Translate this page into:
End-of-Life Milieu of Critically Sick Children Admitted to a Pediatric Hospital: A Comparative Study of Survivors versus Nonsurvivors
Address for correspondence: Dr. Bhavneet Bharti, Department of Pediatrics, Advanced Pediatrics Center, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012, India. E-mail: bhavneetsahul@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The aim of this study was to describe end-of-life (EOL) milieu among caregivers of children who died in the hospital and to compare their psychosocial, spiritual, and financial concerns with caregivers of children who survived.
Materials and Methods:
Sixty caregivers of children (30 survivors and 30 nonsurvivors), admitted in the pediatric intensive care unit and general pediatric unit, were recruited over a period of 1 year. Mixed qualitative methods were used to collect information from parents on EOL care perspectives.
Results:
Demographic, disease, and treatment-related characteristics were not significantly different between nonsurvivor and survivor groups. The caregivers of nonsurvivors versus survivors showed no significant differences as regards optimal care (76.67% vs. 56.67%), social support (76.6% vs. 66.67%), and frequent recitation of scriptures (30.77% vs. 45.83%). Mean medical expenditure among children receiving EOL care was Rs. 40,883 (range: Rs. 800–5 lakhs). Regression results revealed that for every 1 day of increase in hospital stay, cost of hospitalization for dying children increased by Rs. 3000 (P = 0.0001). Medical insurance was reported by only minority of the cases (5%). Several themes emerged in the focus group discussions with care providers which highlighted the importance of communication and need for emotional, social, and financial support. EOL decision was taken in only two of the nonsurviving children.
Conclusions:
The study offers useful insight about social, financial, and religious “end-of-life” needs among terminally sick children and thereby sensitizes the health-care providers to optimize their care at this niche period.
Keywords
End-of-life care
financial
psychosocial needs
religious
sick children
INTRODUCTION
Loss of a child to an illness (end-of-life [EOL]) is a crisis which is fraught with multitude of psychosocial stresses for the family as well as their health-care providers.[123] Unrestrained medical interventions can prolong parental suffering needlessly and also result in serious neglect of family's ethical and cultural values. In a recently published meta-summary of 21 qualitative and survey-based studies on the needs of children and their families facing EOL, Stevenson et al. identified ten patient and family needs. These needs included needs related to health-care delivery and accessibility, information, bereavement, psychosocial, spiritual, cultural, and decision-making.[4]
There is surprisingly little research from developing countries, including India, on EOL and palliative care for children to guide pediatricians to improve parent/care provider experience,[56] though few studies are available on adults.[789] In India, parents are accorded little autonomy in taking medical decisions, primarily due to lacunae in pediatric medical training, wherein the emphasis is on curative approach to disease rather than on palliative care, even when the patient's prognosis is poor. In addition, a pediatrician may be unsure of what constitutes optimal management in EOL care as there are few legal guidelines for treating patients in intensive care units. Indeed, laws with respect to death with dignity in India are unclear, wherein laws in the developing countries have evolved over time to accommodate the changing paradigm.[1011]
Clearly then, there is a need to study the unique financial, psychological, and social constraints faced by Indian parents to enhance our understanding of caregiver perspectives when they face the death of their child. This will, indeed, be valuable to develop EOL care services in Indian pediatric centers. Keeping this in mind, the aim of the present study was to describe the EOL milieu among caregivers of children who die in the hospital and to compare the psychosocial, spiritual, and financial concerns of parents of children who died and those who survived.
MATERIALS AND METHODS
The study children were enrolled in the pediatric emergency where they were systematically prioritized using Modified Emergency Severity Index triage algorithm which yields reliable and valid stratification of patients into five levels such as resuscitation, emergent, urgent, less urgent, and nonurgent. The children categorized as resuscitation/emergent were followed up till the desired outcome, i.e., death/discharge. The first interview of the caregivers took after 48 h of hospitalization in the pediatric intensive care unit or in the wards. At the first interview, it was not clear whether a given patient would be designated as a case (nonsurvivor) or control (survivor), but we prospectively enrolled and followed every critically sick and eligible child till death or discharge. This process continued till we had the requisite sample size of 30 in each study arm. In addition, 2–4 more interviews were conducted for participants in both the study groups depending on their length of stay in hospital. No caregiver was interviewed after discharge/death of their admitted child.
Inclusion criteria included children who presented with the following conditions: fever with altered consciousness/behavior, toxicity, body temperature >40°C, hypothermia, unconsciousness, sudden paralysis, respiratory distress, slow/irregular breathing, stridor, obstructed airway, severe diarrhea and/or vomiting, acute bleeding or sudden worsening of previously known illness, age range 2 months–12 years, and hospital stay of at least 48 h. Children admitted with accidents/trauma or whose illnesses had medicolegal ramifications were excluded. The study was cleared by the Institute's Ethics Committee, and a written informed consent from parents was obtained before enrollment.
Tool used
Mixed qualitative methods (observations, semi-structured questionnaire, and rich narrative interviews) were used to collect information from parents on EOL care perspectives. The interviews were conducted in two to four sittings and were audio-taped and transcribed later. The questionnaire elicited information on financial, behavioral, psychosocial, and religious concerns of parents. EOL decisions, if any, were recorded either from the medical records or from the interviews. These decisions were categorized into the following categories: palliative care, do-not-resuscitate order, withholding support, left against medical advice, and discharged on request.
Statistical analysis
Descriptive statistics included measures of central tendency and dispersion for quantitative variables and frequency/proportions for categorical variables. Shapiro–Wilk tests and Q–Q plots were used to test the normality of data. Group comparisons were done either by Chi-square test for independence (categorical variables) or Mann–Whitney U-test (quantitative variables). Regression analysis was carried out to predict hospitalization cost and other care-related outcomes. The level of agreement between treating pediatricians and parents was assessed using the kappa statistics. All tests were two-tailed, and P < 0.05 was taken as statistically significant. Statistical analysis was performed using Stata IC version 14 (StataCorp., LLC, Texas, USA).
RESULTS
The flow chart for recruitment of the two groups is presented in Figure 1. The demographic characteristics of the study cohort are presented in Table 1. The two study groups were matched on socioeconomic and demographic characteristics, and there were no statistically significant group differences on age, sex, birth order, education level of father, and socioeconomic status. The children were in the age range of 2 months–12 years (median age: 4 years; interquartile range [IQR]: 8 years). The sample predominantly consisted of upper-lower and lower-middle socioeconomic status families, with low levels of education. Main occupations reported were labor and farming, and few respondents were from the service/business sector. The disease and treatment characteristics of the sample are shown in Table 1. No significant differences emerged between the survivor and nonsurvivor groups.
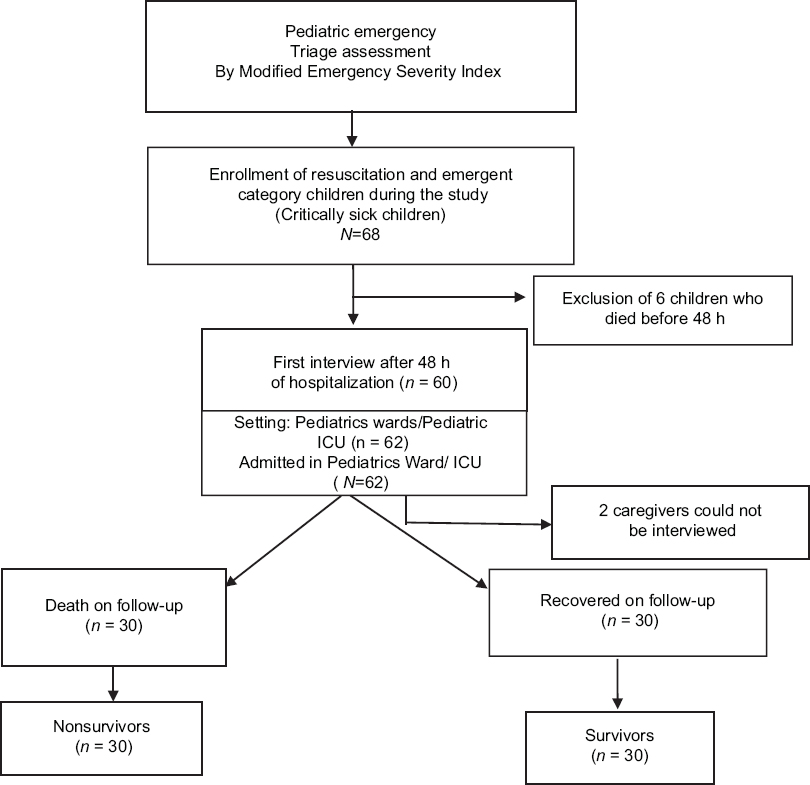
- Flowchart showing the study plan
| Total (n=60), n (%) | Nonsurvivors (n=30), n (%) | Survivors (n=30), n (%) | P | |
|---|---|---|---|---|
| Age (years), median (IQR) | 4 (8) | 2.5 (8) | 4.5 (8.25) | 0.48 |
| Gender | ||||
| Female | 26 (43.3) | 15 (50.0) | 11 (36.7) | 0.29 |
| Male | 34 (56.7) | 15 (50.0) | 19 (63.3) | |
| Religion | ||||
| Hindu | 42 (70.0) | 21 (70.0) | 21 (70.0) | 0.53 |
| Sikhism | 14 (23.3) | 8 (26.7) | 6 (20.0) | |
| Muslim | 4 (6.7) | 1 (3.3) | 3 (10.0) | |
| Educational level | ||||
| No education | 10 (16.67) | 5 (16.67) | 5 (16.67) | 0.85 |
| Primary | 30 (50) | 14 (46.67) | 16 (53.33) | |
| Secondary and higher | 20 (33.33) | 11 (36.66) | 9 (30) | |
| Occupation | ||||
| Laborer | 20 (33.33) | 11 (36.67) | 9 (30) | 0.47 |
| Farmer | 16 (26.67) | 9 (30) | 7 (23.33) | |
| Business | 6 (10) | 4 (13.33) | 2 (6.67) | |
| Government job | 10 (16.67) | 4 (13.33) | 6 (20) | |
| Others | 8 (13.33) | 2 (6.67) | 6 (20) | |
| Income (Rs), median (IQR) | 6000 (7000) | 6000 (5000) | 6000 (9750) | 0.67 |
| Socioeconomic status | ||||
| Low | 1 (1.7) | 0 (.0) | 1 (3.3) | 0.92 |
| Upper lower | 32 (53.3) | 16 (53.3) | 16 (53.3) | |
| Lower middle | 20 (33.3) | 10 (33.3) | 10 (33.3) | |
| Upper middle | 7 (11.7) | 4 (13.3) | 3 (10.0) | |
| High | 0 (0) | 0 (0) | 0 (0) | |
| Birth order | 0.87 | |||
| First | 21 (35) | 10 (33.33) | 11 (36.67) | |
| Second | 24 (40) | 13 (44.34) | 11 (36.67) | |
| >2 | 15 (25) | 7 (23.33) | 8 (26.66) | |
| Diagnosis | ||||
| Infectious | 28 (46.67) | 12 (40) | 15 (50) | 0.65 |
| Neoplastic | 8 (13.33) | 5 (16.67) | 3 (10.0) | |
| Others | 24 (40.0) | 13 (43.33) | 12 (40.0) | |
| Length of stay (days), median (IQR) | 15 (10) | 15.5 (11) | 15 (13.5) | 0.89 |
| Out-of-pocket expenditure in hospital (rupees), median (IQR) | 22500 (35000) | 30000 (32750) | 10000 (23250) | 0.70 |
| Out-of-pocket expenditure before admission (rupees), median (IQR) | 70000 (14250) | 13000 (14000) | 6500 (17000) | 0.20 |
| Proportion of poor free admission files | 23 (38.3) | 15 (50.0) | 8 (26.7) | 0.06 |
| Number of children privately insured | 3 (5.0) | 3 (10.0) | 0 (0) | 0.08 |
| Help received from various charitable and social welfare organizations | 8 (13.3) | 3 (10.0) | 5 (16.7) | 0.45 |
IQR: Interquartile range
The median duration of hospital stay was 15 days (IQR: 10 days). Hospital charges were waived off by the hospital for a little more than one-third (38%) of the patients. Overall, median hospital medical expenditure reported was Rs. 22,500 (IQR: 35,000), and median expenditure before admission to the hospital was Rs. 70,000 (IQR: 14,250). Three-fourth reported not anticipating the high costs associated with hospital admission. Medical insurance was reported by minority of the cases (5%). Majority of the parents (91.7%) reported borrowing money, and 5.2% reported that they had sold their assets to meet the costs of caring for their sick child. Some (11.7%) parents reported that escalating financial burden was forcing them to consider getting their child discharged against medical advice, and 7% caregivers reported that they had been refused financial help by their relatives/friends. Only a minority (8%) of the families had taken financial aid from charitable and social organizations. Loss of wages was reported by majority (72%) of the parents, and mean days of wages lost reported were 24.54 days (standard deviation = 15). Regression results revealed that for every 1 day of increase in hospital stay, cost of hospitalization of dying children increased by Rs. 3000 (P = 0.0001). It may be noted that costs only including expenditure on drugs and disposables, incidental expenses on food, transport, and other miscellaneous expenditures were not included while computing financial costs. None of the families were covered under the National Health Insurance Scheme which is currently available in India to protect economically weaker sections from out-of-pocket health expenditure.
Majority of the caregivers reported being satisfied with the medical care (66.7%) and were well informed (83.3%) about the possibility of a child's death. No significant group differences were found on satisfaction with care, social support, and recitation of religious scriptures [Table 2]. Odds of reporting of suboptimal care were indeed decreased by 60% among caregivers of nonsurvivors as compared to survivors (odds ratio [OR]: 0.40, 95% confidence interval [CI]: 0.13–1.21), but this difference was not statistically significant (P = 0.10). Odds of reciting scriptures in the hospital were also not statistically different between caregivers of nonsurvivors as compared to survivors (OR: 0.52, 95% CI: 0.16–1.67, P = 0.28). Similarly, caregivers of nonsurvivors reported lower, yet nonsignificant, odds of suboptimal social support (OR: 0.61; 95% CI: 0.20–1.90, P = 0.39). Social pressure for seeking medical treatment from an alternative health-care setup was rarely reported (3.3%), and only a few parents (8.3%) blamed the treating medical team for worsening of their children's condition at the hospital.
| Total (n=60), n (%) | Nonsurvivors (n=30), n (%) | Survivors (n=30), n (%) | P | |
|---|---|---|---|---|
| Satisfaction with level of care | ||||
| Completely | 40 (66.7) | 23 (76.7) | 17 (56.7) | 0.28 |
| Mostly | 10 (16.7) | 2 (6.7) | 8 (26.7) | |
| Fairly | 2 (3.3) | 1 (3.3) | 1 (3.3) | |
| Little | 3 (5.0) | 2 (6.7) | 1 (3.3) | |
| Not at all | 5 (8.3) | 2 (6.7) | 3 (10.0) | |
| Belief of doctor being truthful | ||||
| Completely | 45 (83.3) | 24 (85.7) | 21 (80.8) | 0.12 |
| Mostly | 5 (9.3) | 4 (14.3) | 1 (3.8) | |
| Fairly | 2 (3.7) | 0 (0) | 2 (7.7) | |
| Not at all | 2 (3.7) | 0 (0) | 2 (7.7) | |
| Satisfaction with social support | ||||
| Completely | 43 (71.7) | 23 (76.7) | 20 (66.7) | 0.13 |
| Mostly | 1 (1.7) | 1 (3.3) | 0 (0) | |
| Fairly | 5 (8.3) | 2 (6.7) | 3 (10.0) | |
| Little | 6 (10.0) | 4 (13.3) | 2 (6.7) | |
| Not at all | 5 (8.3) | 0 (0) | 5 (16.7) | |
| Support to attend child at night | ||||
| Not at all | 5 (8.3) | 4 (13.3) | 1 (3.3) | 0.21 |
| Little | 6 (10.0) | 2 (6.7) | 4 (13.3) | |
| Fair | 6 (10.0) | 5 (16.7) | 1 (3.3) | |
| High | 3 (5.0) | 1 (3.3) | 2 (6.7) | |
| Significant | 40 (66.7) | 18 (60.0) | 22 (73.3) | |
| Frequency of prayer | ||||
| Not at all | 8 (13.3) | 6 (20.0) | 2 (6.7) | 0.07 |
| Little bit | 27 (45.0) | 10 (33.3) | 17 (56.7) | |
| Some extent | 3 (5.0) | 3 (10.0) | 0 (0) | |
| Frequently | 15 (25.0) | 9 (30.0) | 6 (20.0) | |
| Always | 7 (11.7) | 2 (6.7) | 5 (16.7) | |
| Consulted astrologer | 10 (16.7) | 4 (13.3) | 6 (20.0) | 0.48 |
| Tied holy thread | 22 (36.7) | 12 (40.0) | 10 (33.3) | 0.59 |
| Brought any spiritual leader in hospital | 2 (3.5) | 2 (7.4) | 0 (0) | 0.13 |
| Recite any religious scripture in hospital | ||||
| Not at all | 2 (4.0) | 2 (7.7) | 0 (0) | 0.12 |
| Occasionally | 25 (50.0) | 12 (46.2) | 13 (54.2) | |
| Sometimes | 4 (8.0) | 4 (15.4) | 0 (0) | |
| Frequency | 12 (24.0) | 6 (23.1) | 6 (25.0) | |
| Daily | 7 (14.0) | 2 (7.7) | 5 (20.8) |
Several themes emerged in the focus group discussions with care providers which highlighted the importance of communication, need for emotional, social, and financial support, empathy, and spirituality [Table 3]. Caregivers expressed the need for honesty in information provided, manner of communication, and time constraints. Few parents (10%) opined that care providers did not listen to their concerns, and communication was often physician dominated and full of medical jargon. Parents reported that care providers rarely asked them about their goals and preferences. Parents opined that they would appreciate truthful and easy to comprehend information provided in an individualized and caring manner by care providers. A significant relationship between communication of the current status of the child and survival outcome was found. Parents, whose children subsequently died, reported higher odds of delayed update (>24 h) in compared to parents of survivors (relative risk: 4.30; 95% CI: 0.81–22.80), and this difference showed trend for significance (P = 0.09).
| Financial Constraints P3 (Father): I have borrowed money from my owner where I work, now he refuses to give more. I do not blame him, as I have borrowed a lot. Now I have finished all my money, but there is no end in sight as the medical expenses are unending. I have nothing left P8 (Father): I have already spent a lot of money (1.5 lakhs approximately) and the costs keep mounting. I can borrow money but then I should feel that the child is improving, or I should be reassured that the child will recover, without this hope and reassurance, I do not want to incur financial debt and be in more trouble P17 (Mother): Till date I have spent Rs. 6 lakhs for his treatment. I have taken a loan from a neighbor at a high interest. My family has also loaned us money for the treatment. I have mortgaged my land, my house, ……. What should I sell now? Should I sell my child now? There is hardly any improvement ……….I just do not want to continue the treatment as I have no more money |
| Lack of Social Support P7 (Mother): No neighbors or relatives are there to help me in my time of crisis. I alone have to take care of my child around the clock, send investigations, run for reports, and talk to the doctors. Her father is also not bothered, maybe because she is a girl P17 (Father): Gradually all my relatives are leaving us due to the child’s prolonged hospitalization. They have lost all hope. We are finding it extremely difficult to continue his treatment |
| Faith in God and Rituals P25: We have visited many temples to pray for our child’s recovery. I have great faith in God and I am sure there is a reason behind our suffering. The temple priest has advised us to give “daan” (donation) equal to the child’s weight. We have already distributed that much amount of grain to the needy. In addition, we have donated a cow. I am willing to donate more as long as my child recovers P10: I have visited the “pirbaba’s dargah” and vowed “chadar chadhanna” if my child recovers from his illness. I have also tied a holy thread …………carried out many other religious rituals. All rituals cost money and I have already spent Rs. 2500. |
| Belief in Astrology and Faith healers P13 (Father): I have visited many astrologers and one of the astrologers told me that three-fourth of my child is destroyed and very little of my child is intact. I have great faith in this astrologer and after his prediction, I have lost all faith in the doctors. I don’t believe my child will recover so why should I continue with his treatment and spend more time and money? P2 (Father): “Maine jharwaya tha, lekin koi farak nahi para” (I have even carried out rituals advised by faith healers and it has made little difference to my child’s condition). |
| Communication issues P9 (Father): The doctor tells us that our child has improved considerably (80%), but we feel our child has not improved at all. The doctor talks in a language that we find difficult to comprehend. We are apprehensive about asking the doctors too many questions and clarifications as they are busy and we do not want to annoy them P15 (Mother): I have repeatedly asked the doctors and nurses to tell me why my child is the way he is, but no one clarifies my doubts. Maybe they have no answers |
Good communication between parents facing EOL crisis was found to be a key component related to satisfaction with care, and this aspect of care was repeatedly emphasized by parents in the focused open-ended discussions. Agreement between treatment team and parents regarding the prognosis of the child and current condition of the child was also examined. High level of agreement was found regarding the prognosis of the hospitalized child (kappa = 0.87); however, only moderate agreement was found regarding the current condition of the admitted children (kappa = 0.57).
Nearly two-third parents of hospitalized children reported a significant social support at night, and only 18.3% complained about poor or no social support during night time. Most parents took recourse to religion to cope with the EOL crisis, little more than one-third (36.7%) reported tying a sacred thread, one-fifth (20%) reported visiting shrines, 16.7% consulted astrologers, and 3% had a religious person visiting their seriously sick child in the hospital. Only 38% prayed on a regular basis, and lack of a dedicated space for praying was cited as the primary reason.
EOL decision was taken in only two of the nonsurviving children. One was a case of snake envenomation, and the second decision was taken by parents of a child with idiopathic diffuse alveolar hemorrhage with acute respiratory distress syndrome. None of the parents gave consent for autopsy or organ donation.
DISCUSSION
This case–control study describes parental experiences related to EOL care among nonsurvivor children, with a range of underlying medical illnesses, in a tertiary care government hospital in North India. Higher financial costs and need for additional financial resources were voiced by nearly all parents. However, majority of the parents were found to be satisfied with communication and care provided by the health-care providers. Previous studies which have examined communication in critical care settings have emphasized the importance of honesty, comprehensiveness of information, accessibility, and attention to parental emotions.[121314] Indeed, good communication between parents and the treating team has been identified as critical for reducing parental distress before and after the loss as well as for improving parental satisfaction of treatment.[1215]
EOL decisions were taken by only two families. The rates found in the present study are substantially lower than found in the research conducted in the developed countries as decisions regarding withholding of support due to medical futility are rarely taken in India.[916] For example, Guglani and Lodha (2005) noted that most pediatricians are unaware of the EOL guidelines and many still view withholding of support as being ethically different from active withdrawal of support. Several legal battles in India have not upheld familial decision of limitation/withdrawal of life support as it is perceived against the spirit of Article 21 of the Indian Constitution.
Focused discussions in our study shed some light on the difficulties faced by physicians surrounding withdrawal of life support including lack of safeguards in the form of institutional guidelines, indecisiveness of parents, and religious, cultural, and social barriers. Several recurring themes emerged in focus group discussions with families related to their psychological, spiritual, and financial needs which need to be addressed to provide sensitive EOL care. Previous studies too have emphasized the need for conducting spiritual assessments with the child and family as a salient aspect EOL care.[1718] In fact, clinicians generally underestimate the role of spirituality and religion in medical decision-making of families.[1920]
The study has a few limitations. First, the findings cannot be generalized to all hospitals in the country due to variable health-care systems in India, particularly differences between the private and the public sectors. Additional research is needed with a more socioeconomically diverse sample. Clearly, more work is needed in the pediatric critical and palliative care in the developing countries to understand how best to provide comprehensive care to dying children and their families in order to alleviate human suffering and reduce unnecessary economic and psychosocial costs to children and their families.
CONCLUSION
Our study unmasked the unmet financial, psychological, religious and social needs to improve the end-of-life care of hospitalized children with critical illness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the help of our social worker Ms. Suman Gautam in assisting the investigators in taking interviews during the difficult times of the families.
REFERENCES
- When a child dies: Parents’ experiences of palliative care-an integrative literature review. J Pediatr Nurs. 2014;29:660-9.
- [Google Scholar]
- Integrative review: Parent perspectives on care of their child at the end of life. J Pediatr Nurs. 2012;27:514-22.
- [Google Scholar]
- Traditional expectations versus US realities: First- and second-generation Asian Indian perspectives on end-of-life care. J Gen Intern Med. 2012;27:311-7.
- [Google Scholar]
- Pediatric palliative care in Canada and the United States: A qualitative metasummary of the needs of patients and families. J Palliat Med. 2013;16:566-77.
- [Google Scholar]
- Attitudes towards end-of-life issues amongst pediatricians in a tertiary hospital in a developing country. J Trop Pediatr. 2008;54:261-4.
- [Google Scholar]
- What influences parents’ decisions to limit or withdraw life support? Pediatr Crit Care Med. 2005;6:513-8.
- [Google Scholar]
- End-of-life issues for a modern India – Lessons learnt in the West. Indian J Crit Care Med. 2005;9:81-5.
- [Google Scholar]
- End-of-life decisions in an Indian intensive care unit. Intensive Care Med. 2009;35:1713-9.
- [Google Scholar]
- Constitutional and legal provisions in Indian law for limiting life support. Indian J Crit Care Med. 2005;9:108-14.
- [Google Scholar]
- Limitation of life support in the ICU: Ethical issues relating to end-of-life care. Indian J Crit Care Med. 2003;7:112-7.
- [Google Scholar]
- Symptoms and suffering at the end of life in children with cancer. N Engl J Med. 2000;342:326-33.
- [Google Scholar]
- Communication in pediatric critical care: A proposal for an evidence-informed framework. J Child Health Care. 2016;20:27-36.
- [Google Scholar]
- Parents’ perspectives on physician-parent communication near the time of a child's death in the pediatric intensive care unit. Pediatr Crit Care Med. 2008;9:2-7.
- [Google Scholar]
- Family perspectives on the quality of pediatric palliative care. Arch Pediatr Adolesc Med. 2002;156:14-9.
- [Google Scholar]
- Limitation and withdrawal of intensive therapy at the end of life: Practices in intensive care units in Mumbai, India. Crit Care Med. 2005;33:1272-5.
- [Google Scholar]
- Taking a spiritual history allows clinicians to understand patients more fully. J Palliat Med. 2000;3:129-37.
- [Google Scholar]
- Spiritual care of families in the intensive care unit. Crit Care Med. 2007;35:1084-90.
- [Google Scholar]
- Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med. 1999;159:1803-6.
- [Google Scholar]
- Importance of faith on medical decisions regarding cancer care. J Clin Oncol. 2003;21:1379-82.
- [Google Scholar]






