Translate this page into:
Impact of COVID-19 Pandemic on Palliative Care Workers: An International Cross-sectional Study

*Corresponding author: Liliana De Lima, International Association for Hospice and Palliative Care, Houston, Taxes, United States. ldelima@iahpc.com
-
Received: ,
Accepted: ,
How to cite this article: Pastrana T, De Lima L, Pettus K, Ramsey A, Napier G, Wenk R, et al. Impact of COVID-19 pandemic on palliative care workers: An international cross-sectional study. Indian J Palliat Care 2021;27(2):299-305.
Abstract
Objectives:
The COVID-19 pandemic and the measures taken to mitigate spread have affected countries in different ways. Healthcare workers, in particular, have been impacted by the pandemic and by these measures. This study aims to explore how COVID-19 has impacted on palliative care (PC) workers around the world.
Materials and Methods:
Online survey to members of the International Association for Hospice and PC during the initial months of the COVID-19 pandemic. Convenience sampling was used. Statistical descriptive and contingency analyses and Chi-square tests with P < 0.05 were conducted.
Results:
Seventy-nine participants (RR = 16%) from 41 countries responded. Over 93% of those who provide direct patient care reported feeling very or somewhat competent in PC provision for patients with COVID-19. Eighty-four felt unsafe or somewhat safe when caring for patients with COVID-19. Level of safety was associated with competence (P ≤ 0.000). Over 80% reported being highly or somewhat affected in their ability to continue working in their PC job, providing care to non-COVID patients and in staff availability in their workplace. About 37% reported that availability and access to essential medicines for PC were highly or somewhat affected, more so in low-income countries (P = 0.003).
Conclusion:
The results from this study highlight the impact of COVID-19 on the provision of PC. It is incumbent on government officials, academia, providers and affected populations, to develop and implement strategies to integrate PC in pandemic response, and preparedness for any similar future events, by providing appropriate and comprehensive education, uninterrupted access to essential medicines and personal protective equipment and ensure access to treatment and care, working together with all levels of society that is invested in care of individuals and populations at large. The long-term effects of the pandemic are still unknown and future research is needed to monitor and report on the appropriateness of measures.
Keywords
COVID-19 pandemic
Healthcare workers
Palliative care
INTRODUCTION
The “tsunami of suffering”[1] unleashed by the SARS-CoV-2 disease 2019 (COVID-19) global pandemic underscores the crucial role of palliative care (PC) in the comprehensive relief of health-related suffering[2] and the need to integrate PC in epidemic response and preparedness plans. Health systems that integrate PC in their COVID-19 response prioritise symptom management and appropriate communication that relieve the acute physical, psychosocial and spiritual suffering of affected patients and families.[3] PC is a component of health care, including acute conditions and in emergency situations.[4] There is no precedence of such a global pandemic in modern world – however, the role of PC is applicable in COVID-19 and other similar diseases.
Since the first COVID-19 case was reported in December 2019 by Dong et al.,[5] the pandemic has affected countries in different ways. Governments have implemented control measures in the effort to minimise transmission and mortality and mitigate the impact on health systems. Many countries enforced lockdowns, allowing only essential workers to leave their homes. Health care systems in high-income countries have focused on expanding intensive care resources and delaying non-essential interventions to expand their ability to treat patients with COVID-19 and respiratory failure. All the measures have had both positive and negative effects on society in general and on health workers in particular.[6-9] The importance of PC in pandemics and humanitarian crises and emergencies has been reported and is increasingly being recognised.[10-12]
In an effort to evaluate and assess the impact of the COVID-19 pandemic on PC workers, the International Association for Hospice and PC (IAHPC) conducted a cross-sectional online survey using Survey Monkey with its individual members. The survey consisted of multiple choice and open-ended questions. For example, participants could select among several options, including Highly affected; Somewhat affected, Not affected at all; Don’t know/Unsure. We expected that participants would report being highly affected or somewhat affected.
The objective of the study was to explore how COVID-19 has impacted PC workers around the world.
MATERIALS AND METHODS
An ethics review board of the Fundacion FEMEBA in Argentina approved the study.
The study consisted of a 20-question self-assessment survey, grouped into three blocks: The first block “Personal capacity and safety” assessed the impact of COVID-19 on participants (5 items). Questions included how respondents assessed their level of competency in caring for patients with COVID-19, how safe they felt when caring for those patients using a 3-point scale: “Not at all safe,” “Somewhat safe” and “Very safe,” and the availability of personal protective equipment (PPE) with the following scale “Appropriate,” “Adequate,” “Insufficient” and “We do not have any PPE.”
A second block “Impact of the COVID-19 pandemic in care provision” of five questions assessed the impact on their ability to work and the impact on their institutions, using a 3-point answer scale (“Not affected at all,” “Somewhat affected” and “Highly affected” with the additional option “Don’t know/unsure”). This block covered the following domains: (1) Ability to continue working in usual role/job in PC, (2) service provision to non-COVID-19 PC patients, (3) staff availability in their own setting and (4) access to essential medicines for pain relief and PC. Respondents were provided space to elaborate on the situation and describe any adaptive/ coping strategies they may have implemented. A third block of five questions referenced the global policy documents and resolutions relevant to the COVID-19 pandemic and the advocacy strategies of national PC associations. Participants were given the opportunity to provide comments in text boxes, explaining or expanding on their responses.
Five IAHPC staff members piloted the survey for content validity and recommended changes that were implemented prior to distribution. This paper describes the quantitative results from the first two blocks of questions described above. A separate report with the qualitative analysis of the comments will be prepared and submitted for publication.
The survey was developed using SurveyMonkey© and distributed to IAHPC individual members by email. The survey was opened on 28 May and closed on 30 June 2020. An invitation to participate was sent on the 1st day to 979 individuals through email followed by a reminder on 22 June. Participants were provided with general information about the study as well as the objectives of the survey. Before responding, they had to confirm that their participation was voluntary and that they were 18 years or older. The survey was not anonymous, and participants were asked if an IAHPC staff member could contact them for follow-up interviews. As a gesture of gratitude, IAHPC extended the annual memberships of those who completed the survey by 3 months.
Data were collected in Excel. Quantitative data were cleared of all incomplete data sets and exported to SPSS (v. 25, IBM Corporation, Armonk, USA) for the analyses. Data were stored in a secure account in the cloud, using Microsoft Office OneDrive. A statistical descriptive analysis as well as contingency analysis of all selected questions was conducted. The countries were dichotomised in high/more resourced (high-income countries [HICs] and upper-middle-income countries [UMICs]) and low/fewer resourced (lower-middle-income countries [LMICs] and low-income countries [LICs]). According to the World Bank, in 2019, countries with $1035 or less GNI per capita were classified as low income, $1036–$4045 lower-middle income, $4046–$12,535 as upper-middle income and over $12,536 as high income.[13] Chi-square tests were used for the latter, considering P < 0.05 statistically significant.
RESULTS
The email was opened by 494 members. Seventy-nine participants (response rate = 16%) from 41 countries responded the survey, representing between 14% and 22% of all the countries in each income category. Participants were mostly from HIC (34.2%) followed by LMIC (33%). Table 1 shows the distribution of participants by income group according to the World Bank classification.
| Income group* | Countries represented in survey: Number/total category (% of group) and list | Participants per income group (%) |
|---|---|---|
| HIC | 14/83 (17%) Australia, Bahamas, Canada, Chile, Germany, Israel, Italy, New Zealand, Norway, Panama, Sweden, Trinidad and Tobago, United Kingdom, United States |
27 (34.2) |
| UMIC | 12/56 (21%) Argentina, Brazil, Bulgaria, China, Costa Rica, Ecuador, Guatemala, Indonesia, Lebanon, Malaysia, Peru, South Africa |
20 (25.3) |
| LMIC | 11/50 (22%) El Salvador, India, Kenya, Moldova, Nepal, Nicaragua, Nigeria, Philippines, Sri Lanka, Tanzania, Zimbabwe |
26 (32.9) |
| LIC | 4/29 (14%) Haiti, Malawi, Mozambique, Uganda |
6 (7.6) |
The regional representation was proportional to the IAHPC membership distribution[14] in each of the World Health Organisation’s (WHO) regions. Most of the participants were located in countries in the Americas (WHO region PAHO, n = 24; 30.4%) followed by Africa (WHO region AFRO, n = 17; 21.5%) and Western Pacific (WHO region WPRO, n = 16; 20.3%).
Personal capacity and safety
Twenty-three (29.1%) of the participants provide direct patient care for COVID-19 patients. Over 93% of those reported feeling very or somewhat competent in the provision of PC for patients with COVID-19 [Table 2]. No significant association was found between level of competence and having cared for patients with COVID-19 (Chi2 [2, n = 59] = 0.139, P = 0.933) nor between level of competence and country income group (Chi2 [4, n = 63] = 0.829, P = 0.935). More than half of the participants (n = 45; 57%) reported availability of PPE as adequate or appropriate. Participants in countries with more resources (HIC and UMIC) reported this significantly more often than those in countries with fewer resources (LMIC and LIC) (Chi2 [2, n = 67] = 10.946, P = 0.004).
| Features | n (%) |
|---|---|
| Care of patients with COVID-19 | |
| Yes | 23 (33.8) |
| No | 45 (66.2) |
| Level of competency in the provision of PC for patients with COVID-19* | |
| Very competent | 19 (32.2) |
| Somewhat competent | 37 (62.7) |
| Not competent at all | 3 (5.1) |
| Level of safety when providing care to patients with COVID-19* | 9 (16.4) |
| Very safe | |
| Somewhat safe | 38 (69.1) |
| Not safe at all | 98 (14.5) |
| Availability of personal protective equipment (PPE) for palliative care consult/visits | |
| Appropriate | 21 (26.6) |
| Adequate | 24 (30.4) |
| Insufficient | 22 (27.8) |
| Do not have any | 2 (2.5) |
| Not sure | 10 (12.7) |
A large percentage (84.2%) of participants who provide direct patient care felt either unsafe or somewhat safe when caring for patients with COVID-19 (n = 9 and 39, respectively). A highly significant association was found between the perceived level of safety and level of competence (Chi2 [4, n = 57) = 27.282, P ≤ 0.000) and the availability of PPE (Chi2 [4, n = 52] = 14.208, P = 0.007). No significant association was found between the level of safety and country income group (Chi2 [4, n = 57] = 2.433, P = 0.296).
Impact of the COVID-19 pandemic in care provision
Figure 1 summarises participants’ responses regarding the impact of the pandemic on their institutions’ and their personal ability to continue providing care to patients with PC needs.
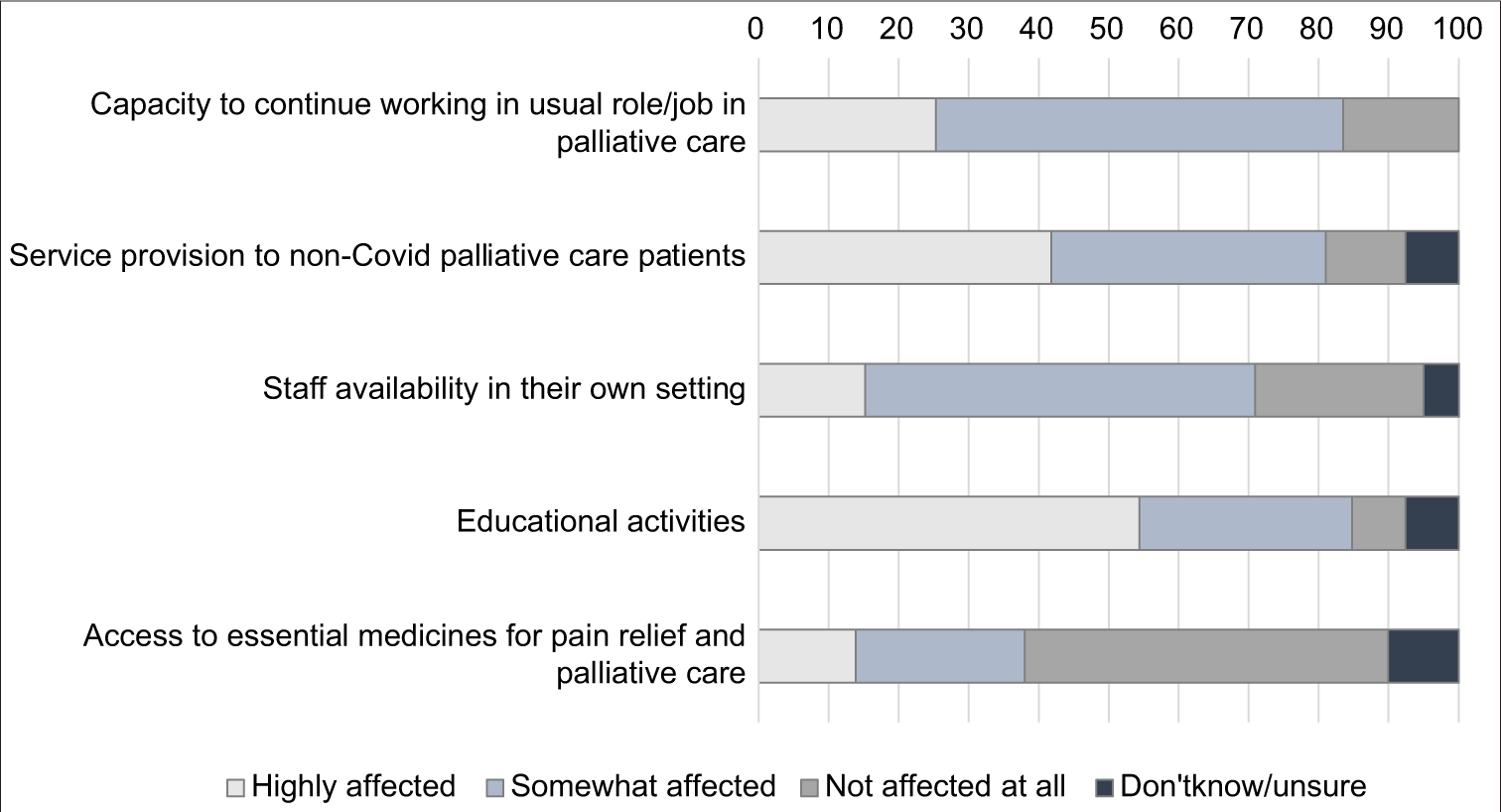
- Impact of the Covid-19 pandemic in care provision.
Ability to continue working
A large percentage (n = 66; 83.5%) of the participants reported being highly affected or somewhat affected in their ability to continue working in their PC role/job. A significant association was found between caring for patients with COVID-19 and being highly affected by the pandemic in their work (Chi2 [2, n = 68] = 8.958, P = 0.011). Ability to continue working was not associated with feeling of competency (Chi2 [4, n = 63] = 3.454, P = 0.485) or feeling safe (Chi2 [4, n = 57] = 2.815, P = 0.589). Ability to continue working was unrelated to country income group (Chi2 [4, n = 57] = 7.309, P = 0.120).
Care provision to non-COVID PC patients
The vast majority of the participants reported that the COVID-19 pandemic highly affected or somewhat affected (42% and 40%, respectively) their care provision to nonCOVID PC patients in their community or home settings. No significant association was found between the impact on the service provision to non-COVID PC patients and country income group (Chi2 [2, n = 75] = 7.309, P = 0.178).
Staff availability
More than half of the participants (n = 44; 55.7%) reported that the COVID-19 pandemic “somewhat affected,” staff availability in their workplace (as a result of death, sick leave, furlough, terminated or inability to work related to lockdowns – i.e., childcare) and 15.2% (n = 12) reported being highly affected.
Access to essential medicines for pain relief and PC in work setting
About 30% (n = 11) reported that the availability and access to essential medicines for PC and pain relief in their work setting were highly affected, and 24.1% (n = 19) reported availability as somewhat affected by the pandemic. Access to essential medicines for pain relief and PC for COVID and non-COVID PC patients was significantly less impacted in countries with more resources (HIC and UMIC) compared to LMIC and LICs (Chi2 [2, n = 67] = 11.893, P = 0.003).
DISCUSSION
By assessing the impact of COVID-19 pandemic, we found out that all aspects related with “personal capacity and safety” and “care provision” were affected.
Personal capacity and protection
Only one-third of PC professionals responding to the survey reported caring for patients with COVID-19, indicating both the limited integration of PC with communicable disease divisions and possibly reflecting a lack of awareness of the need for such integration.[15] Numerous publications have called for the integration of PC in rapid response plans and recognise the benefits of this type of comprehensive strategy.[1,10,16,17]
On a positive note, a large majority of respondents reported feeling very or somewhat competent to provide PC to COVID-19 patients. The PC community has called for the inclusion of basic PC training in all medical and nursing schools[18,19] for many years. This includes the knowledge and skills to appropriately manage symptoms frequently occurring in COVID-19 patients, such as dyspnoea, depression, diarrhoea and anxiety, and the competency to appropriately communicate with patients and families regarding goals of care and expectations of treatment and interventions.[3]
Feelings of safety were related to perceptions regarding adequacy of PPE as well as the perceptions of competence. According to the WHO, only 26% of member states report having occupational safety plans for healthcare workers.[20] Almost 25% of the respondents (all located in lower and LICs) cited insufficient availability of PPE or none at all. When asked about strategies and adaptive responses, participants reported using innovative approaches, such as the uptake and integration of telemedicine and manufacturing inexpensive PPE using large plastic garbage bags. Respondents’ comments will form the basis of a qualitative paper based on the survey analysis.
Impact of the COVID-19 pandemic in care provision
A large percentage of the participants reported being highly or somewhat affected in their ability to continue in their usual role/job in PC, regardless of their respective country’s income group, reflecting the global scale of this pandemic. Similarly, a vast majority of the participants reported that the COVID-19 pandemic highly or somewhat affected their care provision to non-COVID PC patients in the patients’ own setting, regardless of the country’s income level. Both responses underscore the need to develop and implement strategies to ensure that patients with non-communicable diseases and other conditions continue to access and receive much-needed treatment and care. Some of these include implementing safety protocols for consultation services, proactively reaching out to patients who may have missed appointments and using telemedicine technology when possible.
A large majority of the participants reported that the effects of the pandemic affected staff availability, as their coworkers dropped out of the workforce due to quarantine, sickness or death, or were unable to work due to lockdown effects for example, the closure of in-person classes in schools forcing parents to stay at home to care for children. This resulted in work overload, feelings of burnout and increased levels of anxiety and stress among healthcare workers.
Respondents in countries with fewer resources reported most frequently on the pandemic’s negative impact on access to essential medicines for pain relief and PC than their counterparts in HICs. This is a significant finding which underscores the inequity of the high burden of health-related suffering borne by patients in poor settings. The finding is confirmed by the numerous pre-pandemic reports and extensive studies showing limited availability and access to essential medicines for pain relief and PC in low and LMICs.[21-24] Some medicines such as opioids may be used for non-COVID and COVID patients, including opioids for pain relief and breathlessness. The global PC community[25-27] and UN special organisations such as the WHO, the Commission on Narcotic Drugs,[28] the Human Rights Council[29] and the International Narcotics Control Board[30] have been calling on member states to improve availability and ensure access to essential PC medicines for years. Some of these essential medicines have been regulated under the international drug control conventions for more than half a century and this makes improving system-level access, particularly during a pandemic, a high-level, evidence-based and multistakeholder process. In member states that have yet to undertake this process, shortages and stockouts are endemic. In many countries and regions, where survey participants live and work, access to morphine for the treatment of respiratory distress associated with the COVID-19 is limited or nonexistent.[31]
The COVID-19 pandemic has resulted in enormous suffering across the world.[32] Although there have been some national and regional reports on preparedness of PC services to respond to the pandemic,[33,34] this study is the first we know of to report on the impact of the COVID-19 pandemic on PC workers around the world, with participation of individuals in different geographical regions and income groups. The extent of the impact is perceived and experienced differently in different countries and this study provides some insight into this differential impact.
Study limitations
Limitations of this study are inherent to any convenience sample or cross-sectional study. Self-reporting bias may have also affected responses. The content of the questionnaire was validated but no statistical test was carried on for further validation. The IAHPC is an international membership organisation with members located in all regions of the world and, thus, one of the few with such a database of PC workers. This sample may not be representative of the global PC workforce and thus the results are not globally generalisable. However, this paper provides a glimpse into the challenges and current situations faced by PC providers around the world during the COVID-19 pandemic which may be happening across countries.
The response rate was low and there may be several reasons. During the time when the survey was conducted: (1) Many healthcare workers were struggling with a high workload due to the pandemic. (2) Numerous surveys and webinars were being disseminated and offered, possibly affecting the willingness, ability and interest of participants to respond. (3) Many workers were under lockdown and ordered to stay at home. Workers from LICs often face technical difficulties with internet access, which affects their ability to participate. (4) Some may not feel comfortable sharing information on what may be considered failures or limitations to appropriate protection, human resource management or response preparedness in their workplaces or health systems. In spite of this, a response rate below 10% is not uncommon for online surveys.[35]
The survey was implemented during a limited time frame in the 1st months of the epidemic trajectory, but the course of the pandemic varies between the countries regarding onset, speed, severity and response. Therefore, it was not possible to relate individual responses with the phase of the pandemic in each of the participant’s country or extrapolate any data for specific pandemic stages. The follow-up qualitative analysis of the respondents’ comments will add to a more in-depth interpretation of the data.
CONCLUSION
The pandemic had an impact on the global PC workforce. The results from this study highlight this impact on the provision of PC to non-COVID patients and on the already limited access to essential medicines – especially opioids – needed for the control of common COVID-19 symptoms and other palliative conditions. Inclusion of PC in national pandemic responses, especially for patients unable or unwilling to access, or triaged away from intensive treatment and ventilator support, will improve patient quality of life, relieve caregiver stress and reduce the clinical burden on critical care professionals. PC team members be helping discuss advance care planning and triaging care for patients, particularly vulnerable adults – physical and mental disability and those on the fringes of society and how would this look in different societies. It is incumbent on government officials, academia, providers and affected populations, to develop and implement innovative and inexpensive strategies to provide appropriate and comprehensive education, uninterrupted access to essential medicines and PPE and ensure access to treatment and care for patients and families with PC needs. The long-term effects of the pandemic are still unknown and future research is needed to monitor and report on the appropriateness of measures taken to slow the spread and containment as well as of treatments and other clinical interventions.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The key role of palliative care in response to the COVID-19 tsunami of suffering. Lancet. 2020;395:1467-9.
- [CrossRef] [Google Scholar]
- Redefining palliative care-A new consensus-based definition. J Pain Symptom Manage. 2020;60:754-64.
- [CrossRef] [Google Scholar]
- Clinical Management of COVID-19 - Interim guidance. 2020. Geneva: WHO; Available from: https://apps.who.int/iris/rest/bitstreams/1278777/retrieve [Last accessed on 2020 Oct 03]
- [Google Scholar]
- Integrating Palliative care and Symptom Relief Into Responses to Humanitarian Emergencies and Crises: A WHO Guide Geneva: World Health Organization; 2018.
- [Google Scholar]
- An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533-4.
- [CrossRef] [Google Scholar]
- The Distributional Effects of COVID-19 and Mitigation Policies Globalization and Monetary Policy Institute Working Paper No 400. 2020. Available from: https://ssrn.com/abstract=3686276 or http://dx.doi.org/10.24149/gwp400 [Last accessed on 2020 Oct 03]
- [CrossRef] [Google Scholar]
- Impact on mental health care and on mental health service users of the COVID-19 pandemic: A mixed methods survey of UK mental health care staff. Soc Psychiatry Psychiatr Epidemiol. 2021;56:25-37.
- [CrossRef] [Google Scholar]
- Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol. 2020;5:886-7.
- [CrossRef] [Google Scholar]
- Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int J Emerg Med. 2020;13:40.
- [CrossRef] [Google Scholar]
- The role and response of palliative care and hospice services in epidemics and pandemics: A rapid review to inform practice during the COVID-19 pandemic. J Pain Symptom Manage. 2020;60:e31-40.
- [Google Scholar]
- Palliative care in humanitarian crises: A review of the literature. J Int Humanitarian Action. 2018;3:5.
- [CrossRef] [Google Scholar]
- Palliative care in humanitarian crises: Always something to offer. Lancet. 2017;389:1498-9.
- [CrossRef] [Google Scholar]
- World Bank Country and Lending Groups. 2020. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Last accessed on 2020 Sep 13]
- [Google Scholar]
- IAHPC Members. 2020. Available from: https://hospicecare.com/members-section/iahpc-members-list/ [Last accessed on 2020 May 17]
- [Google Scholar]
- Integration of palliative care into COVID-19 pandemic planning. BMJ Support Palliat Care. 2021;11:40-4.
- [CrossRef] [Google Scholar]
- Pandemic palliative care: Beyond ventilators and saving lives. CMAJ. 2020;192:E400-4.
- [Google Scholar]
- To face coronavirus disease 2019, surgeons must embrace palliative care. JAMA Surg. 2020;155:681-2.
- [CrossRef] [Google Scholar]
- Nursing education on palliative care across Europe: Results and recommendations from the EAPC Taskforce on preparation for practice in palliative care nursing across the EU based on an online-survey and country reports. Palliat Med. 2021;35:130-41.
- [CrossRef] [Google Scholar]
- Primary palliative care education for trainees in U.S. medical residencies and fellowships: A Scoping Review. J Palliat Med. 2021;24:354-75.
- [CrossRef] [Google Scholar]
- Weekly Operational Update on COVID-19. 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/weekly-updates/wou-9-september-2020-cleared.pdf?sfvrsn=d39784f7_2 [Last accessed on 2020 Sep 25]
- [Google Scholar]
- Use of and barriers to access to opioid analgesics: A worldwide, regional, and national study. Lancet. 2016;387:1644-56.
- [CrossRef] [Google Scholar]
- Solving the global crisis in access to pain relief: Lessons from country actions. Am J Public Health. 2019;109:58-60.
- [CrossRef] [Google Scholar]
- The Global Opioid Policy Initiative (GOPI) project to evaluate the availability and accessibility of opioids for the management of cancer pain in Africa, Asia, Latin America and the Caribbean, and the Middle East: Introduction and methodology. Ann Oncol. 2013;24(Suppl 11):i7-13.
- [Google Scholar]
- Global disparities in access to pain relief In: Abd-Elsayed A, ed. Pain: A Review Guide. Cham: Springer International Publishing; 2019. p. :1185-9.
- [Google Scholar]
- The Declaration Montreal: Access to pain management is a fundamental human right. Pain. 2011;152:2673-4.
- [CrossRef] [Google Scholar]
- Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: The Lancet Commission report. Lancet. 2018;391:1391-454.
- [CrossRef] [Google Scholar]
- An interdisciplinary working group to advocate universal palliative care and pain relief access. J Palliat Med. 2020;23:882-3.
- [CrossRef] [Google Scholar]
- Ensuring Availability of Controlled Medications for the Relief of Pain and Preventing Diversion and Abuse Striking the Right Balance to Achieve the Optimal Public Health Outcome. 2011. Discussion Paper Based on a Scientific Workshop New York: UN. Available from: https://www.unodc.org/docs/treatment/Pain/Ensuring_availability_of_controlled_medications_FINAL_15_March_CND_version.pdf [Last accessed on 2020 Sep 20]
- [Google Scholar]
- Right to Pain Relief: 5.5 Billion People Have no Access to Treatment, Warn UN Experts World Hospice and Palliative Care Day - Saturday 10 October 2015. 2015. Available from: https://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=16590 [Last accessed on 2020 Aug 30]
- [Google Scholar]
- Progress in Ensuring Adequate access to Internationally Controlled Substances for Medical and Scientific Purposes Vienna. 2019. Available from: https://www.incb.org/documents/Publications/AnnualReports/AR2018/Supplement/Supplement_E_ebook.pdf [Last accessed on 2020 Sep 12]
- [Google Scholar]
- INCB. WHO and UNODC Statement on Access to Internationally Controlled Medicines during COVID-19 Pandemic Vienna and Geneva: INCB, WHO, UNODC. 2020. Available from: https://www.incb.org/incb/en/news/news_2020/incb--who-and-unodc-statement-on-access-to-internationally-controlled-medicines-during-covid-19-pandemic.html [Last accessed on 2020 Sep 12]
- [Google Scholar]
- The alleviation of suffering during the COVID-19 pandemic. Palliat Support Care. 2020;18:376-8.
- [CrossRef] [Google Scholar]
- Preparedness of African palliative care services to respond to the COVID-19 pandemic: A rapid assessment. J Pain Symptom Manage. 2020;60:e10-26.
- [Google Scholar]
- Response and role of palliative care during the COVID-19 pandemic: A national telephone survey of hospices in Italy. Palliat Med. 2020;34:889-95.
- [CrossRef] [Google Scholar]
- Improving web survey efficiency: The impact of an extra reminder and reminder content on web survey response. Int J Soc Res Methodol. 2017;20:317-27.
- [CrossRef] [Google Scholar]






