Translate this page into:
Improving Access and Quality of Palliative Care in Kerala: A Cross-sectional Study of Providers in Routine Practice
Address for correspondence: Dr. M. R. Rajagopal, Trivandrum Institute of Palliative Sciences and Pallium India, Aisha memorial hospital Building, Paruthikuzhy, Manacaud P.O, Thiruvananthapuram - 695 009, Kerala, India. E-mail: chairman@palliumindia.org
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Expanding access and improving quality of palliative care in low-middle income countries is a pressing priority.
Objective:
The objective of the study was to describe structure and processes of care across government (GO) and non-GO (NGO) palliative care providers (PCPs) in Kerala, India.
Design:
This was a cross-sectional telephone survey.
Setting/Subjects:
This study consisted of 200 randomly selected PCPs across Kerala. The survey explored organizational structure, patient assessment, opioid availability, and explored elements considered essential to palliative care delivery in the Indian context.
Results:
One hundred GO and 100 NGO PCPs agreed to participate (100% response rate). The annual median number of new patients was 183 and 159 in GO and NGO PCPs, respectively. The median number of annual home visits in GO PCPs was 1398 and in NGO PCPs was 979. Median number of outpatient visits in GO PCPs was 600 and in NGO PCPs was 520. Only 24% (47/200) of the PCPs had full-time physicians with training in palliative care; 60% of GO PCPs had no full time physician with training in palliative care. Patient-reported pain was routinely documented by 21% (21/100) and 65% (65/100) of the GO and NGO sites, respectively (P < 0.001). None of the GO and only 36% (36/100) of NGO PCPs were able to prescribe oral morphine. Psychosocial and spiritual issues were documented routinely in only 4% (4/100) and 48% (47/99) of the GO and NGO PCPs, respectively (P < 0.001).
Conclusions:
Caution is needed against potential challenges to quality care in any new initiative. Kerala has achieved remarkable success in the coverage of palliative care through hundreds of locally active NGOs through GO machinery involving every primary health center. Yet, there are gaps such as absence of full-time physicians. This study highlights the need for periodic review to identify gaps in care.
Keywords
Access to care
global health
health policy
health services research
palliative care
quality of care
INTRODUCTION
Kerala has long been regarded as one of the “leading lights” of palliative care in low-middle income countries (LMICs).[12] This recognition stems from a cumulative set of events over the past three decades bringing together the activities of clinicians, community volunteers and advocates, and policymakers. The Pain and Palliative Care Society (PPCS) was established as a nongovernmental organization in Calicut in 1993. PPCS was subsequently recognized as a demonstration project by the World Health Organization in 1995. Over the next 10 years, about 40 palliative care clinics were established in various parts of Kerala; most of these clinics included substantial participation of community members. Pallium India, based in Trivandrum, was created in 2003 as a national advocacy and educational organization. Finally, the state government (GO) of Kerala adopted a palliative care policy in 2008, declaring palliative care as an integral component of standard health care. By that time, Kerala was already leading India with 83 of India's 139 palliative care service providers.[3]
In recent years, there has been a concerted effort to expand palliative care services within Kerala. This has led to efforts to measure and evaluate the existing services such that gaps in care can be identified to drive improvements in health system performance. In 2006, Pallium India assembled a working group that generated a standards audit tool for Indian palliative care programs. The audit tool measures seven domains of care: structure and processes of care; training of personnel; physical, psychosocial, and spiritual dimensions; drug availability; ethical and legal aspects; organizational aspects; and quality.[4] In 2008, this audit tool was distributed to 86 palliative care providers across India; the response rate was 57% (n = 49).[5] While the majority of providers met most standards that were considered essential, the sample size was small, and the results may not reflect care in most regions of India. In the next phase of this project, we sought to apply a modified version of this tool to a broader sample of GO and non-GO (NGO) palliative care programs across the state of Kerala. The primary objective of this cross-sectional study was to understand the extent to which the existing centers in Kerala are able to meet minimum standards of palliative care. It is hoped that data from this exercise will be helpful for policymakers as they undertake efforts to improve accessibility and quality of palliative care in Kerala and other parts of India.
METHODS
Study setting
Kerala is located on the South West Coast of India and has a population of approximately 33 million. Kerala has the highest literacy (94% vs. 73% national rate), greatest life expectancy (74 years vs. 64 years), and the lowest infant mortality rate in India.[6] Kerala is widely recognized as a global leader in community oriented palliative care.[12] More than 900 panchayats (local self-GO institutions each catering to a population of approximately 35,000–45,000) each has one trained palliative care nurse visiting patients in their homes at least once a month. More than 200 NGO organizations across Kerala are involved in providing palliative care. In addition to providing care to people with prolonged serious illnesses, Kerala's palliative care community provides service to people with psychiatric illness and spinal cord injuries with the incorporation of physiotherapy and vocational rehabilitation together with medical care, nursing care, and psychosocial support.
Palliative care in Kerala is currently delivered in a number of diverse settings by a variety of organizations. GO hospitals, private hospitals, and community-based NGOs deliver palliative care services to inpatients, outpatients, and through mobile PCPs at home. Methadone and morphine are the only orally available opioid's in Kerala and can only be dispensed by an approved provider affiliated with a “Recognized Medical Institution” (RMI). Physicians may stock and dispense oral morphine in their institutions only if they have had a minimum of 10 days of hands-on training in pain relief and palliative care.[7]
Study design
A cross-sectional survey was administered via telephone interview to designated representatives from a convenience sample of 100 GO and 100 NGO palliative care providers (PCPs) in Kerala. One hundred GO PCPs were randomly selected from the 170 primary health centers (PHCs) (n = 170) in Kerala that provide continuous 24 hour health services.[8] One hundred NGO PCPs were randomly selected from 345 PCPs registered with the Indian Association of Palliative Care, Kerala Branch. Eligible PCPs were contacted initially by phone and mail with an invitation letter that provided information about the study and a consent form. Interviews were subsequently conducted by telephone during October 2018–January 2019; interviews were typically 15–30 min in duration. The study was granted clearance by the Institutional Ethics Committee of the Trivandrum Institute of Palliative Sciences (TIPS). The study was also approved by the State Directorate of Health Services.
Survey and data capture
The survey was developed by the multidisciplinary research team and piloted on 10 PCPs before undergoing final revision. Themes explored in the interview related to basic information about the PCP, patient assessment and documentation, access to opioids, members of the clinical team, organizational culture, community outreach, and enablers/barriers to delivery of high-quality palliative care. The questions/themes included in the survey were identified by the research team based on the clinical experience together with the standard audit tool for Indian palliative care programs that was developed in 2006.[4] The survey was also designed in the light of observations from our previous research related to care delivery in Kerala.[910] Data were recorded during the interview on paper data forms and subsequently entered into a Microsoft Excel database. Parallel to this quantitative study, another study will involve detailed qualitative interviews of physicians, nurses, volunteers, and policymakers from 20 PCPs. This second project is ongoing and will be reported separately.
Statistical analysis
Differences in proportions were tested using the Chi-square test; Fisher's exact test was used for those cell values of <5. The results were considered statistically significant at P < 0.05. Analyses were performed using Microsoft Excel and 'R' Software version 3.3.0.
RESULTS
Participating palliative care providers and delivery of clinical care
Two hundred PCPs (100 each from the GO and NGO sectors) were invited to participate in the cross-sectional survey; all of them were accepted. Interviews were conducted with nurses (65%, 130/200), physicians (20%, 40/200), and administrators (15%, 30/200). Participating PCPs were located in each of the three regional zones: Northern Zone (n = 71), Central Zone (n = 54), and Southern Zone (n = 75). As shown in Figure 1, while half of the NGO PCPs were initiated during 1991–2005, GO PCPs were not initiated until 2008. During 2008–2013, there was a substantial expansion in the number of GO PCPs. Funding for NGO PCPs came primarily from public philanthropy (82%, 82/100) and project-based grants (17%, 17/100).

- Year of initiation among 200 government and nongovernment palliative care palliative care providers in Kerala, India
Clinical care was delivered primarily via home visits (100% [100/100] GO PCPs, 98% [98/100] NGO PCPs) and on-site outpatient clinics (94% [94/100] GO PCPs, 78% [78/100] NGO PCPs) [Table 1]. On-site inpatient PCPs were less common, especially within GO PCPs (2% [2/100] vs. 14% [14/100]), P = 0.003 [P < 0.05]).
| PCPs | ||
|---|---|---|
| GO (n=100) (%) | NGO (n=100) (%) | |
| Setting of care | ||
| Home visit | 100 | 98 |
| Outpatient clinic | 94 | 78 |
| Inpatient unit | 2 | 14 |
| Annual case volumes (median) | ||
| New patients | 183 | 159 |
| Home visits | 1398 | 979 |
| Outpatient visits | 600 | 520 |
| Members of the clinical team | ||
| Physicians | 94 | 40 |
| Nurses | 100 | 97 |
| Social workers | 10 | 31 |
| Physiotherapists | 97 | 46 |
| Pharmacists | 66 | 35 |
| Community volunteers | 34 | 94 |
| Documentation of symptoms | ||
| Pain (always/often) | 21 | 65 |
| Psychosocial concerns (always/often) | 4 | 48 |
| Access to opioids* | ||
| RMI status | 0 | 36 |
| Morphine availability (always/often) | 57 | 55 |
| Psychosocial supports | ||
| Bereavement support/follow-up | 36 | 83 |
| Education supports | 4 | 42 |
| Physical rehabilitation | 52 | 53 |
| Vocational support | 2 | 25 |
*RMI able to prescribe/store/dispense oral morphine. Government hospitals are deemed RMIs. Hospitals which are not RMI status can often access morphine by local referral networks. RMIs: Recognized Medical Institutions, PCPs: Palliative care providers, GO: Government, NGO: Non-GO
The annual median number of new patients was 183 (interquartile range [IQR]: 120–273) and 159 (IQR: 78–250) in GO and NGO PCPs, respectively. The median number of home visits was 1398 (IQR: 1065–1680) in GO PCPs and 979 (IQR 369–1300) in NGO PCPs. The median number of outpatient visits was 600 (IQR: 360–867) in GO PCPs and 520 (IQR 132–990) in NGO PCPs.
Clinical team and organizational culture
Members of the clinical team are shown in Figure 2. Physicians were more commonly involved in NGO PCPs compared to GO PCPs (94% [94/100] vs. 40% [40/100], P < 0.001). Only a minority of PCPs had full-time physicians with training in palliative care (21% [21/100] GO and 26% [26/100] NGO). Nurses were involved in virtually all palliative care PCPs (100% [100/100] GO and 97% [97/100] NGO), 90% (177/197) of whom had formal training in palliative care. Social workers were more commonly involved in NGO PCPs compared to GO PCPs (31% [31/100] vs. 10% [10/100], P < 0.001). Conversely, physiotherapists (97% [97/100] vs. 46% [46/100], P < 0.001) and pharmacists (66% [66/100] vs. 35% [35/100], P < 0.001) were more likely to be involved with GO compared to NGO PCPs. Community volunteers were more likely to be involved in NGO than GO PCPs (94% [94/100] vs. 34% [34/100], P < 0.001).
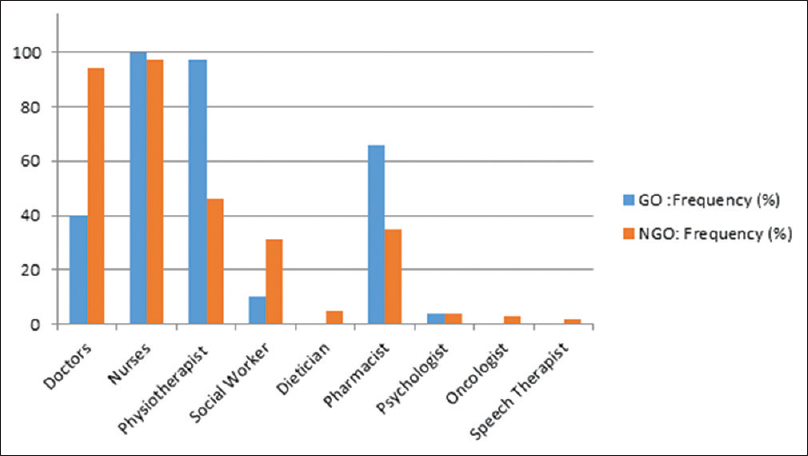
- Availability of health-care professionals among 200 government and nongovernment palliative care palliative care providers in Kerala, India
Regular organizational team meetings were conducted by 100% (100/100) and 96% (96/100) of the GO and NGO PCPs, respectively. Meetings were held on a monthly basis in the GO PCPs; 51% (51/100) and 38% (38/100) of the NGO PCPs reported having regular meetings on a monthly or weekly basis, respectively. Regular clinical meetings were held by 100% (100/100) and 93% (93/100) of the GO and NGO PCPs, respectively; these meetings were usually held on a weekly basis (75% [75/100] of GO PCPs and 71% [71/100] NGO PCPs).
Pain and symptom management
Patient-reported pain was documented “always” or “often” by 21% (21/100) and 65% (65/100) of GO and NGO sites, respectively (P < 0.001). Only 36% (36/100) of the studied NGO and 0% (0/100) of the GO PCPs were able to prescribe and provide oral morphine as RMIs. All GO hospitals are deemed RMIs, but mostly, GO PCPs would refer patients to taluks, districts, and general hospitals as well the Regional Cancer Center in Trivandrum for opioids. Through this referral network or in-house RMI status, only 57% (57/100) and 55% (55/100) of the GO and NGO PCPs reported “always” or “often” having an uninterrupted supply of oral morphine for their patients. Regular and appropriate documentation of opioid use was reported by 5% (5/100) and 57% (57/100) of the GO and NGO PCPs, respectively (P < 0.001).
Psychosocial supports
The frequency of documentation of psychosocial and spiritual issues were reported as “always” or “often” by 4% (4/100) and 48% (47/99) of the GO and NGO PCPs, respectively (P < 0.001). Thirty-six percent (36/100) and 83% (83/100) of the GO and NGO PCPs offered bereavement support and follow-up. Additional (nonmedical) supports offered by palliative care PCPs included education supports (4% [4/100] GO and 42% [42/100] NGO, P < 0.001), physical rehabilitation (52% [52/100] GO and 53% [53/100] NGO, P = 0.887), and vocational support (2% [2/100] GO and 25% [25/100] NGO, P < 0.001). Food kits were also provided by NGOs to those at risk of starvation and in GO system through panchayat.
Barriers, enablers, and outreach
External advocacy (i.e., public awareness initiatives) and external collaborations (i.e., with panchayats, educational institutions, and other NGOs) were more common among NGO PCPs (24%, [24/100] and 43% [43/100] respectively) compared to GO PCPs (1%, [1/100] and 1% [1/100] respectively). Palliative care training programs for clinical staff and community volunteers were offered by 42% (42/100) and 42% (42/100) of the GO and NGO PCPs, respectively.
The most common enablers reported by NGO PCPs were community members (85%, 85/100), community volunteers (65%, 65/100), local shopkeepers (50%, 50/100), and nonresident Indian donors (27%, 20/100). Common barriers reported by palliative care PCPs are shown in Table 2. The most common barriers reported by GO PCPs were inadequate number of volunteers (80%, 80/100), lack of physicians with training in palliative care (79%, 79/100), lack of access to specialist expertise (30%), and difficulty with access to remote areas (23%, 23/100). Common barriers reported by NGO PCPs were lack of adequate funding (70%, 70/100), lack of full-time physicians (50%, 50/100), inadequate number of volunteers (46%, 46/100), inadequate supply of medicines (40%, 40/100), lack of permanent building (30%, 30/100), and difficulty with access to remote areas (29%, 29/100).
| GO PCPs (n=100) (%) |
| Lack of volunteers (80) |
| Lack of physicians with training in palliative care (79) |
| Lack of access to specialist expertise (30) |
| Difficulty with access to remote areas (23) |
| NGO PCPs (n=100) (%) |
| Lack of adequate funding (70) |
| Lack of permanent physicians (50) |
| Lack of volunteers (46) |
| Lack of medicines (40) |
| Lack of permanent building (30) |
| Difficulty with access to remote areas (29) |
PCPs: Palliative care providers, GO: Government, NGO: Non-GO
DISCUSSION
In this study, we describe organizational structure and delivery of clinical services by 200 palliative care PCPs in Kerala. Several important findings have emerged. First, during 2008–2013, there was a substantial expansion in the number of GO palliative care PCPs; there had not been further expansion since that time. Second, the majority of palliative care services were delivered via home visits, with a substantial proportion of care also delivered in outpatient clinics. Third, only a minority of PCPs had a full-time physician with training in palliative care. Fourth, the availability of supporting staff varied substantially between GO PCPs (who were more likely to have physiotherapists) and NGO PCPs (who were more likely to have social workers). Community volunteers were involved in almost all NGO PCPs but only one-third of GO PCPs. Fifth, there were substantial gaps in the documentation of patient-reported pain and psychosocial concerns; this is most pronounced in the GO PCPs. Sixth, none of the GO PCPs and only one-third of NGO PCPs were able to prescribe or provide oral morphine. Finally, commonly reported barriers to the effective delivery of care included lack of physicians with training in palliative care (GO and NGO), lack of funding (NGO), lack of volunteers (GO and NGO), and lack of medicines (NGO).
It is worth considering our study results in the context of the existing literature. In 2008 Pallium India undertook an on-line audit of 49 PCPs throughout India.[5] The primary objective of the 2008 study was to explore the extent to which these PCPs met preexisting standards deemed “essential” for care. There are notable differences between the 2008 study and the current report. First, the older study included only 49 PCPs from across India, while the current report included 200 PCPs from only Kerala. The current PCPs are also much larger than the prior report; median home visit and OP visits were 1398 and 600 and 979 and 520 for GO and NGO PCPs, respectively, whereas the median annual case volume of the 2008 PCPs was >750 patients. Second, the proportion of PCPs that “always” met essential palliative care components was far lower in the current study than the report from 2008 [Table 3]. We do not believe that this represents a deterioration in the quality of PCPs over time. It is more likely that the studies sampled different PCPs (i.e., in 2008, most PCPs would have been NGO) and used different methodologies to understand structures and processes (self-report on-line data in 2008 vs. telephone interview in 2018). Nevertheless, the data in Table 3 highlight the fact that there is still much to do in efforts to improve the breadth and quality of palliative care availability in Kerala. Given that Kerala is considered one of the leaders of the palliative care movement in India, it is, therefore, very likely that there are even bigger gaps in standards elsewhere in India.
| PCPs | ||
|---|---|---|
| 2008 study (n=49) (%) | 2018 study (n=200) (%) | |
| Assessment and documentation of pain and other symptoms | 76 | 38 |
| Assessment and documentation of psychosocial and spiritual issues | 76 | 23 |
| An uninterrupted supply of oral morphine | 92 | 46 |
| A system for documenting Step 3 opioids | 98 | 33 |
| Physician with palliative care training | 98 | 24 |
| Nurse with palliative care training | 96 | 90 |
| Evidence of community involvement | 78 | 64 |
| Regular team meetings | 57 | 45 |
Our group has recently described temporal and geographic trends in access to opioids in Kerala.[9] While access in Kerala was superior to the rest of India, it was still substantially lower than the estimated need. Kerala's per capita consumption is only less than one-third of the global average and <1% of the UK which is considered a country with optimal utilization.[11] This indicates that pain relief (just one component of palliative care) reaches too few, and most probably, too late. In another report, we described the delivery of clinical care by the NGO TIPS over a 10 year period (2007–2016).[10] This study demonstrated a marked increase in case volumes and a growing burden of cancer.
Our study results should be considered in the light of methodological limitations. Although an effort was taken to ensure wide sampling of both GO and NGO PCPs, the study results may not be representative of all PCPs in Kerala and very likely do not represent PCPs elsewhere in India. Moreover, this study did not include PCPs in Kerala's private sector. As with any self-reported audit, the results may also be prone to reporting bias and measurement error. This is particularly true for some of the questions that are more difficult to quantify such as the level of community engagement and the extent to which psychosocial concerns are addressed. Notable strengths of this study include the very high (100%) participation rate and the fact that these data provide a unique and comprehensive view of palliative care delivery across diverse settings in Kerala.
As with all LMICs, there is a vast need to expand palliative care services across India. Herein lies a challenge for policymakers as they seek to balance access to care (i.e., increasing the number of PCPs) with quality of care (i.e., ensuring that essential palliative care standards are met). With the creation of a standards audit tool Pallium India sought to establish a metric by which all PCPs in India could be evaluated. While the frequency and duration of clinical visits will vary based on patient need, most patients are seen approximately twice/month and clinic/home visits are usually 30–45 min in duration. Building on the 2008 report, the current study highlights important gaps in care that require urgent attention. Although there are eight standards which are deemed essential, we would advise that six of these require the most urgent attention across all PCPs in India. First, given that the central tenet of palliative care is to relieve suffering, it is imperative that PCPs assess and document pain and other symptoms in addition to the psychosocial and spiritual needs of all patients. Second, to provide effective pain relief, it is critical that all PCPs have uninterrupted access to oral morphine either as RMI sites or via local and accessible referral networks. A system for documenting the use of opioids must be an integral part of all PCPs. Finally, while PCPs should strive to provide holistic care with a multidisciplinary team that includes social workers, pharmacists, and physiotherapists, it is essential that all PCPs have a full-time physician and full-time nurse with training in palliative care.
CONCLUSIONS
Kerala has achieved remarkable success in the coverage of palliative care through hundreds of locally active NGOs through GO machinery involving every PHC. While efforts have been made to expand access to palliative care in Kerala, there is an urgent need to improve essential components of high-quality palliative care including the presence of a physician with palliative care training, routine documentation of pain and psychosocial concerns, and uninterrupted availability of oral morphine. Caution is needed against potential challenges to quality care in any new initiative. This study highlights the need for periodic review to identify gaps in care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to acknowledge the 200 palliative care programs across Kerala that willingly participated in this study. The authors are grateful to Mr. K.N. Nair for his assistance in contacting participants. Finally, authors are indebted to the Directorate of Health Services and the IAPC (Kerala Chapter), respectively, for facilitating this project.
REFERENCES
- Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: The lancet commission report. Lancet. 2018;391:1391-454.
- [Google Scholar]
- Provision of palliative care in low-and middle-income countries: Overcoming obstacles for effective treatment delivery. J Clin Oncol. 2016;34:62-8.
- [Google Scholar]
- Hospice and palliative care development in India: A multimethod review of services and experiences. J Pain Symptom Manage. 2008;35:583-93.
- [Google Scholar]
- 2006. Standards Audit Tool for Indian Palliative Care Programs Pallium India. Available from: https://palliumindiaorg/cms/wp-content/uploads/2010/01/Standards-paper-IJPCpdf
- Creation of minimum standard tool for palliative care in India and self-evaluation of palliative care programs using it. Indian J Palliat Care. 2014;20:201-7.
- [Google Scholar]
- 2011. Office of the Registrar General and Census Commissioner India 2011 Census Data Delhi. Available from: http://wwwcensusindiagovin
- 2009. Standard Operating Procedures for approval and Monitoring of Recognised Medical Institutions in Kerala. Available from: https://palliumindiaorg/cms/wp-content/uploads/ 2014/01/Standard-Operating-Procedures-finalpdf
- 2014. List of Modern medicine Institutions Under Directorate of Health Services. Available from: http://wwwdhskeralagovin/docs/orders/combinedpdf
- Oral morphine use in South India: A population-based study. J Glob Oncol. 2017;3:720-7.
- [Google Scholar]
- Palliative care program development in a low-to middle-income country: Delivery of care by a nongovernmental organization in India. J Glob Oncol. 2018;4:1-8.
- [Google Scholar]
- 2013. Global Opioid Consumption Data: Countries University of Wisconsin Pain and Policy Studies Group. Available from: http://wwwpainpolicywiscedu/countryprofiles






