0.05 and β = 0.2, the sample size thus required was 44 in each group. Considering dropouts, we recruited 46 patients in each group.
There were 65 study completers of yoga (n = 42) and supportive therapy (n = 33) in the study.
Interventions
The intervention group received “integrated yoga program” and the control group received “supportive counseling sessions” both imparted as individual sessions over a 3-month period. We developed an integrated yoga module comprising various practices that include asana (postures), pranayama (regulated nostril breathing), yogic relaxation in supine (shavasana), meditation, self-appraisal, and counseling. Practices such as pranic energization technique (positron emission tomography - observing the flow of energy or prana through the body), cyclic meditation - combination of postures and relaxation techniques done keeping eyes closed, and mind sound resonance technique (chanting of mantras verbally and mentally) were some of the specific techniques used in cancer patients. Details of both the interventions are given elsewhere (Raghavendra et al., 2009).[3637]
Outcome measures
At the initial visit before randomization, demographic information, medical history, clinical data, intake of medications, investigative notes, and conventional treatment regimen were ascertained from all consenting participants. The outcome measures ascertained could be grouped into the following categories:
Perceived stress scale
Perceived stress levels were assessed using perceived stress scale[38] questionnaire. This self-rated scale includes 14 items scored on a 5-point scale. This scale was used to assess the degree to which participants appraise their daily life as unpredictable, uncontrollable, and overwhelming over the last month. This has a reliability of 0.85.[38]
Fatigue symptom inventory
The fatigue symptom inventory (FSI), developed in the United States in 1998, is a 14-item self-report measure designed to assess the intensity (4 items), daily pattern (1 item), and duration of fatigue (2 items), as well as its impact on quality of life (7 items).[3940] Twelve items consist of 11-point Likert-type scale (0 = not at all fatigued; 10 = extremely fatigued) and 1 item is composed of the number of days in the past week the patients felt fatigued. However, one item related to daily pattern of fatigue provides qualitative information and is not included in the total fatigue score. The higher the total fatigue score, the more severe the level of fatigue. The scale development process involved a review of literature on fatigue in cancer patients and on chronic fatigue in general. Thus, the scale was intended to be used to compare fatigue in various groups of patients and normal healthy populations. Based on two previous studies, Cronbach's alpha coefficients of the subscale of FSI of impact on quality of life ranged from 0.93 to 0.95.[3940] The FSI has also demonstrated test–retest reliability, construct validity, divergent validity, convergent validity, and discriminant validity.[39]
RESULTS
Ninety-one metastatic breast cancer survivors (group mean age: 50.54 years ± 8.53 years) registered in hospital-based cancer registry of Bangalore Institute of Oncology were recruited for this study. The sociodemographic characteristics of the study sample were similar across groups.
Fatigue severity
Analysis of covariance on postmeasures using baseline fatigue severity score as a covariate showed a significant difference between groups with better decrease in fatigue severity in yoga compared to control group [F(1,61) = 32.55, P < 0.001, ES - 1.4, Percentage change (PC) - 61.15%]. Paired-sample t-test done to assess within-group change showed a significant decrease in fatigue severity in yoga group only (t = 6.7, P < 0.001) and not in the control group (t = −0.05, P = 0.96) [Table 1].
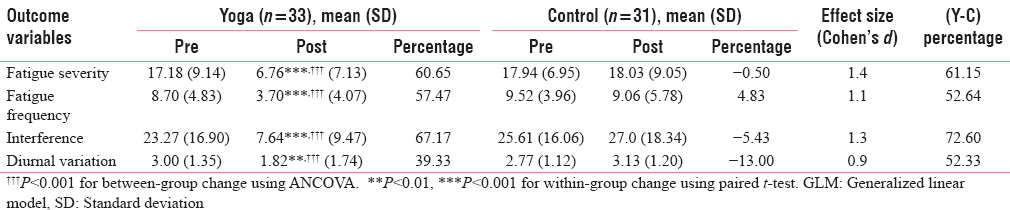
Fatigue frequency
Analysis of covariance on postmeasures using baseline fatigue frequency score as a covariate showed a significant difference between groups with better decrease in fatigue frequency in yoga compared to control group [F(1,61) = 17.81, P < 0.001, ES - 1.1, PC - 52.64%]. Paired-sample t-test done to assess within-group change showed a significant decrease in fatigue frequency in yoga group only (t = 5.8, P < 0.001) and not in the control group (t = 0.33, P = 0.74) [Table 1].
Fatigue interference
Analysis of covariance on postmeasures using baseline fatigue interference score as a covariate showed a significant difference between groups with better decrease in fatigue interference in yoga compared to control group [F(1,61) = 28.36, P < 0.001, ES - 1.3, PC - 72.6%]. Paired-sample t-test done to assess within-group change showed a significant decrease in fatigue interference in yoga group only (t = 5.5, P < 0.001) and not in the control group (t = −0.36, P = 0.72) [Table 1].
Fatigue diurnal variation
Analysis of covariance on postmeasures using baseline fatigue diurnal variation score as a covariate showed a significant difference between groups with better decrease in fatigue diurnal variation in yoga compared to control group [F(1,61) = 13.65, P < 0.001, ES - 0.9, PC - 52.33%]. Paired-sample t-test done to assess within-group change showed a significant decrease in fatigue diurnal variation in yoga group only (t = 3.8, P < 0.001) and not in the control group (t = −1.18, P = 0.24) [Table 1].
Perceived stress score
Nonparametric Mann–Whitney test done to assess between-group changes showed significant difference between groups with better decrease in self-report perceived stress in yoga compared to control group (z = −2.49, P = 0.01, ES - 1.4, PC - 32.57%). Nonparametric Wilcoxon test done to assess within-group change showed significant decrease in self-reported perceived stress in yoga group only (z = −3.46, P = 0.001) not in the control group (z = −0.62, P = 0.54) [Table 2].

Bivariate relationships
There was a significant positive correlation between changes in fatigue severity with change in 9 a.m. cortisol levels, indicating the stress reduction benefits of yogic intervention [Table 3].

DISCUSSION
The results from this study demonstrate a significant reduction in fatigue frequency, severity, interference, and diurnal fatigue variability in yoga group compared to supportive therapy intervention. There was also a significant decrease in perceived stress in yoga group compared to supportive therapy group. These findings are similar to earlier observations in early breast cancer patients with mindfulness-based[29] stress reduction and Iyengar yoga.[33]
Perceived stress
The results suggest an overall decrease in perceived stress scores with time in both the studies. In our study, yoga intervention reduced perceived stress by 32.6% (ES = 1.4) compared to control group. There is growing evidence that perceived stress has a major impact on the initiation and progression of disease, i.e., cardiovascular disease and chronic pain syndromes[4142] by downregulating the immune system, it is observed that greater perceived stress positively predicted salivary cortisol levels.[43]
Fatigue symptom inventory
In this study, there was a significant decrease in fatigue (61.2%, ES = 1.4), fatigue frequency (52.6%, ES = 1.5), fatigue interference (72.6%, ES = 1.3), and diurnal variation (52.3%, ES = 0.9) in yoga group compared to controls on FSI. Our results are in contrast to earlier studies that have shown a modest decrease in fatigue (5.7% following MBSR intervention on Profile of Mood States–fatigue subscale[35] and 6.4% on Functional Assessment of Chronic Illness Therapy fatigue scale in a study by Moadel et al.[44] This could be because of inadequacy of the subscale to measure various dimensions of fatigue[35] and use of yogic intervention in early-stage cancer patients where fatigue would not have been a main concern[44] contrary to our study where fatigue was measured in advanced breast cancer patients using a specific FSI. Fatigue is an important symptom in cancer patients that directly affects functional quality of life. Apart from clinical conditions that affect fatigue such as infections, anemia, and pain, progressive disease itself causes fatigue as a part of cancer cachexia through release of inflammatory cytokines. Therefore, managing fatigue is also an indication of clinical improvement in the patient's condition. The decrease in fatigue seen with our study and consequent reductions in morning salivary cortisol and improvement in natural killer (NK) cell counts support this understanding.
Adherence to intervention and outcomes
Adherence to intervention was good in our study with 80% attending 24 supervised sessions. There was a significant improvement in quality of life and decrease in 9 p.m. cortisol level in individuals with good adherence to intervention (attending >20 classes). Adherence to intervention in control group was 100%, as they had to invariably meet the counselors before appointment with their oncologists. This also explains why earlier studies did not have similar effects, as the number of sessions was very limited (9–12 sessions).[4546]
It may be hypothesized from these results that distress decreases with time in cancer patients, use of stress reduction interventions only augments this process and that, patients with initially high distress and high cortisol levels would probably take a longer time for attenuation of such high cortisol levels than those with lesser distress or cortisol profiles. These observations are important as hypothalamic-pituitary-adrenal (HPA) axes dysregulation in terms of diurnal salivary cortisol rhythm was found to be an important predictor for survival in advanced breast cancer patients.[17] The changes in stress response patterns and appraisal could have contributed to reductions in cortisol and distress seen with our intervention. The reduction in perceived stress seen with our intervention further offers support for this mechanism. An elevated level of cortisol is known to have immunosuppressive effects and is largely responsible for the downregulation of immune function because of stress. Reduction seen in cortisol levels in our study offers further support for improvements in immune functioning (NK cell counts) seen in our study in yoga group (32.4%, ES = 0.5) as also seen with our earlier study.[47] The combination of physical postures, breathing exercises, relaxation, and meditation could have helped attenuate cortisol levels through stress reduction and exercise effect as earlier studies have documented quality of life and biological benefits in cancer patients after moderate exercise.[4849] Various components of yoga intervention are known to have a calming effect and correct the autonomic imbalance[505152] and HPA axes disturbances[35] that prelude stress responses. Overall, the reduced psychological stress and cortisol following yoga program could be attributed to stress reduction rather than mere social support and education in conformity with earlier studies.[53]
The ability to “unwind” after stressful encounters, i.e., the ability to return to ones neuroendocrine baseline influences the total burden that the stressors place on the individual.[54] Decrement in NK cell counts has been found to be an important predictor for survival in advanced breast cancer. Catecholamines and glucocorticoids have been shown to rapidly and markedly affect the distribution of NK cells among different immune compartments (e.g., spleen, liver, lungs, circulating blood, marginating pool of blood, etc.),[5556] and it may be hypothesized that changes in these hormone levels and NK cell counts could be one of the mechanisms of action of our intervention.
Larger randomized controlled trials are needed to further validate the findings and effects of yoga intervention on HPA axes dysregulation.
CONCLUSION
In summary, our yoga-based intervention was effective in reducing psychological morbidity, distressful symptoms, toxicity, and improving the quality of life in early breast cancer patients undergoing conventional cancer treatments. This was probably facilitated through stress reduction and helping the cancer patients to cope better with their illness at various stages of their conventional treatment. However, larger randomized controlled trails with structured psychiatric interventions as controls are needed to further validate our findings.
Financial support and sponsorship
This study was supported with grants from the Central Council for Research in Yoga and Naturopathy, Ministry of AYUSH, Government of India.
Conflicts of interest
There are no conflicts of interest.
Ackowledgments
Central Council for Research in Yoga and Naturopathy, Ministry of AYUSH, Govt of India
REFERENCES
- Psychological reactions to progression of metastatic breast cancer – An interview study. Cancer Nurs. 2009;32:55-63.
- [Google Scholar]
- Impact of cancer-related fatigue on the lives of patients: New findings from the Fatigue Coalition. Oncologist. 2000;5:353-60.
- [Google Scholar]
- A qualitative study to explore the concept of fatigue/tiredness in cancer patients and in healthy individuals. Eur J Cancer Care (Engl). 1996;5(2 Suppl):8-23.
- [Google Scholar]
- Fatigue in patients with cancer. Analysis and assessment. Recent Results Cancer Res. 1998;145:1.
- [Google Scholar]
- Pain, psychological distress, health status, and coping in patients with breast cancer scheduled for autotransplantation. Oncol Nurs Forum. 1999;26:1337-45.
- [Google Scholar]
- Effects of exercise on fatigue, physical functioning, and emotional distress during radiation therapy for breast cancer. Oncol Nurs Forum. 1997;24:991-1000.
- [Google Scholar]
- The influence of daytime inactivity and nighttime restlessness on cancer-related fatigue. Oncol Nurs Forum. 1999;26:1663-71.
- [Google Scholar]
- Fatigue and its associated factors in ambulatory cancer patients: A preliminary study. J Pain Symptom Manage. 1999;17:42-8.
- [Google Scholar]
- Fatigue and quality of life outcomes of exercise during cancer treatment. Cancer Pract. 2001;9:119-27.
- [Google Scholar]
- Correlates of fatigue in people with breast or lung cancer. Oncol Nurs Forum. 1991;18:81-7.
- [Google Scholar]
- Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psychooncology. 2009;18:1273-80.
- [Google Scholar]
- Flattened cortisol rhythms in metastatic breast cancer patients. Psychoneuroendocrinology. 2004;29:1082-92.
- [Google Scholar]
- Cognitive-behavioral stress management reduces serum cortisol by enhancing benefit finding among women being treated for early stage breast cancer. Psychosom Med. 2000;62:304-8.
- [Google Scholar]
- Repression and high anxiety are associated with aberrant diurnal cortisol rhythms in women with metastatic breast cancer. Health Psychol. 2004;23:645-50.
- [Google Scholar]
- Depressive symptoms and inflammation are independent risk factors of fatigue in breast cancer survivors. Psychol Med. 2017;47:1733-43.
- [Google Scholar]
- Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92:994-1000.
- [Google Scholar]
- Hypothalamic-pituitary-adrenal axis perturbations in patients with fibromyalgia. Arthritis Rheum. 1994;37:1583-92.
- [Google Scholar]
- National Institutes of Health State-of-the-Science Conference Statement: Symptom management in cancer: Pain, depression, and fatigue, July 15-17, 2002. J Natl Cancer Inst. 2003;95:1110-7.
- [Google Scholar]
- Symptom interactions as mechanisms underlying symptom pairs and clusters. J Nurs Scholarsh. 2005;37:209-15.
- [Google Scholar]
- The middle-range theory of unpleasant symptoms: An update. ANS Adv Nurs Sci. 1997;19:14-27.
- [Google Scholar]
- Effects of supportive-expressive group therapy on pain in women with metastatic breast cancer. Health Psychol. 2009;28:579-87.
- [Google Scholar]
- Responsiveness to change [corrected] due to supportive-expressive group therapy, improvement in mood and disease progression in women with metastatic breast cancer. Qual Life Res. 2007;16:1007-17.
- [Google Scholar]
- Group coping skills instruction and supportive group therapy for cancer patients: A comparison of strategies. J Consult Clin Psychol. 1986;54:802-8.
- [Google Scholar]
- Social support and salivary cortisol in women with metastatic breast cancer. Psychosom Med. 2000;62:337-45.
- [Google Scholar]
- Aerobic physical exercise for adult patients with haematological malignancies. Cochrane Database Syst Rev. 2014;11:CD009075.
- [Google Scholar]
- Do yoga and aerobic exercise training have impact on functional capacity, fatigue, peripheral muscle strength, and quality of life in breast cancer survivors? Integr Cancer Ther. 2015;14:125-32.
- [Google Scholar]
- Feasibility of conducting a clinical trial on Hatha yoga for chronic low back pain: Methodological lessons. Altern Ther Health Med. 2004;10:80-3.
- [Google Scholar]
- Effects of yoga interventions on fatigue in cancer patients and survivors: A systematic review of randomized controlled trials. Explore (NY). 2013;9:232-43.
- [Google Scholar]
- Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med. 2008;14:637-44.
- [Google Scholar]
- Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integr Cancer Ther. 2007;6:242-50.
- [Google Scholar]
- Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: A randomized controlled trial. Integr Cancer Ther. 2009;8:37-46.
- [Google Scholar]
- Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23:135-42.
- [Google Scholar]
- Mindful Yoga for women with metastatic breast cancer: Design of a randomized controlled trial. BMC Complement Altern Med. 2017;17:153.
- [Google Scholar]
- Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448-74.
- [Google Scholar]
- Influence of yoga on mood states, distress, quality of life and immune outcomes in early stage breast cancer patients undergoing surgery. Int J Yoga. 2008;1:11-20.
- [Google Scholar]
- Effects of yoga on symptom management in breast cancer patients: A randomized controlled trial. Int J Yoga. 2009;2:73-9.
- [Google Scholar]
- Measurement of fatigue in cancer patients: Development and validation of the Fatigue Symptom Inventory. Qual Life Res. 1998;7:301-10.
- [Google Scholar]
- A multidimensional measure of fatigue for use with cancer patients. Cancer Pract. 1998;6:143-52.
- [Google Scholar]
- Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:953-62.
- [Google Scholar]
- Stress management: A randomized study of cognitive behavioural therapy and yoga. Cogn Behav Ther. 2006;35:3-10.
- [Google Scholar]
- Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. J Clin Oncol. 2007;25:4387-95.
- [Google Scholar]
- Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571-81.
- [Google Scholar]
- Effects of Hatha yoga and African dance on perceived stress, affect, and salivary cortisol. Ann Behav Med. 2004;28:114-8.
- [Google Scholar]
- Effects of yoga on natural killer cell counts in early breast cancer patients undergoing conventional treatment. Comment to: Recreational music-making modulates natural killer cell activity, cytokines, and mood states in corporate employees Masatada Wachi, Masahiro Koyama, Masanori Utsuyama. Med Sci Monit. 2008;14:LE3-4.
- [Google Scholar]
- Exercise interventions during cancer treatment: Biopsychosocial outcomes. Exerc Sport Sci Rev. 2001;29:60-4.
- [Google Scholar]
- Physical exercise and quality of life following cancer diagnosis: A literature review. Ann Behav Med. 1999;21:171-9.
- [Google Scholar]
- Oxygen consumption and respiration following two yoga relaxation techniques. Appl Psychophysiol Biofeedback. 2000;25:221-7.
- [Google Scholar]
- Autonomic changes while mentally repeating two syllables – One meaningful and the other neutral. Indian J Physiol Pharmacol. 1998;42:57-63.
- [Google Scholar]
- Autonomic changes during “OM” meditation. Indian J Physiol Pharmacol. 1995;39:418-20.
- [Google Scholar]
- Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2:888-91.
- [Google Scholar]
- Pace variation and control of work pace as related to cardiovascular, neuroendocrine, and subjective responses. Biol Psychol. 1986;23:247-63.
- [Google Scholar]
- Effects of beta-adrenergic blockade on immunologic and cardiovascular changes induced by mental stress. Circulation. 1994;89:762-9.
- [Google Scholar]
- Effects of stress on immune cell distribution. Dynamics and hormonal mechanisms. J Immunol. 1995;154:5511-27.
- [Google Scholar]






