Translate this page into:
Forecasting Patients' Lifespan
Address for correspondence: Dr. Md Rabiul Alam, Department of Anaesthesiology, Combined Military Hospital, Dhaka 1206, Bangladesh. E-mail: rabiuldr@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Prognostication is sensitive and always uncomfortable for the doctors. Doctors often get involved in it by encountering somewhat pressures, obligations, and critical queries from the agonized patients and their relatives in stress. Instead, they are neither trained properly in prognosticating by a formal curriculum nor having any unanimous determining tool.[1] Yet, forecasting affects the quality of end-of-life care.
Most of the patients suffering from chronic and incurable diseases yearn for their prognosis. In a large-scale study, 71% of terminally ill cancer patients desired to know how long they had left to live.[2] Despite this preference, only 18% reported that their physicians provided them with a prognostic estimate.
There is a wide controversy on the accuracy of prognostication. In another study, 74% of patients recalled that their life expectancy estimations were accurate to within a year.[3] Studies of prognostic accuracy in palliative care are found to be heterogeneous and are frequently inaccurate.[4] The prognosis of patients of a hospice was overestimated in 88% of cases.[5]
In contrast, doctors are inaccurate in prognosis and the error is systematically optimistic. A cohort study showed that only 20% of predictions were accurate: 63% were overoptimistic and 17% were overpessimistic. The greater the experience of the doctor, the greater the prognostic accuracy, but interestingly, a stronger doctor–patient relationship is associated with lower prognostic accuracy.[6]
Besides, researchers are constantly striving to be accurate in prognostication. A score based on 14 metabolic biomarkers and sex leads to improved risk prediction as compared to the conventional risk factors.[7]
Instead of usefulness, prognostication has detrimental effects on the patients' psyche. It has risks, especially at the level of the individual. Individuals who have an illness are often dissuaded from pursuing personal goals that may exceed perceived limitations caused by the illness. Seeking educational, vocational, or independent-living goals beyond one's expected capabilities may lead to failure and relapse.[8]
Foretelling is prohibited in most of the beliefs. But, religions do not utterly defy the phenomenon of prognostication, particularly in the case of moribund patients. There are comprehensive recommendations for dealing with patients who are in end-of-life care.
The caregivers and the doctor who is treating should raise patient's hopes of recovery and give him/her the impression that his/her illness is not something to worry about and cheer him/her up by telling him/her that he/she will get better and be healthy and live a long life.[910] Patients' psychological state helps with recovery and healing from sickness. The stronger the patient's morale, the more likely and speedy his/her recovery will be.
Telling the patient about the real nature of his/her sickness and that this sickness may lead to his/her death is a matter that is subject to further clarification. If this will not make him/her feel worse, then the basic principle is that it is permissible to tell him/her, while also reminding that it is possible to recover. Hence, for example, it may be said: some people were affected by this disease and recovered from it by the grace of our Creator and other such words that will give the patient the hope of healing. But, if telling will make him/her feel worse, then it is better not to tell.
This varies from one patient to another. Some patients are of strong character and do not care if the sickness is fatal or not. In this case, he/she must be told the truth because the patient may have certain relationships with his/her family or other people in which some problems need to be corrected. Hence, in this case, he/she must be told, and there will be no harm in that.
However, if the patient is of weak character and there is the fear that if he/she is told the truth that this is a fatal disease, he/she will be more adversely affected and will only focus on this sickness, and it is known that if the patient focuses on his/her sickness and that becomes his/her main concern, this exacerbates the sickness, but if he/she ignores it or tries to forget it and starts behaving as if there is nothing wrong with him/her, then this is one of the best means of recovery.
“No person knows what he will earn tomorrow, and no person knows in what land he will die. Verily, Allah is All-Knower, All-Aware (of things).”[11]
Saying that someone will die on such and such a day for certain is not permissible and comes under the heading of claiming to know the unseen.
However, if someone says that so and so may die after a certain amount of time, or after a few days, based on his/her condition and sickness, and by the way of expectation only, there is nothing wrong with this. But, it should not be spread widely or said to the patient or his/her family because this may affect the patient's psychology or make his/her sickness worse, and it may also affect the psychology of his/her relatives. So, such matters should be concealed, and the patient and his/her family should be given the hope that he/she may recover by the mercy of God, meaning, this is not a false hope.
Prognostic information is important for patients, caregivers, and clinicians. For patients, it allows time to prepare for approaching death, for example, by making financial plans or saying goodbye. For clinicians, awareness and consideration of prognosis may be important for informing decision-making surrounding medical interventions, achieving a preferred place of care, and advance care planning.[12] Open discussion about prognosis can facilitate patient-centered care and shared decision-making. Moreover, this process is not a constant, it requires reevaluation. An infographical cycle [Figure 1] for prognostication is proposed here for quick and better understanding by the counselors. Religious faiths and social cultures may be needed to incorporate the phenomenon of prognostication to achieve better outcomes.
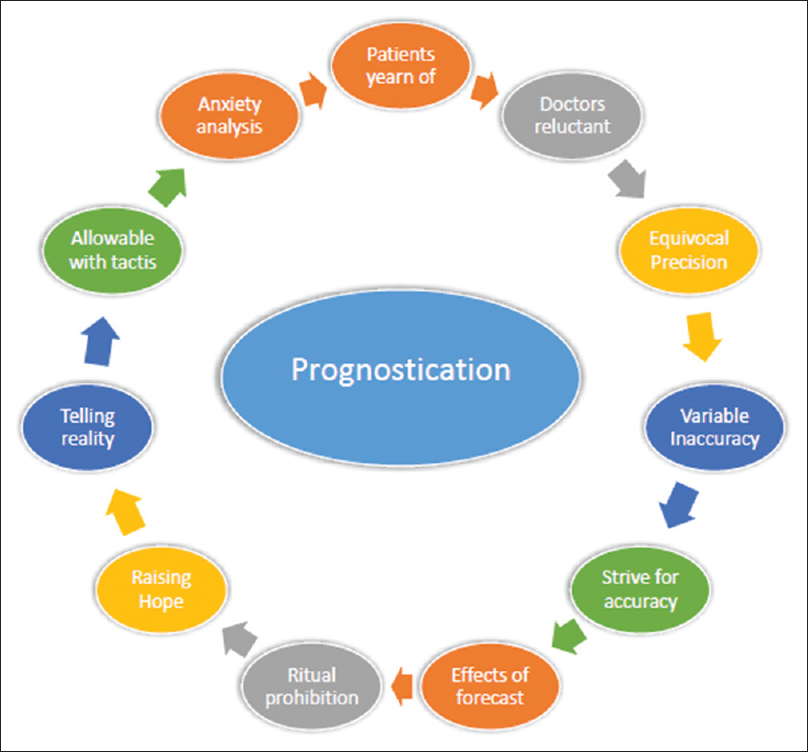
- The proposed cycle of prognostication
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Outcomes of prognostic disclosure: Associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol. 2015;33:3809-16.
- [Google Scholar]
- Accuracy of oncologists' life-expectancy estimates recalled by their advanced cancer patients: Correlates and outcomes. J Palliat Med. 2016;19:1296-303.
- [Google Scholar]
- A systematic review of predictions of survival in palliative care: How accurate are clinicians and who are the experts? PLoS One. 2016;11:e0161407.
- [Google Scholar]
- Can doctors accurately predict the life expectancy of patients with terminal cancer? Palliat Med. 1987;1:165-6.
- [Google Scholar]
- Extent and determinants of error in doctors' prognoses in terminally ill patients: Prospective cohort study. BMJ. 2000;320:469-72.
- [Google Scholar]
- A metabolic profile of all-cause mortality risk identified in an observational study of 44,168 individuals. Nat Commun. 2019;10:3346.
- [Google Scholar]
- Ruling on Informing a Patient that he will die Soon. Available from: https://islamqainfo/en/answers/188991/
- Dar-us-Salam Hadith 3936. Available from: https://quranxcom/Hadith/Bukhari/DarusSalam/Hadith-5354
- The Quran. Available from: http://tanzilnet/#trans/ensahih/31:34





