Translate this page into:
Herth Hope Index: A Psychometric Evaluation Study within a Sample of Greek Patients with Cancer
*Corresponding author: Mystakidou Kyriaki, Department of Radiology, Pain Relief and Palliative Care Unit, Areteion Hospital, School of Medicine, Athens, Greece. mistakidou@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Nikoloudi M, Tsilika E, Parpa E, Kostopoulou S, Tentolouris A, Psarros C, et al. Herth Hope Index: A Psychometric Evaluation Study within a Sample of Greek Patients with Cancer. Indian J Palliat Care 2021;27:367-74.
Abstract
Objectives:
This study aims to develop the Greek version of the Herth Hope Index (HHI) and assess its psychometric properties to a palliative care patient sample, using a cross-sectional design.
Materials and Methods:
The HHI was translated into Greek (HHI-Gr) using the ‘forward-backward’ procedure. It was administered to 130 eligible cancer patients, while for the stability of patients’ responses, 40 of these patients completed the HHI-Gr 3 days later. Along with the HHI-Gr, patients also completed the Hospital Anxiety and Depression Scale (HADS) and the Beck Hopelessness Scale (BHS). The HHI-Gr internal consistency reliability (Cronbach’s a), stability (intraclass correlation coefficient [ICC]), factor structure (factor analysis) and convergent validity (correlation with the HADS and the BHS questionnaires) were examined using the Eastern Cooperative Oncology Group (ECOG) performance status.
Results:
The HHI-Gr yielded a one-factor model and a Cronbach alpha (0.860) with excellent internal consistency reliability and stability ICC (>0.90). Satisfactory convergent validity was supported by the correlation analysis between the HHI-Gr and BHS (r = 0.718, P < 0.001). Overall test-retest reliability was satisfactory with a range between 0.77 and 0.96 (P < 0.001).
Conclusion:
These results demonstrate that the HHI-Gr is an instrument with satisfactory psychometric properties and is a valid research tool for the measurement of the levels of hope among Greek oncology patients.
Keywords
Palliative care
Cancer
Hope
Depression
Anxiety
INTRODUCTION
Hope has been positively correlated with health overtime. Hope’s qualities such as cognitive-emotional, indented-impulsive and individual-social have been described in clinical practice and in theory due to its high importance among patients.[1-3] Hope is defined as ‘the multidimensional, dynamic and empowering state of being at the centre of life, related to external help and care, oriented toward the future and personalised to each individual.’[4,5] Although hopelessness is strongly associated with increased levels of stress and depression, as a multidimensional concept, hope represents more than the loss of relevant clinical symptoms of anxiety and/or depression.[6] Hope is especially important for people’s mental well-being, as it acts as a protective mechanism against stress and disease, and as a pre-requisite for effective response to treatment.[7] It also has a positive effect on some psychological distressing symptoms, such as depression, stress and exhaustion, and appears to have a long-term effect on people’s well-being.[8-10] People with higher levels of hope, often, are less isolated, they have more positive interpersonal relationships, while there is a relationship between hope with other psychological parameters, such as self-esteem and life satisfaction.[7,11,12]
Health professionals often face difficulties in communicating unpleasant diagnostic and/or prognostic issues experience a moral dilemma; whether to maintain hope by disclosing some information or divulge the whole truth respecting patients’ autonomy but with the risk of losing hope. This perspective is directly related to various theories of ethics, where health professionals experience serious task conflicts.[13-15]
For the oncology patient, hope is a prerequisite for effectively treating the disease and symptoms, better tolerating pain and making the appropriate decisions. Hope protects against physical, mental and social burden from the disease, while it is the act by which the tendency toward despair is ‘controlled;’ therefore, it may affect adaptation to the disease and contribute to the deterioration of the well-being.[16-18] As an inner force, hope is perceived as an available source of life in the present and as a central aspect of the dignified end of a person’s life.[18] At the same time, hope plays a very important role in the management of disease and loss, while the loss of hope can create a submissive response.[7]
The feeling of hope is a promotional act of cognitive processing that is directly related to success. It has been found that hope improves the treatment of the disease, psychological adjustment and quality of life. The essential role of hope is also present in advanced cancer stages.[18,19] In this context, the concept of hope plays a central role in their lives. Hope is the primary reason why patients make the decision to follow a particular treatment or operation from the beginning.[20]
The assessment of hope and its qualities are difficult; however to date, a variety of hope scales have been developed and used. The most commonly used tools are the Herth Hope Scale, and its short form, the Herth Hope Index (HHI).[7,21-23] The HHI was developed by Herth, it has been translated and validated in various cultures, and their psychometric properties have been reevaluated by many researchers.[4,16,23] Nevertheless, it has not been translated and validated to Greek. Therefore, the purpose of this study was to examine the psychometric properties of the translated Greek version of the HHI in palliative care cancer patients.
MATERIALS AND METHODS
This is a cross-sectional study, performed at the outpatient clinic of a pain relief and palliative care unit in Athens, Greece. The unit is approached by cancer patients from all over the country. The HHI-Gr was administered to 130 eligible cancer patients who visited the unit for symptom management; for the stability of patients’ responses, 40 of these patients completed the HHI-Gr 3 days later. The study was performed from August 2018 to April 2019. The hospital’s ethics committee approved the study protocol, all participant patients provided written informed consent, and was in accordance with the guidelines of Good Clinical Practice. The inclusion criteria were as follows: Histologically confirmed malignancy, age >18 years, ability to communicate effectively with the health-care professionals and provision of informed consent. Criteria for exclusion were history of drug abuse, knowledge of the disease diagnosis and significant cognitive impairment (MoCA≤26 and MMSE≤24).[24,25]
Researchers recorded data on patients’ demographic characteristics, disease status, treatment regimen (surgery, chemotherapy, radiotherapy and opioids) and performance status as defined by the Eastern Cooperative Oncology Group (ECOG; 0 = optimum performance status and 4 = worse performance status). Patients with an ECOG score 0 or 1 were categorised as having ‘good’ performance status and those with score 2 or 3 as ‘moderate to poor’ performance status.[26]
The study design included administration of the Greek version of the HHI (HHI-Gr), the Greek version of the Hospital Anxiety and Depression Scale (HADS) and the Beck Hopelessness Scale (BHS), translated and validated in the Greek language.[27,28]
Translation
The forward-backward procedure was applied to translate the HHI from English to Greek. Two individuals translated the original English version into Greek (step 1), and another two individuals translated the results of step 1 back into English (step 2). The main researcher completed the final step (step 3) of the translation process by comparing and matching the original with the English version from step 2.
Instruments
HADSs have been used as a screening tool for the assessment of anxiety and depression symptomatology. HADS is a self-assessment mood scale specifically designed for use in hospital departments.[29] The two HADS subscales, HADS-A (anxiety) and HADS-D (depression), include seven items, on a 4-point scale (0: no problems–3: maximum distress).[30] The authors of the original study suggested the following cutoff scores: 0–7: Non-cases, 8–10: Doubtful cases for both anxiety and depression (with possible ranges of 0–21 for each subscale) and ≥11: Cases. Many investigators have interpreted HADS as a bidimensional instrument, assessing anxiety and depression independently.[30,31] The Greek version of HADS has been translated and validated in a sample of patients with cancer in advanced stages.[28]
Hopelessness was assessed with the BHS, translated and validated in the Greek language (G-BHS).[27,32] The patient self-report scales included BHS.[32] It is a 20-item self-report inventory that was designed to tap a general tendency toward pessimism and negative expectancies.[32] Based on the original cutoff scores, the subjects were classified into four groups: No hopelessness at all (0–3); mild (4–8); moderate (9–14) and severe (15–20).[33] Beck et al. (1974) suggested three factors: ‘Affective,’ ‘motivational’ and ‘cognitive’ factors.
The approval of the study was conducted by the hospital’s ethics committee and according to the Declaration of Helsinki Principles. The study followed the guidelines for Good Clinical Practice.
Statistical analysis
Descriptive statistics were analysed and presented in the study (means, counts and percentages). To assess the reliability of the questionnaire, the internal consistency (Cronbach’s alpha coefficient) and intraclass correlation coefficient (ICC) were also calculated. Principal component analysis (PCA) with varimax rotation was used to validate the HHI-Gr factor structure. Confirmatory factor analysis (CFA) was used to examine the factor structure of the questionnaire to confirm the structure revealed from the exploratory factor analysis. Convergent validity of the HHI-Gr was determined by establishing its correlation to BHS and HADS scales using the Spearman’s correlation coefficient. Known groups validity of the HHI-Gr questionnaire was examined in terms of the ability of questionnaire to distinguish between subgroups of patients formed on the basis of their functional status according to ECOG performance status. Independent samples t-test was used for the statistical analysis. Item analysis of the HHI-Gr questionnaire was performed by analysing the item discriminating power and the item difficulty (item mean) depicted by the explanatory data analysis. A receiver operating curve analysis was conducted to obtain the cutoff level of the HHI-Gr total score for differentiation between subgroups of patients formed on the basis of their expectation of positive outcomes according to the BHS, calculating the respective areas under the curve (AUC). The AUC with standard error and 95% confidence interval (CI) was calculated using the maximum likelihood estimation method, and the sensitivity and specificity of different cutoff points of the HHI-Gr total score were estimated using the BHS score (minimal or mild hopelessness [0–8] vs. moderate or severe hopelessness [9–20] as estimated variable). The intraclass (stability) was determined by calculating ICC between the initial assessment of the HHI-Gr and the reassessment after 3 days. All tests were two sided, P < 0.05 was used to denote statistical significance. All analyses were carried out using the statistical package SPSS version 21.00 (IBM Corporation, Somers, NY, USA).
RESULTS
Descriptive
Of the 130 patients, 53.1% were female; the majority were high school graduates and married (65.4%). Gastrointestinal and lung cancer were diagnosed in 24.4% followed by urogenital cancer (23.2%). Most patients (80.5%) had a poor performance status, 42.7% had undergone chemotherapy and 51.2% were already receiving strong opioids [Table 1].
| Total, n(%) | |
|---|---|
| Gender | |
| Male | 61 (46.9%) |
| Female | 69 (53.1%) |
| Family status | |
| Married | 85 (65.4%) |
| Unmarried | 45 (34.6%) |
| Education | |
| Primary | 27 (20.8%) |
| High school | 72 (55.4%) |
| University | 31 (23.8%) |
| ECOG | |
| 0–1 | 75(57.7%) |
| 2–3 | 55 (42.3%) |
| Chemotherapy | |
| No | 46 (35.4%) |
| Yes | 84 (64.6%) |
| Radiotherapy | |
| No | 41 (31.5%) |
| Yes | 89 (68.5%) |
| Surgery | |
| No | 53 (40.8%) |
| Yes | 77 (59.2%) |
| Age, Mean±SD (min–max) | 70.0±12.0 (29–90) |
SD: Standard deviation
Factor analyses
The factor structure (i.e. three factors) of the original HHI was assessed by CFA giving unacceptable global fit indices. The resulting global fit indices χ2 = 314.3, Chi-square degrees of freedom (df) ratio= 5.82, root mean square error of approximation (RMSEA) = 0.193, comparative fit index (CFI) = 0.461, normed fit index (NFI) = 0.427, goodness of fit index (GFI) =0.744 and adjusted goodness of fit index (AGFI) = 0.630 showed that the three-factor solution proposed by the author should be rejected. The Kaiser-Meyer-Olkin measure of sampling adequacy was equal to 0.882 showing suitable data for factor analysis. The hypothesis of no intercorrelation of items was rejected by Bartlett’s test of sphericity (χ2 = 528.3, df = 66, P <0.001). The 12 items were analysed via maximum likelihood extraction method using a Varimax rotation. Three factors, with eigenvalue of over 1 and items factor loadings were ≧0≥40, were identified. The eigenvalue for factor 1 was 4.98, explaining 41.5% of the variance, the eigenvalue for factor 2 was 1.12, explaining 9.6% of the variance and the eigenvalue for the third factor was 1.01, explaining 8.4% of the variance. Factor loadings ranged from 0.442 to 0.668 for the Factor 1, from 0.453 to 0.638 for the Factor 2 and from 0.501 to 0.644 for the Factor 3 [Tables 2 and 3].
| Items | Eigenvalues | % of variance | Cumulative % |
|---|---|---|---|
| 1 | 4.98 | 41.50 | 4.50 |
| 2 | 1.12 | 9.62 | 51.12 |
| 3 | 1.01 | 8.41 | 59.53 |
| 4 | 0.83 | 6.92 | 66.45 |
| 5 | 0.73 | 6.04 | 72.49 |
| 6 | 0.64 | 5.34 | 77.83 |
| 7 | 0.54 | 4.50 | 82.33 |
| 8 | 0.52 | 4.36 | 86.70 |
| 9 | 0.51 | 4.21 | 90.91 |
| 10 | 0.45 | 3.77 | 94.67 |
| 11 | 0.38 | 3.19 | 97.86 |
| 12 | 0.26 | 2.14 | 100.00 |
| Factor 1 | Factor 2 | Factor 2 | |
|---|---|---|---|
| ITEM10 | 0.668 | ||
| ITEM9 | 0.506 | ||
| ITEM4 | 0.494 | ||
| ITEM6 | 0.490 | ||
| ITEM7 | 0.442 | ||
| ITEM12 | 0.638 | 0.486 | |
| ITEM11 | 0.574 | ||
| ITEM8 | 0.507 | ||
| ITEM5 | 0.453 | ||
| ITEM3 | 0.644 | ||
| ITEM2 | 0.610 | ||
| ITEM1 | 0.464 | 0.501 |
Extraction method: Principal axis factoring, rotation: Varimax, only loadings with values >0.4 are presented.
A three-factor model of HHI-Gr, based on exploratory factor analysis, was examined by CFA giving acceptable global fit indices. The resulting global fit indices χ2 = 70.42, Chi-square-df ratio = 1.38 RMSEA = 0.054, CFI = 0.960, NFI = 0.882, GFI =0.919 and AGFI = 0.876 showed that the new three-factor solution proposed by the exploratory factor analysis could be retained. Although the fit indices of CFA for the three-factor model were good the scree test, Monte Carlo PCA for parallel analysis (the criterion value was 1.54, higher than eigenvalue of the second factor) and the eigenvalues of 2nd and 3rd factor of the model which were marginally accepted (1.12 and 1.01) indicated a single-factor structure. Moreover, the observed three factors are difficult to interpret. They have at least two items in common with the factors of the HHI but neither are the factor denominations by HHI satisfactory for the new factors nor did we achieve to find new suitable and distinct factor descriptions for the new factors. In agreement with Ripamonti et al. (2012) and Geiser et al. (2015), a single-factor model was adopted. The resulting global fit indices χ2 = 89.16, Chi-square-df ratio= 1.65 RMSEA = 0.065, CFI = 0.927, NFI = 0.838, GFI =0.900 and AGFI = 0.850 confirmed the single-factor solution [Figure 1].

- Confirmatory factor analysis of hope single-factor Greek model.
Reliability
Internal consistency
The internal consistency of the HHI-Gr total score was measured with Cronbach’s alpha and estimated as 0.860 which indicate excellent internal consistency for total score and sufficient reliability for the subscales.
Test-retest reliability
The paired samples t-test between initial assessment and reassessment of HHI-Gr subscales and total score indicated no statistically significant difference. The ICC between initial assessment and reassessment of the HHI-Gr total score was 0.902 (P < 0.001), respectively. Bland-Altman plot for total score, inspection of scatter gram showed that all differences were within mean difference ±2 SDs, thus confirming the agreement between two assessments [Figure 2].

- Bland-Altman plot of hope total score mean difference: 0.75 (95% CI −3.4–4.8).
The above results of stability indicated that HOPE total score was remarkably consistent between the two occasions.
Convergent validity
The correlation between the HHI-Gr total score and BHS was high (r = −0.718, P < 0.001), hence satisfying the convergent validity.
Known-groups validity
The HHI-Gr total score well discriminated between subgroups of patients on the basis of their different functional status according to ECOG performance status. HHI-Gr’s total score was higher for patients with ECOG score (1–2) compared to ECOG 3–4 (P < 0.001). The above results of stability indicated that HHI-Gr total score was higher for patients with ECOG score (1–2) compared to ECOG 3–4 (P < 0.001).
Item analysis
The item analysis of the HHI-Gr showed that item 1 had the highest corrected item correlation (0.678), whereas item 5 had the lowest corrected item correlation (0.265). In addition, item 6 had the lowest item mean (2.51), and item 9 had the highest item mean (3.42).
Interpretability floor or ceiling effects
The percentage of patients scoring at the lowest possible level of the scale and at the highest possible level was for the HHIGr total score (0.8% and 3.1%). The critical value of 15% was not surpassed so there were neither ceiling nor floor effect for HOPE questionnaire; the minimum inhibitory concentration was for total score 3.
Measurement error
The error associated with the HHI-Gr total score at a given point in time standard error of the mean was 1.9. The corresponding minimal detectable change value was 5.3.
The cutoff points of HHI-Gr total score
The AUC of HHI-Gr total was 0.900 (95% CI 0.84–0.96 P < 0.001) with cutoff point 34.5, sensitivity 78% and specificity 87%. Patients with HHI-Gr total score <34.5 have 78% probability to have moderate or severe hopelessness, while patients with HHI-Gr total score more than 34.5 have 87% probability to have to minimal or mild hopelessness [Figure 3].
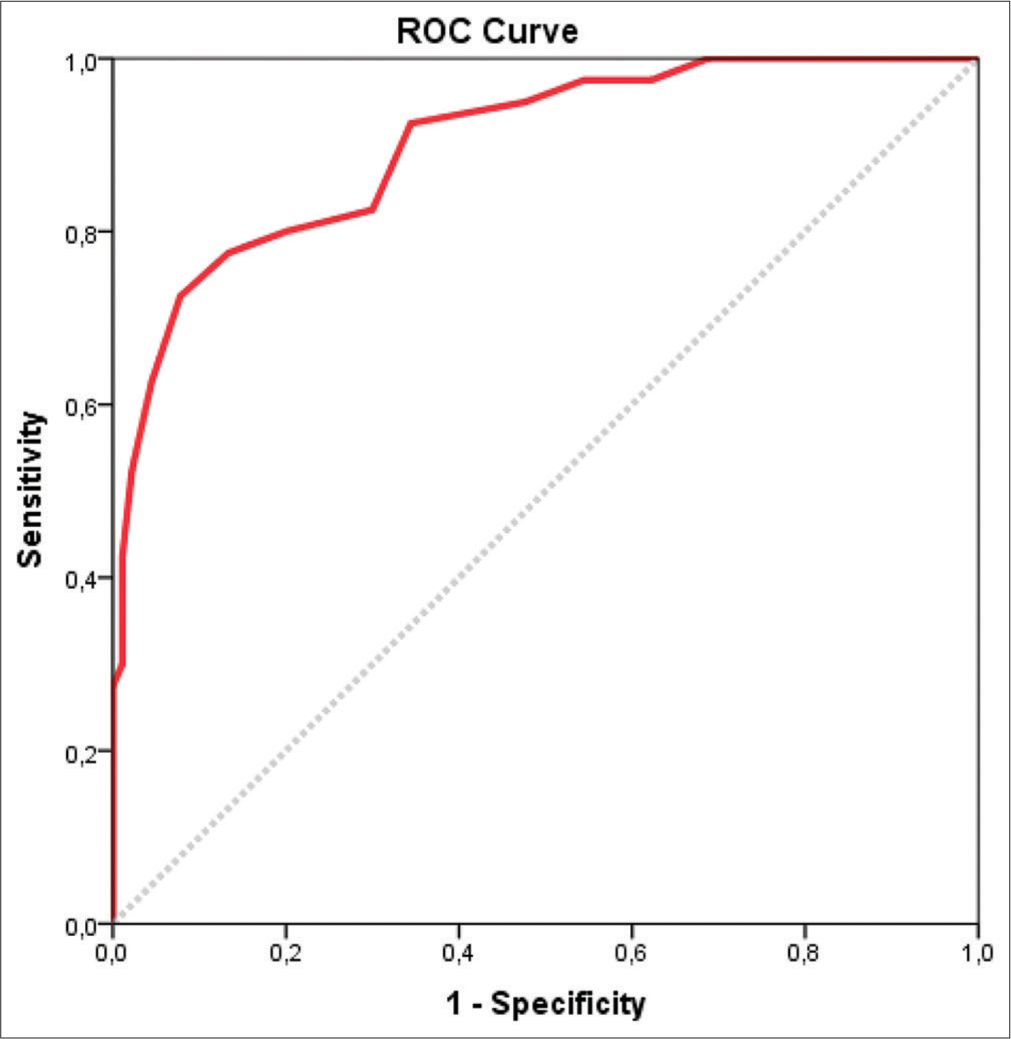
- Receiver operating curve analysis for hope total score.
DISCUSSION
The diagnosis of a chronic disease is a biographical reversal in the history of human life. This overthrow creates great needs, which require immediate satisfaction. The area in which higher levels of needs are present is that of psychological support.[34,35]
Research in the field of psychological needs, confirms that the key issues concerning hope are the scourge of shattered hope, the temporary steps toward a new state of hope, the reshaping of hope in the context of a life-threatening illness and the strengthening of hope and of prosperity.[34,36] Due to the multilevel effect of hope in the trajectory of the oncology patient, the aim of the present study was to explore the psychometric properties of the HHI in cancer patients in Greece.
The MoCA and MMSE questionnaires were used to assure the cognitive status of the participants. The prevalence of mild cognitive impairment (MCI) is not easily determined due to slightly different definitions of MCI and possible variabilities between studies resulting from factors such as the mean age of the sample.[37-39] Nevertheless, current consensus guidelines for MCI suggest the use of a standardised cognitive test as a starting point and the mini-mental and MoCA are considered accurate diagnostic tools.[24,40,41] In this context, we consider that regardless of the mean age of the sample, the use of these two tests warrants the absence of cognitive impairment of the participants.
According to the CFA in the Herth three-factor model, a three-factor model of the original HH index emerged, which, however, was characterised by unacceptable global adjustment indicators. Therefore, the model of the three factors proposed by the creator does not apply to the Greek population. Similar research has been conducted in the past by other researchers who have tried to assess the psychometric properties of the index in other countries, such as Sweden, Italy, Norway and Iran.[2,42-45] In contrast, authors of Chinese version have confirmed Herth’s factors.[16]
Exploratory factor analysis of the index followed revealed also three factors, but of different conceptual content from those of the original index. These were confirmed by CFA. In contrast to the findings of the original work, the analysis of index factors in Sweden and Norway identified two key factors, while in Iran, it was shown that the Persian version of the HH index showed a factor consisting of 11 questions interpreting 38.309% of the total variance.[2,42,44,45] These differences are expected between different countries due to different characteristics and different cultures of these countries. At the same time, it was found in our analysis that all the factors that emerged had at least two questions in common with the factors of the Herth model. However, the description of the factors was not satisfactory regarding its content; in addition, there was no internal coherence in the questions to conceptually interpret each factor separately. Therefore, the formation and structure of the three factors could not be semantically justified. The findings of this study are consistent with those of Ripamonti et al. (2012) in Italy and Geiser et al. (2015) in Germany, with a view to adopting a single-factor model, which we concluded with further statistical analysis. Our results concerning one factor solution may be due to cultural reasons.
The questionnaires used as golden rules, satisfy the validity of the criterion, while no floor or ceiling effects were observed, as <15% of participants had achieved lower or higher possible value, respectively. In the present study, based on the values of the Cronbach’s alpha coefficient, the internal consistency for the overall score of hope was excellent (0.869). Therefore, it could be argued that the overall score of hope could be used both at research and clinical levels to assess the levels of hope of Greek oncology patients. In the Dutch version of the HH index, the Cronbach’s alpha index was 0.84 for the overall score and the reliability of control and retest was 0.79.[46] The Cronbach’s alpha coefficient was very close to that observed in the present study for the overall score (0.869). The reliability of control-reexamination of the Dutch version showed a higher difference than the reliability of control-reexamination of the present research of a total score (0.902), which was higher than that of the Dutch index. Within acceptable limits, but at lower prices, the Cronbach’s alpha coefficient of reliability was observed in other versions of the HH index, such as in the Persian version and in the Italian version, while in the Persian version of HHI as examined by Soleimani and Allen (2019), the value of the Cronbach’s alpha coefficient was almost equal to that observed in the present study.[7,43] Hope and hopelessness are significant occurrences for both patients and their families in palliative care, but it is not entirely clear how they relate to each other.[47] The HHI-Gr revealed a satisfactory convergent validity whereas HHI-Gr and BHS were highly correlated. Known-groups validity reported that HHI-Gr discriminated well regarding patients with good performance status related to those with poor one.
The major strengths of this study were that no cases were omitted from the analysis due to missing data, and there was a high degree of compliance, which indicated that the format and the content of the questionnaire were acceptable for patients with cancer.
A possible limitation of the present study could be the fact that it was conducted in a cancer patient population, so results may not be generalised in patients with chronic diseases.
CONCLUSION
The present results show that the HHI-Gr could be a useful and valid instrument for measuring hope in cognitively intact patients with cancer, of a broad age spectrum, to develop interventions that aim to support them. Furthermore, studies could use the current index to obtain empirical data about the impact of hope, while it could be of great assist in research and clinical patterns as it can motivate health-care professionals to adopt new and reinforced interventions for people with cancer.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Structuring the meaning of hope in health and illness. Soc Sci Med. 1999;48:591-605.
- [CrossRef] [Google Scholar]
- The herth hope index-a psychometric study among cognitively intact nursing home patients. J Nurs Meas. 2013;21:378-400.
- [CrossRef] [PubMed] [Google Scholar]
- Hope: The power of wish and possibility. Theory Psychol. 2010;20:251-76.
- [CrossRef] [Google Scholar]
- The german version of the herth hope index (HHI-D): Development and psychometric properties. Oncol Res Treat. 2015;38:356-60.
- [CrossRef] [PubMed] [Google Scholar]
- The concept of hope in nursing 1: Its origins, background and nature. Br J Nurs. 2002;11:832-40.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and associated positive psychological variables of depression and anxiety among Chinese cervical cancer patients: A cross-sectional study. PLoS One. 2014;9:e94804.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-cultural adaptation and psychometric evaluation of the herth hope index within a sample of iranian older peoples. Int J Aging Hum Dev. 2019;89:356-71.
- [CrossRef] [PubMed] [Google Scholar]
- Hope and emotional well-being: A six-year study to distinguish antecedents, correlates, and consequences. J Posit Psychol. 2015;10:520-32.
- [CrossRef] [Google Scholar]
- Poor sleep quality, depression and hope before breast cancer surgery. Appl Nurs Res. 2017;34:7-11.
- [CrossRef] [PubMed] [Google Scholar]
- The relationships between mood disturbances and pain, hope, and quality of life in hospitalized cancer patients with pain on regularly scheduled opioid analgesic. J Palliat Med. 2010;13:311-8.
- [CrossRef] [PubMed] [Google Scholar]
- The importance of hope as a mediator of psychological distress and life satisfaction in a community sample of cancer patients. Cancer Nurs. 2010;33:258-67.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between body esteem and hope and mental health in breast cancer patients after mastectomy. Indian J Palliat Care. 2015;21:198-202.
- [CrossRef] [PubMed] [Google Scholar]
- Improving communication on hope in palliative care. A qualitative study of palliative care professionals' metaphors of hope: Grip, source, tune, and vision. J Pain Symptom Manage. 2014;48:831-8.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Solicitude: Balancing compassion and empowerment in a relational ethics of hope-an empirical-ethical study in palliative care. Med Health Care Philos. 2016;19:11-20.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in levels of hope after diagnostic disclosure among Taiwanese patients with cancer. Cancer Nurs. 2003;26:155-60.
- [CrossRef] [PubMed] [Google Scholar]
- Herth hope index: Psychometric testing of the Chinese version. J Adv Nurs. 2012;68:2079-85.
- [CrossRef] [PubMed] [Google Scholar]
- Resilience and hope during advanced disease: A pilot study with metastatic colorectal cancer patients. BMC Palliat Care. 2016;15:70.
- [CrossRef] [PubMed] [Google Scholar]
- Hope in the context of lung cancer: Relationships of hope to symptoms and psychological distress. J Pain Symptom Manage. 2010;40:174-82.
- [CrossRef] [PubMed] [Google Scholar]
- Thinking outside the box: Depression, hope, and meaning at the end of life. J Palliat Med. 2003;6:973-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hope in patients with hematological malignancy in different phases of their disease and during the phase of hematopoietic stem cell transplantation. A literature review. Hosp Res. 2014;39:140-5.
- [Google Scholar]
- Psychometric properties of hope scales: A systematic review. Int J Clin Pract. 2018;72:e13213.
- [CrossRef] [PubMed] [Google Scholar]
- Rasch analysis of the herth hope index in cancer patients. Health Qual Life Outcomes. 2018;16:196.
- [CrossRef] [PubMed] [Google Scholar]
- Abbreviated instrument to measure hope: Development and psychometric evaluation. J Adv Nurs. 1992;17:1251-9.
- [CrossRef] [PubMed] [Google Scholar]
- The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695-9.
- [CrossRef] [PubMed] [Google Scholar]
- Brief cognitive assessment of cancer patients: Evaluation of the mini-mental state examination (MMSE) psychometric properties. Psychooncology. 2007;16:352-7.
- [CrossRef] [PubMed] [Google Scholar]
- Toxicology and response criteria of the eastern cooperative oncology group. Am J Clin Oncol. 1982;5:649-55.
- [CrossRef] [PubMed] [Google Scholar]
- The experience of hopelessness in a population of Greek cancer patients receiving palliative care. Int J Soc Psychiatry. 2008;54:262-71.
- [CrossRef] [PubMed] [Google Scholar]
- The hospital anxiety and depression scale in greek cancer patients: Psychometric analyses and applicability. Support Care Cancer. 2004;12:821-5.
- [CrossRef] [PubMed] [Google Scholar]
- The hospital anxiety and depression scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14.
- [CrossRef] [PubMed] [Google Scholar]
- The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-70.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for depression and anxiety in cancer patients using the hospital anxiety and depression scale. Gen Hosp Psychiatry. 1993;15:69-74.
- [CrossRef] [Google Scholar]
- The measurement of pessimism: The hopelessness scale. J Consult Clin Psychol. 1974;42:861-5.
- [CrossRef] [PubMed] [Google Scholar]
- Psychometric properties of the beck depression inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77-100.
- [CrossRef] [Google Scholar]
- Mapping the psychosocial and practical support needs of cancer patients in Western Australia. Eur J Cancer Care. 2012;21:107-16.
- [CrossRef] [PubMed] [Google Scholar]
- Age, health, and education determine supportive care needs of men younger than 70 years with prostate cancer. J Clin Oncol. 2007;25:2560-6.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring hope and healing in patients living with advanced non-small cell lung cancer. Oncol Nurs Forum. 2014;41:497-508.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges of epidemiological studies of mild cognitive impairment. Alzheimer Dis Assoc Disord. 2004;18:1-2.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of mild cognitive impairment about elderly population in China: A meta-analysis. Int J Geriatr Psychiatry. 2011;26:558-63.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of mild cognitive impairment in diverse geographical and ethnocultural regions: The COSMIC collaboration. PLoS One. 2015;10:e0142388.
- [CrossRef] [Google Scholar]
- Author response: Practice guideline update summary: Mild cognitive impairment: Report of the guideline development, dissemination, and implementation subcommittee of the american academy of neurology. Neurology. 2018;91:373-4.
- [CrossRef] [PubMed] [Google Scholar]
- "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-98.
- [CrossRef] [Google Scholar]
- The herth hope index: A validation study within a sample of iranian patients with heart disease. Soc Health Behav. 2019;2:108-13.
- [CrossRef] [Google Scholar]
- Hope herth index (HHI): A validation study in Italian patients with solid and hematological malignancies on active cancer treatment. Tumori. 2012;98:385-92.
- [CrossRef] [PubMed] [Google Scholar]
- The swedish version of herth hope index-an instrument for palliative care. Scand J Caring Sci. 2003;17:409-15.
- [CrossRef] [PubMed] [Google Scholar]
- The Norwegian version of the Herth Hope Index (HHI-N): A psychometric study. Palliat Support Care. 2004;2:255-63.
- [CrossRef] [PubMed] [Google Scholar]
- Hope as a determinant of mental health recovery: A psychometric evaluation of the herth hope index-dutch version. Scand J Caring Sci. 2010;24(Suppl 1):67-74.
- [CrossRef] [PubMed] [Google Scholar]
- The level of and relation between hope, hopelessness and fatigue in patients and family members in palliative care. Palliat Med. 2005;19:234-40.
- [CrossRef] [PubMed] [Google Scholar]






