Translate this page into:
Hip Joint Neurolysis in a Patient with Cerebral Palsy – An Alternative Option for Pain Management
*Corresponding author: Ali Sarfraz Siddiqui, Department of Anaesthesiology, The Aga Khan University, Karachi, Sindh, Pakistan. sarfraz.siddiqui@aku.edu
-
Received: ,
Accepted: ,
How to cite this article: Siddiqui A, Shariff Y, Katto AA, Afshan G. Hip Joint Neurolysis in a Patient with Cerebral Palsy – An Alternative Option for Pain Management. Indian J Palliat Care. doi: 10.25259/IJPC_352_2024
Abstract
Hip joint disorders are frequently observed in patients with cerebral palsy (CP) due to static encephalopathy, dyskinesia and spasticity. Surgical treatments have shown improved pain relief, but sometimes, due to comorbid conditions, they are not feasible. Hip joint neurolysis is a palliative pain procedure that destroys the sensory nerves responsible for hip joint pain. We present a case of a 23-year-old girl with severe spastic CP, who presented to the pain clinic with severe left hip joint pain. Her surgical reconstruction for hip dislocation was planned, but due to anaesthesia risk and post-procedure morbidities, her mother requested non-surgical options. At the pain clinic, a diagnostic block of the anterior articular sensory nerve of the hip joint (left femoral and obturator) was done to provide 80% pain relief. After 2 weeks, a neurolytic block with 90% alcohol was then performed on the articular nerves of the left hip joint, providing 90% pain relief during routine care activities.
Keywords
Analgesia
Pain management
Peripheral nerves
INTRODUCTION
The global prevalence of cerebral palsy (CP) ranges from 2 to 6 cases per 1,000 live births, making it one of the most common neurological childhood disabilities worldwide.[1] Hip joint disorders are frequently observed in patients with CP due to static encephalopathy, which is often characterised by dyskinesia, ataxia and spasticity. These conditions lead to myostatic contractures primarily affecting the knee and hip joints.[2] The primary pathophysiology involves spastic muscles that maintain the hip in flexion, adduction and internal rotation. This positioning, combined with high muscle force from spasticity, causes the hip to be displaced in a posterior superior direction, leading to acetabular dysplasia. As dysplasia progresses, the acetabulum opens further, eventually resulting in the femoral head completely displacing from the hip joint.[3] The prevalence of hip displacement for CP patients is nearly 35%. The prevalence of hip subluxation is between 25 and 60%, and hip dislocation in 10–15% of children with CP.[4]
Multiple surgical and rehabilitative techniques have been developed to reduce hip joint deformities in children with CP. The injection of botulinum toxin A in the large muscles has been shown a reduction in spasticity, for up to 6 months.[5] Salvage treatments include proximal femoral resection, intrathecal baclofen, subtrochanteric valgus osteotomy, hip arthrodesis and prosthetic arthroplasty. Surgical treatments have shown improved pain relief and better sitting balance, with no evidence suggesting that one method is superior to another.[6]
Hip joint neurolysis is a palliative interventional pain procedure that targets and destroys the sensory nerves responsible for hip joint pain. It is indicated for severe, chronic hip pain unresponsive to conservative treatments, spasticity related to conditions like CP and painful hip deformities.
In this report, we present the case of a 23-year-old girl with severe spastic CP, who was bedridden and successfully underwent hip joint neurolysis for pain management following a hip joint dislocation.
CASE REPORT
A 23-year-old woman with spastic CP with Level -V Gross Motor Function Classification System severity was presented. She had spastic quadriplegia (all four limbs affected) with associated impairments including significant motor impairment leading to bed-bound status, intellectual disability and respiratory issues. The patient was non-ambulatory (bedbound) since childhood and was entirely dependent on her mother or caregiver for daily activities, including eating, dressing, diaper changes, bathing, repositioning in bed from supine to lateral and using a wheelchair for mobility with muscle stiffness (hypertonia), exaggerated reflexes (spasticity) and difficulty with voluntary movements.
She presented to the pain clinic with severe pain due to bilateral hip joint dislocation, as evident on the X-ray imaging. Her mother reported that, for the past 6 weeks, her daughter had been suffering from severe left hip joint pain. She was receiving analgesics like paracetamol and Nonsteroidal Anti-Inflammatory Drug regularly for her pain but inadequate relief. She cried or screamed during diaper changes or any movement in bed, especially when her pelvic area or lower limbs were touched. Due to this discomfort, she struggled to sleep and often screamed throughout the night, extremely disturbing her quality of life. The goal was to improve her quality of life by alleviating her pain with a minimally invasive technique. Written informed consent was obtained from the patient’s mother to report the case. The institution’s ethical approval committee exempted ethical approval for the case report.
A corrective sub-trochanteric osteotomy (surgical reconstruction for hip dislocation) following extensive soft tissue release was planned. However, due to anaesthesia risk and possible post-operative intensive care unit care, her mother declined consent and requested some non-surgical options. The patient was then referred to the pain physician to explore possible interventions for pain relief as an alternative to surgical correction.
At the pain clinic, the patient was evaluated and scheduled for a diagnostic block of the anterior articular sensory nerve of the hip joint. Under fluoroscopic guidance, the articular branches of the left femoral and obturator nerves [Figure 1][7] were blocked with local anaesthetic (0.25% bupivacaine) and steroids (4 mg dexamethasone). Immediately after the procedure, a reduction of more than 80% in pain was observed when moving the left hip joint. According to her mother, she remained pain-free for about 2 weeks before the pain returned, but it was below baseline level. A fluoroscopic-guided neurolytic block with 90% alcohol was then performed on the targeted nerve (articular branches of the left femoral and obturator nerves) of the left hip joint. On the follow-up visit, the patient’s mother reported more than 90% pain relief during routine care activities, sustained for 6 months (until her last follow-up). She no longer cries during diaper changes and now has a restful sleep, rarely requiring paracetamol.
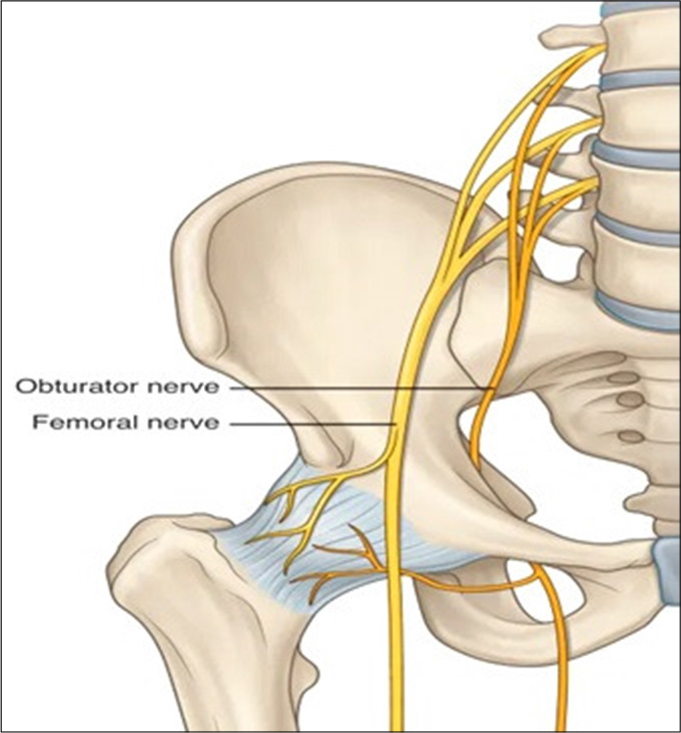
- The nerve supply of the hip joint used in ablation.
DISCUSSION
In patients with CP, surgical intervention is typically the primary approach for hip dislocation pain. The literature shows that while some patients experience improvement without surgery, long-term success is generally achieved with major arthroplasty because only soft-tissue surgery is ineffective. Open reduction with femoral osteotomy has been shown to cause a concentric reduction in patient pain; however, many patients retained their abnormal postural reflex activity, which can lead to complications such as scoliosis, pelvic obliquity, hip extension contractures and knee flexion deformities, ultimately compromising the success of the hip surgery. Thus, the prognosis regarding the surgical procedures remains uncertain.
Invasive procedures in CP patients require anaesthesia, which carries additional risks and potential morbidity. CP patients face a 63% risk of perioperative complications. Despite successful surgery, certain complications such as avascular necrosis of the femoral head, non-union and delayed union after osteotomy, heterotopic bone formation and additional fracture of already fragile bones.[8]
In such cases, parental concerns about anaesthesia-related complications, uncertain outcomes and potential for recurrence can make the decision for surgical intervention difficult. For these situations, pain management procedures offer an excellent alternative for effective pain relief and rehabilitation. Pain intervention can significantly increase the range of motion and improve the quality of life. This is particularly important as research has shown that hip pain prevalence is 56%, with pain intensity strongly correlated to the extent of degenerative cartilage lesions and the degree of femoral anteversion.[9] Therefore, effective pain management may lead to an increased range of motion.
Multiple pain interventional procedures have been used for such cases. For long-term pain relief, blocking the sensory articular branches supplying the hip joint is essential. This can be achieved either by radiofrequency ablation (RFA) or chemical neurolysis. A recent review showed an increased success rate in relieving chronic hip joint pain at 8 days–36 months after RFA; however, the analgesic benefit varied with the reduction in pain scores, ranging from 30% to more than 90% from baseline pain scores [Figure 1].[7] In another case report, where RFA was used to ablate the articular branches of the femoral nerve, accessory obturator nerve and obturator nerves in the patient for whom total hip replacement surgery was contraindicated, more than 50% pain relief was reported at 6 months, with relatively no adverse effect.
In chemical neurolysis, phenol and ethyl alcohol are used to mediate their effect by non-selectively denaturing proteins upon application to a nerve. Phenol is typically used at concentrations between 5% and 7% for spasticity, and ethyl alcohol is used at concentrations between 45% and 100%.
Regarding the safety and effectiveness of this technique, a recent study on cancer patients revealed that percutaneous neurolysis and neuromodulation are feasible, reproducible and efficient palliative therapies, achieving a 70–80% success rate in pain reduction. In addition, these methods were found to be safe, with an approximate mean complication rate of 0.5% in patients with refractory pain.
In this case, chemical neurolysis with absolute alcohol was used for multiple reasons, like altered anatomy due to hip dislocation, difficulty in positioning due to muscle spasm and contractures, patient’s inability to cooperate and communicate due to altered cognition and palliative approach due to disease and prolonged immobility and dependency. Alcohol neurolysis helps to achieve pain remission, significantly improving the quality of life for patients. By treating pain and reducing spasms in individuals with CP, neurolysis also effectively addresses palliative care aspects. Future researchers are encouraged to investigate the recurrence rate of pain after neurolysis, as this patient was only monitored for up to 6 months.
CONCLUSION
Hip joint neurolysis emerges as a pivotal treatment modality for addressing the challenging hip joint disorders characterised by dynamic pain in patients with CP. By effectively blocking pain signals, neurolysis not only alleviates pain but also enhances mobility and functionality, crucial aspects of daily living that are often compromised in CP patients. This approach offers a less invasive alternative to surgery, making it particularly suitable for those deemed unfit for surgical intervention due to anaesthesia-related concerns.
Ethical approval
The Institutional Review Board has waived ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Predicting the Prevalence of Cerebral Palsy by Severity Level in Children Aged 3 to 15 Years Across England and Wales by 2020. Dev Med Child Neurol. 2017;59:864-70.
- [CrossRef] [PubMed] [Google Scholar]
- Etiology of Hip Displacement in Children with Cerebral Palsy In: Cerebral Palsy. Cham: Springer; 2020. p. :1881-91.
- [CrossRef] [Google Scholar]
- Hip Displacement in Cerebral Palsy: The Role of Surveillance. Indian J Orthop. 2021;55:5-19.
- [CrossRef] [PubMed] [Google Scholar]
- Botulinum Toxin in the Management of Children with Cerebral Palsy. Pediatr Drugs. 2019;21:261-81.
- [CrossRef] [PubMed] [Google Scholar]
- Salvage Treatment Options for Painful Hip Dislocations in Nonambulatory Cerebral Palsy Patients. J Am Acad Orthop Surg. 2020;28:363-75.
- [CrossRef] [PubMed] [Google Scholar]
- Radiofrequency Ablation of Hip Joint Articular Nerves Aneskey. Available from: https://aneskey.com/radiofrequency-ablation-of-hip-joint-articular-nerves [Last accessed on 2024 Jul 27]
- [Google Scholar]
- Complications of Hip Treatment in Children with Cerebral Palsy In: Cerebral Palsy. Cham: Springer; 2020. p. :2049-78.
- [CrossRef] [Google Scholar]
- Incidence and Risk Factors of Hip Joint Pain in Children with Severe Cerebral Palsy. Disabil Rehabil. 2011;33:1367-72.
- [CrossRef] [PubMed] [Google Scholar]
- Radiofrequency Procedures to Relieve Chronic Hip Pain: An Evidence-Based Narrative Review. Reg Anesth Pain Med. 2018;43:72-83.
- [CrossRef] [PubMed] [Google Scholar]






