Translate this page into:
Essential Elements of Home-based Palliative Care Model: A Rapid Review
*Corresponding author: Mousami Kirtania, Department of Public Health, School of Medical Sciences, University of Hyderabad, Hyderabad, Telangana, India. mousmikirtania15@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kirtania M, Katta A. Essential Elements of Home-based Palliative Care Model: A Rapid Review. Indian J Palliat Care 2023;29:359-67.
Abstract
The need for palliative care is increasing due to the rising burden of non-communicable diseases and some communicable diseases. Chronic illnesses demand patient-centred care that focuses on the patient’s individual healthcare needs. Palliative care improves the patients’ and caregivers’ quality of life by providing pain and symptom relief through a holistic approach after the disease is diagnosed. Though there are various models followed in different countries, home-based palliative care is preferred by patients who wish to stay close to their loved ones at their end of life. For providing home-based care, there are certainly important elements that have to be taken care of before planning the implementation because every country has its own healthcare needs, system, and context. India is a developing country where isolated Palliative Care is practiced, hence the situation demands the need of addressing the essential elements that can be included in the protocol of home-based palliative care to enhance the quality of care. Therefore, this study aims to identify a few elements needed to provide home-based palliative care in the Indian context. A rapid review was conducted where seven studies were included that mentioned the elements of home-based palliative care. The electronic databases searched were MedLine, PubMed, and Cochrane databases of systematic reviews. The review was carried out over a period of 8 weeks in June and July 2022. Seven common essential themes were identified; (i) inter-sectoral and inter-professional cooperation, (ii) trust and safety, (iii) holistic management, (iv) non-academic palliative care, (v) spiritual care, (vi) support to caregivers, and (vii) funding and financial support. Our review of effective palliative care models explicates the essential elements for quality home-based care for patients with a terminal illness. The application of the elements must be relevant to the local context due to the huge diversity of the country.
Keywords
Palliative care
Home-based model
Elements
Caregivers
Quality of life
India
INTRODUCTION
The rapid rise in the cases of chronic illnesses is mostly attributed to non-communicable diseases.[1,2] Chronic illness needs long-term care, further requiring a care team and higher cost utilisation for longer hospital stays.[3] To reduce the number of hospital days and provide efficient care by relieving the signs and symptoms of the patient, the home-based palliative care model is effective.[4] Home-based care is not only patient-centred care but also focuses on increasing the patient’s quality of life and giving them painless death.[5] Although many studies have supported the model of home care in terms of patient satisfaction and cost utilisation, there is a need for delineation of the essential elements to effectively process the model.[6]
The community-based approach to delivering home care has meant to improve patient outcomes while reducing the cost of care.[6] Home-based care can be proven effective in terms of providing potent psychosocial care by the carers which is not possible in long-term hospital stays.[7] To provide palliative care at home, it is necessary to address the elements that are essential for the patient and the family members for high-quality care.[8] The addition of appropriate elements in the home-care program will lead to the successful implementation of the same.
A total of 754 articles were identified. Out of which 503 articles were related to models of palliative care. After cleaning the data, seven studies were found to be associated with the essential elements of home-based palliative care. These studies were based on four factors: perspectives of healthcare providers and caregivers, experiences of nurses and general practitioners, strategies for implementing a home-based palliative care program, and funding and financial support, for rapid review and synthesis. Perspectives of the caregivers are equally important as that of the health-care providers to know the unmet needs of the patients reducing the failure rate and increasing patient satisfaction. The review questions for this study are as follows;
What are the essential elements required for providing quality home-based palliative care?
What are the patient’s and caregiver’s needs while receiving palliative care at home?
How can the elements be implemented into the home-care palliative program?
This article aims to bring out the following outcomes concerning the Indian context;
The most effective and essential elements necessary for a home-based model of palliative care
Challenges and experiences faced by the patients/ caregivers and the healthcare providers, respectively
Reference of important and evident strategies for implementing a home-based palliative care intervention.
METHODS
A rapid review is an alternative to systematic reviews which are performed to stabilise the time constraint and possible bias occurrence.[9] The rapid review is preferred here to get an overview of the evidence of the essential elements used for the home-care model. This study was undertaken for 8 weeks from 1 June to 31 July 2022. Although the process of rapid review saves time/resources, it has a scope of generating bias due to the restricted literature coverage. Therefore, the studies were selected carefully by searching various databases such as PubMed, Medline, and Cochrane database of systematic reviews. Although there was no quality check, independent screening of citations and abstracts of the included studies was done by both reviewers. The strategy of study selection is shown below [Figure 1]. The first 4 weeks were utilised for searching and reading the literature available in the databases PubMed and Medline. The next 4 weeks were used to critically analyse the systematic reviews from the Cochrane Library and add them as a reference.
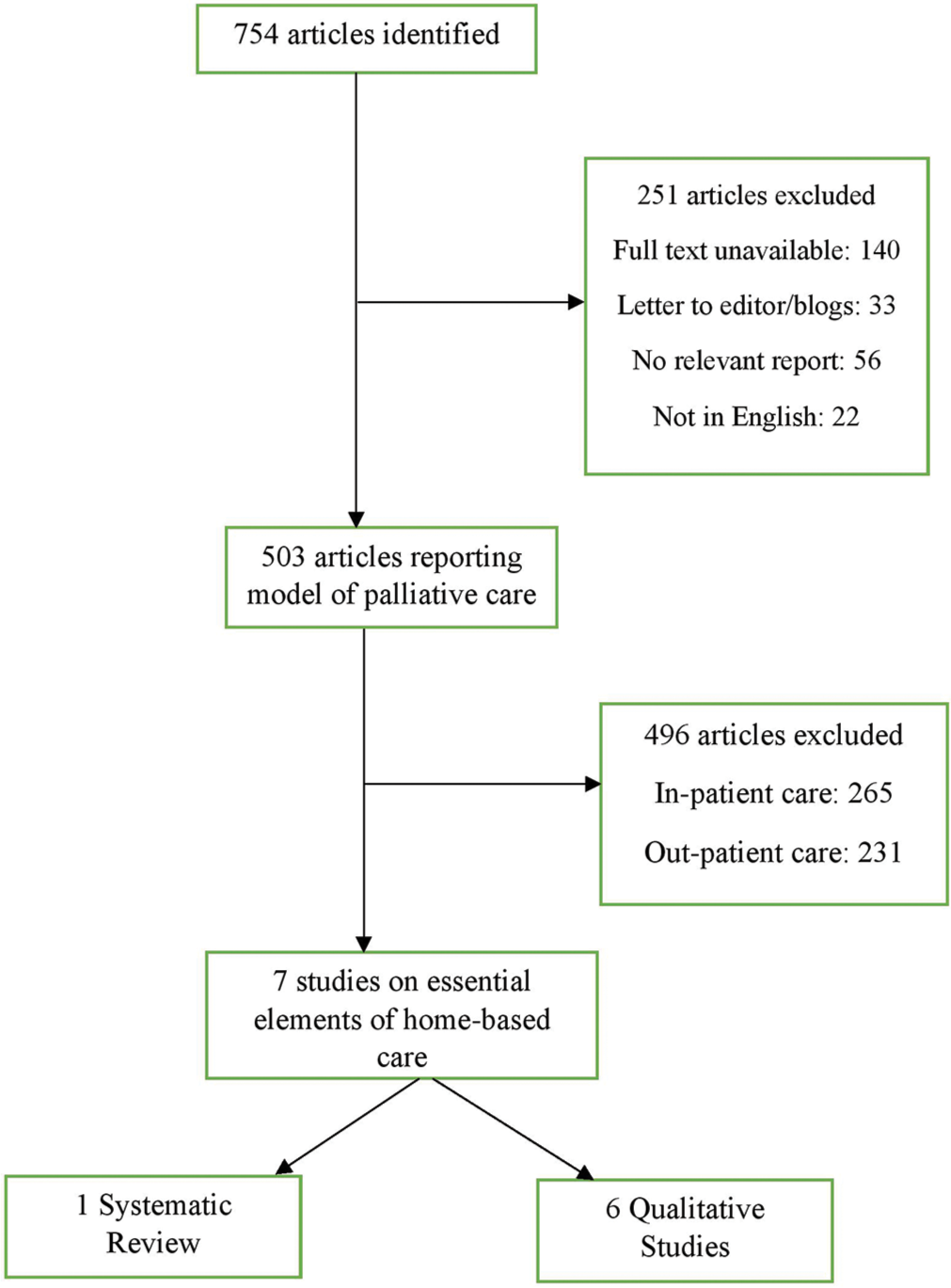
- The strategy for study selection.
Seven studies were selected for the synthesis, after a review of the palliative home-care programs based on the Indian context. The studies selected were a systematic review of the unmet needs of patients; perceptions of healthcare providers about home-based palliative care; a qualitative study on the perspectives of caregivers; a qualitative study on challenges of home-care nurses and physicians; recommended strategies for implementing a home-based palliative care intervention; CanSupport: a model for home-based palliative care delivery in India and Public, patient’s and carer’s views on palliative and end-of-life care in India. A qualitative method using ‘Thematic Synthesis’ developed by Thomas and Harden was used to synthesise the studies and extract common themes out of them, concluding with seven common and essential elements needed for a home-based palliative care program.[10] The analysis was done by the authors and the themes identified were discussed with the palliative care specialists and other research scholars. The summary notes were compared and contrasted to derive some common elements synthesised from the studies. Details of the selected studies for synthesis are discussed below in [Table 1].
| S. No. | Title and author | Type of Study | Methods | Results | Conclusion |
|---|---|---|---|---|---|
| 1. | ‘Home-based palliative care: a systematic review of the self-reported unmet needs of the patients and caregivers’. Ventura et al.[11] |
The systematic review included nine qualitative, three quantitative, and three mixed-design studies. | The study followed PRISMA guidelines. The databases used were PubMed, CINAHL, Embase, MEDLINE, PsycINFO, AMED, and Care Search to identify the unmet needs of the patients and the caregivers | The most important and frequently mentioned needs by the patients and the caregivers were the ineffective and lack of communication with the health-care professionals. | The communication gap had a negative impact during the entire process of home-care intervention. On the other side, the physical needs were mostly met in terms of signs and symptoms relief. |
| 2. | ‘Health-care providers’ perceptions about home-based palliative care in terminally-ill cancer patients.’ Heydari et al.[12] |
The study adopted a qualitative approach using a conventional content analysis carried out in the phase from October 2016 to September 2018 in Iran. | The method involved 18 individual interviews and a focus group discussion with the healthcare providers selected through the process of purposive sampling. The analysis of the data was performed by following the method proposed by Lundman and Graneheim. | From the data analysis, 511 codes were extracted and divided into two major categories of challenges and opportunities which were further divided into ten subcategories. | Some of the most important identified challenges were lack of inter-sectoral and inter-professional cooperation, lack of infrastructure for the care of dying, right time of transferring the patient from the care setting to the home, academic palliative care, and spiritual vacuum. |
| 3. | ‘Barriers to home-based palliative care in people with cancer: a qualitative study of the perspectives of the caregivers’ Hassankhani et al.[13] |
The study was descriptive and carried out in a community-based centre. | Twenty-three caregivers participated in the study where interviews were taken through a semi-structured questionnaire. | Data analysis led to many barriers such as a lack of instructions to the caregivers in terms of clinical practice guidelines, tariffs, and insurance coverage if any. The nurses had limited knowledge due to no provision of specialised training for home-based palliative care. | The caregiver’s and/or the family’s view of prognosis were not taken into consideration to improve the patient’s outcomes which developed many trust issues between the two. |
| 4. | ‘Experiences and challenges of home-care nurses and general practitioners in home-based palliative care: a qualitative study’. Danielsen et al.[14] |
The study was qualitative in nature. | The study involved four focus group discussions with a total of 19 participants, who were either nurses or general practitioners. A semi-structured questionnaire was used for the same. The data was analysed by systematic text condensation and enclosed thematic analysis of the texts and cases. | Three major themes were identified. One was about the good start of the home-care program by developing trust and safety with the patient and family by the healthcare professionals. Second, the prime importance of collaboration between the health sectors including primary care as well. And lastly, complete preparation for the terminal stage of illness together with the bereavement process. | Due to the lack of collaboration, there is a vulnerable gap in transferring patients from the hospitals to their homes. Counselling to the patients and the family members is to be delivered whenever felt necessary. |
| 5. | ‘Barriers, facilitators and recommended strategies for implementing a home-based palliative care intervention in Kolkata, India.’ Qanungo et al.[15] |
The study was qualitative in nature. | The study took in 20 clinical and patient stakeholders for the semi-structured interview. The questions examined the delivery system of palliative care and the barriers and facilitators in Kolkata, India. | The authors found that most of the patients remained unaware of their disease stage and severity. Till the time they access palliative care, it is already late and the disease is at its last stage. Furthermore, there is little or no community engagement in home-care palliative programs. | The strict rules and regulations regarding morphine distribution at home acted as a considerable hurdle for providing pain relief to the patients. |
| 6. | ‘CanSupport: A model for home-based palliative care delivery in India.’ Yeager et al.[16] |
The study was retrospective in nature and aimed to describe the home-based palliative care model provided by CanSupport, an NGO based in Delhi since 1996. | The study included the patients treated by CanSupport in the year 2009–2010. | Most of the patients at their end stage desire to stay at home and get treated. The home-based model reduced the hospital and out-of-pocket expenditures. | The multidisciplinary team helped in symptom management as well as emotional counselling for both patients and families. |
| 7. | ‘Public, patient’s and carer’s views on palliative and end-of-life care in India.’ Venkatasalu et al.[17] |
The study was an integrative review. | The integrative review was done with the help of five databases; MEDLINE, CINAHL, EMBASE, PsychINFO, and Google Scholar for the period 1990–2014. | Five themes were identified. A thematic analysis framework was used to identify and analyse the key themes. | The review suggested the theme of family caregiving during the last days of life as one of the major and important factors responsible for psychosocial impacts. |
RESULTS
Common themes were identified from the seven selected studies for review and synthesis. After performing the thematic synthesis as suggested by Thomas and Harden, the results derived seven common essential elements required for providing quality home-based palliative care [Table 2]. Various codes were identified from the selected studies and combined into descriptive and analytical themes. The common themes are further presented in detail to have a better understanding.
| S. No | Elements | Home-based Palliative care: a systematic literature review of the self-reported unmet needs of the patients and caregivers | Healthcare Providers’ perceptions of Home-based Palliative care in terminally ill cancer patients | Barriers to home-based palliative care in people with cancer: a qualitative study of the perspectives of the caregivers | Experiences and challenges of home-care nurses and general practitioners in home-based palliative care | Barriers, facilitators, and recommended strategies for implementing a home-based palliative care intervention in Kolkata, India | CanSupport: A Model for Home-based Palliative Care in India | Public, patient’s, and carer’s views on palliative and end-of-life care in India |
|---|---|---|---|---|---|---|---|---|
| 1. | Inter-sectoral and Inter-professional Cooperation | Communication between doctors and nurses as well as between primary and secondary staff. Poor coordination of services. |
Coordination to promote the health of the community. Community-based health services. Media and welfare organisations should be involved. |
Siloed care. Lack of high-quality care. Absence of communication between caregiver and physicians. |
Lack of collaboration with hospitals in the transfer of patients. No collaboration of nurses with general practitioners. |
Integration for implementing health-related programs | Local Self-Government Institutions (LSGIs) are the backbone of service delivery facilitation | --- |
| 2. | Trust and safety | --- | The social record of the family should be assessed. Fear of theft/assault. Consider security issues and coordinate with local security officials. |
Distrust in-home-care services. | Primary group for patients and family for safety. Empathy. Time to listen. 24/7 availability |
Regular communication. Good collaboration from the very 1st day |
--- | --- |
| 3. | Holistic management | Psychological needs. Practical needs in transport and outdoor mobility. Respite care. |
Management of death. Transferring patients to their homes. |
--- | Good support from the hospital’s palliative care centre. Mentoring and counselling. Preparing for the terminal stage. |
--- | Team-based approach Coordinated care |
Religion is a major factor in deathbed visions Religious and spiritual practices as a major element in India |
| 4. | Non-academic palliative care | Patients and carers wanted more information about the illness. Information about caregiving role in writing. |
The incompetence of professional health-care providers. Physicians and nurses are not taught in courses and curricula about home-based care. |
Lack of clinical practice guidelines. Did not receive education/training in palliative care. Lack of professionalism. |
Collaboration with other sectors for courses/curriculum | Special course for nurses. Training during graduation |
Educating physicians about palliative care referral | Family-centred palliative care and end-of-life Curricula in Nursing programs |
| 5. | Spiritual care | Inability to attend religious services. To pray and be with friends and family. To be brave. |
No knowledge of spiritual experts. The potential of religious experts is not fully utilised. Peaceful death for patients. |
--- | End-of-life care. Bereavement care. |
--- | Psychological assessment including spiritual, and emotional needs | Some of the major spiritual concerns were faith in God, karma, re-birth, denial and self-acceptance |
| 6. | Support to carers/caregivers | Respite care | --- | --- | --- | Family support system | Caregiver’s satisfaction is measured by delivering the post-bereavement questionnaire by CanSupport after -12 weeks of the patient’s death. | Carer’s leave or Respite care to reduce the burden and to maintain a psychosocial balance in the caregiver. |
| 7. | Funding and Financial Support | Assistance with transport and mobility Access to wheelchairs |
Appropriate infrastructure Lack of Insurance coverage |
Lack of specific tariffs Lack of insurance coverage |
--- | Lack of affordability of medication and treatment costs | Lack of funding and government policies act as a barrier to access early palliative care. | The lack of basic life needs and financial constraints among Indian families |
Inter-sectoral and Inter-professional cooperation
The communication gap was found to be the major drawback in all the observed studies as there was a dearth of coordination between the physicians and the nurses as well as between the caregivers and the healthcare professionals, and therefore, there was a lack of high-quality care as quoted by the caregivers.[11-13] Inter-sectoral coordination between health-care professionals and various institutions including primary care is imperative to promote the health of the community. It was thought to be useful in cases of referring patients for palliative care by the general practitioners/physicians, transferring the patients from the hospitals to their homes, and also providing any healthcare facilities.[14] Maintaining professionalism is of utmost necessity in the field of healthcare to gain patients’ and caregivers’ trust and support. The review identified a communication gap between the palliative care team members which resulted in a poor care plan for the patients.[15] The healthcare providers believed that inter-sectoral coordination is essential for integrated care. However, the caregivers stated that inter-professional cooperation helps improve the quality of life of the patients.[16]
Trust and safety
Building rapport and trust between the patients/caregivers and the health-care team is a vital part of home-care services and one of the ways is listening to them carefully with all your attention.[12] Long-term care plans cannot work smoothly if the patients do not trust their care providers.[13] Furthermore, the round-the-clock availability of health-care providers on the telephone ensures some extra care and comfort for the patients.[14] Safety issues were registered from both sides. On one hand, the caregivers were not prepared enough to accept the palliative care team as they were unaware and new to the concept of home care. Hence, they demanded coordination with local security officials before entering their homes.[15] While, on the other hand, some of the nurses had fear of physical assaults and theft. Hence, they suggested that the social records of the families should be assessed before implementing the care plan.
Holistic management
The home-care plan must include all the aspects of care such as physical, social, psychological, and spiritual.[11] In most cases, only the physical needs are fulfilled in terms of pain relief by giving medications or therapy. The spiritual and psychosocial aspects of care often remain unmet either due to a lack of knowledge or training of the staff. Psychosocial care can be offered by showing empathy toward the family and patient as well as through better communication. Providing emotional support in the end-of-life has been beneficial for both the family members and the patients. Palliative care hospital centres should also provide practical support such as transportation and outdoor mobility.[12,16] Holistic care also involves giving respite care to caregivers. Respite care allows temporary relief to the primary caregivers for a day or a week. This helps in reducing anxiety and stress arising out of continuous care. Many studies have been suggesting to add respite care as one of the components of holistic care. Religion also played a role during the before- and after-bereavement process.[17]
Non-academic palliative care
Palliative care is still an emerging field of study, especially in low-middle-income countries. That being the case, there is a lag in training/practice in academics (UG and PG courses in medical colleges) and clinics/hospitals, respectively.[12] Professional healthcare providers were incompetent, especially physicians and nurses were not familiar with the dimensions of the home-care approach.[13] A special need was recognised for providing training in home-based palliative care for the nurses.[15,17] The studies also recommended introducing curricula related to home-based palliative care in undergraduate medical courses so that the professionals can follow the clinical guidelines without any discrepancy. Like the (National Consensus Project) guidelines encourage to integration of palliative care principles in the routine assessment to provide quality care.[18]
Spiritual care
The patients expressed their sadness when they could not attend the religious services or perform their cultural rituals due to the sickness.[11] The older adults wanted to offer prayers along with their friends and family. The studies noted that only a few home-care models involved a spiritual expert. Even if they are involved, their potential is not utilised fully either due to a lack of training or cooperation.[12] Many of the patients found their peace when performing religious activities of their choice. Hence, the patients should be given freedom and privacy to spend leisure time in their own way which will ultimately lead to the satisfaction of the patients. Spiritual care is also one of the components of bereavement care which is often provided before and after the death of the sick.[14] The spiritual needs are not limited to religious matters. It is a broad spectrum that can differ from person to person ranging from love, attention, hope, forgiveness, grief, etc.[17] Hence, before providing spiritual care, the patient’s individual spiritual needs should be assessed to offer individual healing.
Support to caregiver
Very few studies have mentioned the support and care needed by the caregiver. Most of the time, the caregiver is a woman, mainly a housewife. Emotional disturbances such as anxiety and stress of the caregiver affected the general well-being of the patient as well as the caregiver. Furthermore, no former experience in taking care of patients with palliative care needs is one of the challenges identified by the family caregivers. Support can be provided through telemedicine or mobile apps to the patients and the caregivers to navigate care at home. Another aspect called respite care is a term that means to give temporary relief to the primary caregivers from their duty so that a balance can be restored in their lives.[11,17]
Funding and financial support
Economic self-sufficiency plays a major role in the sustainability of any palliative care model. The financial security of the program depends on the source of funding. For instance, the community-based Kerala palliative care project receives its funding through micro-donations, social entrepreneurship, and regular monthly collections. Likewise, the NGOs and hospices in India are mostly run by the private sector.[15] Sufficient funds must be released from the flexi pool to develop infrastructure and avail medications for the state.[16] Many low- and middle-income families sometimes could not bear the basic expenses of receiving home-based palliative care.[17] Hence, the financial needs must be assessed before transferring the patient from the hospice to the home-care setting.
DISCUSSION
The review has identified some of the major drawbacks of the home-care palliative model such as the communication gap, trust and safety issues, incompetent health-care professionals, devoid of professional courses and clinical guidelines, and an atomistic approach. Although these common elements are very true in a sense, as it is always situated in the local context applicable.[19] In a country like India where palliative care is at its developing stage, it needs strong advocacy at the population and the health-care level.[20] Therefore, palliative care must be included in the courses and curricula of the medical and paramedical students too. As the concept is new, it may take time to build confidence and trust among the beneficiaries at the beginning. Although the most effective way to gain trust is to listen carefully to the patients, varying from person to person. Some patients believe to participate in the treatment decision-making while some prefer to delegate the decision-making role,[21] while some of them may ask for private time during the treatment which has to be respected in any way.[22]
Total pain management is a concept consisting of four dimensions, that is, physical, psychological, social, and spiritual care.[23] No dimension can be treated in isolation.[24] Physical pain is managed by giving pain-relieving drugs such as opioids or physical therapy, which could be further hindered by the lack or unavailability of opioids in the health centers.[25] According to the Narcotic and Psychotropic Substances Act of 1985, opioid availability is very much restricted to prevent its misuse. Only a few cancer hospitals are exempted from the licensing procedure; otherwise, it is mandatory to hold a license to avail of an opioid that is morphine.[26] Psychological care often deals with alleviating the levels of anxiety, stress, depression, and mood swings related to the sickness or in general. The social aspect of care becomes functional when the patient’s social role in the family and society declines or gets replaced. The social network may become infirm due to the stigma of the disease.[27] Spirituality is usually confused with religion. However, religion is one of the components of the broad term spirituality.[28]
Apart from all the aspects of care, there is respite care which is considered to be critically important for the caregivers, patients, and the healthcare system. In a recent study, it was noticed that providing respite care enhanced patients’ self-esteem, improved the quality of life for the caregivers, and reduced hospital admission rates.[29] There are certain limitations to the study. The literature search was limited to some selected studies that mentioned the needs of the palliative care program from the caregivers’ and health-care providers’ perspectives. There were very few studies found in the Indian context so the international models were also considered for the review. However, the themes were found to correspond with the Indian studies as well.[30]
IMPLICATIONS FOR POLICY AND PRACTICE
Support for family caregivers should be the priority concern of the policymakers. Navigating the care plan through telemedicine and telephonic calls by healthcare professionals will keep the carers updated about the patient’s condition. The navigators also make the carer confident and provide emotional support during situations like pain management.[31] Given the resource constraints, it is recommended to focus on the primary family carers (identified by the patient) and wherever possible, include the other family members in providing psychosocial and bereavement care.[32] To ensure quality and coordinated care, a social and healthcare policy should be developed incorporating guidelines for healthcare professionals.
CONCLUSION
The review of the selected literature studies found seven essential elements required for an effective home-based palliative care program, considering the local context. They are as follows; (a) inter-sectoral and inter-professional cooperation; (b) trust and safety; (c) holistic management of death; (d) non-academic palliative care; (e) spiritual care; (f) support to caregivers; and (g) funding and financial support. The common elements identified in this review also correspond with other international studies.[33,34] The observed elements are believed to be needed during the implementation of any home-based palliative care model.[35] A successful palliative care model in developing countries like India will prove a model of trust, safety, and high-end quality care for the patients and their family members. At the same time, it is important to strengthen the knowledge of palliative care among healthcare providers and the end-users through various platforms such as institutions, clinics, NGOs, and media.[36]
Acknowledgement
I thank Dr. Katta Ajitha, Associate Professor, and my supervisor for providing her valuable comments and suggestions for writing the manuscript.
Declaration of patient consent
Patient consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Junior Research Fellowship (JRF) by UGC-NET.
References
- A Review on Noncommunicable Diseases (NCDs) Burden, its Socio-economic Impact and the Strategies for Prevention and Control of NCDs in India. Indian J Public Health. 2018;62:302-4.
- [CrossRef] [PubMed] [Google Scholar]
- Physical Activity and the Prevention of Chronic Illness in the BRICS Nations: Issues Relating to Gender Equality. J Sport Health Sci. 2019;8:507-8.
- [CrossRef] [PubMed] [Google Scholar]
- The Effects of Multiple Chronic Conditions on Hospitalization Costs and Utilization for Ambulatory Care Sensitive Conditions in the United States: A Nationally Representative Cross-sectional Study. BMC Health Serv Res. 2016;16:77.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Home-based Palliative Care on Health Care Costs and Hospital Use: A Systematic Review. Palliat Support Care. 2021;19:474-87.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care in India: Current Progress and Future Needs. Indian J Palliat Care. 2012;18:149-54.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of a Home-based Palliative Care Program on Healthcare Use and Costs. J Am Geriatr Soc. 2016;64:2288-95.
- [CrossRef] [PubMed] [Google Scholar]
- Home Based Palliative Care: Known Benefits and Future Directions. Curr Geriatr Rep. 2021;10:141-7.
- [CrossRef] [PubMed] [Google Scholar]
- What are the Essential Elements of High-quality Palliative Care at Home? An Interview Study Among Patients and Relatives Faced with Advanced Cancer. BMC Palliat Care. 2019;18:96.
- [CrossRef] [PubMed] [Google Scholar]
- Rapid Reviews Methods Series: Guidance on Literature Search. BMJ Evid Based Med 2023:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Methods for the Thematic Synthesis of Qualitative Research in Systematic Reviews. BMC Med Res Methodol. 2008;8:45.
- [CrossRef] [PubMed] [Google Scholar]
- Home-based Palliative Care: A Systematic Literature Review of the Self-reported Unmet Needs of Patients and Carers. Palliat Med. 2014;28:391-402.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring Health Care Providers' Perceptions about Home-based Palliative Care in Terminally Ill Cancer Patients. BMC Palliat Care. 2019;18:66.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to Home-based Palliative Care in People with Cancer: A Qualitative Study of the Perspective of Caregivers. Nurs Open. 2020;7:1260-8.
- [CrossRef] [PubMed] [Google Scholar]
- Experiences and Challenges of Home Care Nurses and General Practitioners in Home-based Palliative Care-a Qualitative Study. BMC Palliat Care. 2018;17:95.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers, Facilitators, and Recommended Strategies for Implementing a Home-based Palliative Care Intervention in Kolkata, India. Am J Hosp Palliat Care. 2021;38:572-82.
- [CrossRef] [PubMed] [Google Scholar]
- CanSupport: A Model for Home-based Palliative Care Delivery in India. Ann Palliat Med. 2016;5:166-71.
- [CrossRef] [PubMed] [Google Scholar]
- Public, Patient and Carers' Views on Palliative and End-of-life Care in India. Int Nurs Rev. 2018;65:292-301.
- [CrossRef] [PubMed] [Google Scholar]
- National Consensus Project Clinical Practice Guidelines for Quality Palliative Care Guidelines, 4th Edition. In: J Palliat Med. Vol 21. 2018. p. :1684-9.
- [CrossRef] [PubMed] [Google Scholar]
- Specialist Palliative Care: Patients' Experiences. J Adv Nurs. 2003;44:24-33.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care Advocacy: Why does it Matter? J Palliat Med. 2020;23:1009-12.
- [CrossRef] [PubMed] [Google Scholar]
- Shared Decision-making in Palliative Care: A Systematic Mixed Studies Review Using Narrative Synthesis. Palliat Med. 2011;25:242-61.
- [CrossRef] [PubMed] [Google Scholar]
- Dignity of Patients with Palliative Needs in the Middle East: An Integrative Review. BMC Palliat Care. 2021;20:112.
- [CrossRef] [PubMed] [Google Scholar]
- The Concept of Total Pain: A Focused Patient Care Study. Br J Nurs. 2001;10:1248-55.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care Integration for Patients with Advanced Chronic Obstructive Pulmonary Disease (COPD): Identifying Essential Components Using Participatory Action Research. Palliat Med. 2021;35:1933-40.
- [CrossRef] [PubMed] [Google Scholar]
- Improving Access to Opioid Analgesics for Palliative Care in India. J Pain Symptom Manage. 2002;24:152-9.
- [CrossRef] [PubMed] [Google Scholar]
- Medical Use, Misuse, and Diversion of Opioids in India. Lancet. 2001;358:139-43.
- [CrossRef] [PubMed] [Google Scholar]
- Creating Social Work Competencies for Practice in Hospice Palliative Care. Palliat Med. 2010;24:79-87.
- [CrossRef] [PubMed] [Google Scholar]
- Spiritual Care at the End of Life in the Primary Care Setting: Experiences from Spiritual Caregivers-a Mixed Methods Study. BMC Palliat Care. 2019;18:98.
- [CrossRef] [PubMed] [Google Scholar]
- The Concept of Respite in Palliative Care: Definitions and Discussions. Curr Oncol Rep. 2021;23:25.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care in India: Situation Assessment and Future Scope. Indian J Cancer. 2015;52:99-101.
- [CrossRef] [PubMed] [Google Scholar]
- 'My Wife is My Doctor at Home': A Qualitative Study Exploring the Challenges of Home-based Palliative Care in a Resource-poor Setting. Palliat Med. 2021;35:97-108.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for the Psychosocial and Bereavement Support of Family Caregivers of Palliative Care Patients. J Palliat Med. 2012;15:696-702.
- [CrossRef] [PubMed] [Google Scholar]
- The Impact of a Home-based Palliative Care Program in an Accountable Care Organization. J Palliat Med. 2017;20:23-8.
- [CrossRef] [PubMed] [Google Scholar]
- A Review of the Essential Components of Quality Palliative Care in the Home. J Palliat Med. 2018;21:S37-44.
- [CrossRef] [PubMed] [Google Scholar]
- "Small Small Interventions, Big Big Roles" a Qualitative Study of Patient, Caregiver and healthcare worker Experiences of a Palliative Care Programme in Kerala, India. BMC Palliat Care. 2019;18:16.
- [CrossRef] [PubMed] [Google Scholar]
- Developing a Service Model that Integrates Palliative Care Throughout Cancer Care: The Time is Now. J Clin Oncol. 2014;32:3330-6.
- [CrossRef] [PubMed] [Google Scholar]






