Translate this page into:
Meta-analysis on Effectiveness of Palliative Care versus Conventional Care amongst Advanced Gynaecological Patients with Cancer and Caregivers
*Corresponding author: Dr. Kusum Kumari, Associate Professor, College of Nursing, All India Institute of Medical Sciences, Deoghar, Jharkhand, India. kus2211@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumari K, Kalyani CV, Gupta S, Gupta P, Venkatesan L, Gaur R, et al. Meta-analysis on Effectiveness of Palliative Care versus Conventional Care amongst Advanced Gynaecological Patient with Cancer and Caregivers. Indian J Palliat Care. 2024;30:289-95. doi: 10.25259/IJPC_145_2024
Abstract
In cancer patients, physical and psychological issues are very common. There is a need for family support and high utilisation of healthcare resources commonly. Palliative care (PC) has grown in popularity to better fulfil of needs of patients and their families and potentially lowering hospital costs. Given that the majority of patients still die in hospitals, there is a need for an effective model of PC for advanced gynaecological cancer, as well as the wise allocation of scarce resources. The main aim of this study was to compare the efficacy of PC to conventional treatment for adults with cancer, including gynaecological cancers, and their caregivers. Four randomised controlled trials (RCTs) were identified by searching PubMed, PubMed Central, Clinical Key, Embase and other grey literature from a duration of 2011–2021. Cochrane criteria were used to calculate the risk of bias, and the Grade Profiler Guideline Development Tool was used to check the quality of the included studies. Standardised mean differences (SMDs), I2 value and forest plot were prepared by using Review Manager 4.0. A total of four RCTs were extracted by following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and found to have a high risk for bias and low to poor quality of evidence. Included study sample sizes ranged from 22 to 104 participants, including 670 people in total, including 289 patients with advanced cancer patients, including gynaecological cancer and 381 unpaid caregivers. Results also showed that PC enhances patients’ quality of life (SMD = 0.26; 95% confidence interval [CI] = −0.29–0.80; I2 = 76%), lowered symptom burden amongst patients (SMD = −0.75, 95% CI = −1.75–0.25; I2 = 89%), reduces patient depression (SMD = 0.08, 95% CI = −0.19–0.34; I2 = 0%) and decreases depression in unpaid caregivers (SMD = −0.16, 95% CI = −0.56–0.24; I2 = 59%). PC treatment increases patients’ quality of life and lowers their symptom burden. In comparison to conventional care, it also reduces depression among patients and caregivers. We believe that the findings should be viewed with care until more recent exclusive RCTs are available.
Keywords
Palliative care
Conventional care
Advanced cancer
Gynaecological cancer
Caregivers
INTRODUCTION
Globally, the burden of cancer has increased and put higher stress on the healthcare system. Any advanced cancer patient experiences functional and cognitive impairment continuously after diagnosis, followed by an unpredictable phase of clinical and functional decline. To overcome the complications of cancer, i.e., physical distress, functional dependence, psychological distress and weakness, there is a requirement for family support from months to years to fight against cancer along with the health-care system.[1] The increased incidence of female-aged populations with gynaecological cancer has resulted in significant healthcare costs of 3.8 billion dollars, with an average cost of 6,293 dollars per patient and increased clinical complexity.[2] The World Health Organization (WHO) defined palliative care (PC) to advanced cancer patients as always resulting in increased staff costs, including PC services and specialised PC.[3,4] In developed countries like the United States, specialised PC hospitals had more than and equal to 50 beds, and that increased by 178% between 2000 and 2016, from 25% in 2000 to 75% in 2016.[5,6] One out of every five advanced cancer patients dies in a hospital, and death in institutional care persists into the later stages of life, which always pays a very high amount to any country’s health system and economy, too.[7]
PC includes symptom management and care during the end-of-life phase for almost every cancer, including gynaecological cancer, at hospices, hospitals and at home.[8-10] Studies have shown that PC not only improves treatment quality but also improves clinical outcomes for all cancer patients, including gynaecological cancer.[2,11] Caregivers are the main key support for any cancer patient. PC can be provided by assisting unpaid caregivers or family members as they are family who love and care for their loved ones, and it is also required during the grief and bereavement process.[12] By knowing gynaecological cancer patient’s quality of life and their caregivers, we can generate research evidence and implement their PC in the future. The present study focused on comparing specialist PC with conventional care for patients who have advanced gynaecological cancer and their caregivers.
MATERIALS AND METHODS
Four randomised controlled trials (RCTs) were included for comparison of PC versus conventional care on quality of life, burden and depression level of cancer patients and their caregivers, including gynaecological cancer. All studies looking for primary or secondary outcomes of gynaecological cancer were eligible.
Participants were patients who were diagnosed with advanced cancer, received specialist PC and had a compromised quality of life were included. Unpaid caregivers were family members or significant others, and those who received a pre-bereavement intervention from specialist PC staff to manage bereavement-related problems were included.
We decided to include studies in which patients get PC intervention provided in hospitals, hospices and home settings by a PC team. Unpaid caregivers were adults and patients’ family members or significant others who were receiving hospital inpatient, outpatient or outreach PC services and received intervention. We considered trials that compared PC to standard treatment. Trials excluded research in which PC was provided by only PC practitioners (pain management and oxygen therapy) because that did not consider holistic PC.
Outcome measures were primary as well as secondary outcomes were derived from previous relevant RCTs. Results reflect the multifaceted character of PC, i.e., patients received direct and indirect patient care, and caregivers received care, too. Primary outcomes were patients’ health-related quality of life and burden of symptoms, as the primary goal of PC. Quality of life was measured by health-related quality of life scales, and the burden of symptoms was the collection of two or more symptoms that include social, physical, spiritual and psychological domains as reported by patients using any validated scale. The secondary outcomes were patient and caregiver depression was assessed with validated depression assessment scales as secondary outcomes.
The search strategy used in this study was electronic searches (PubMed [n = 20], PubMed Central [n = 22], Clinical Key [n = 02] and Embase [n = 02]) and other grey literature searches were used to find RCTs. Only the English language is restricted, and research from 2011 to 2021 was included. By utilising electronic searches and using MeSH terms, we found four relevant papers.
Included studies titles and abstracts found in our electronic searches were independently examined by two authors (CVK and KKR). If there was any ambiguity about the study’s eligibility after reading the abstract, we retrieved full-text RCTs for further evaluation, and two authors (PG and VL) reviewed those articles again. Cochrane Handbook for Systematic Reviews of Interventions were followed and used Preferred Reporting Items for Systematic Reviews and Meta-analyses[13] (Higgins 2011a) guidelines to resolve disagreements by discussion [Figure 1].
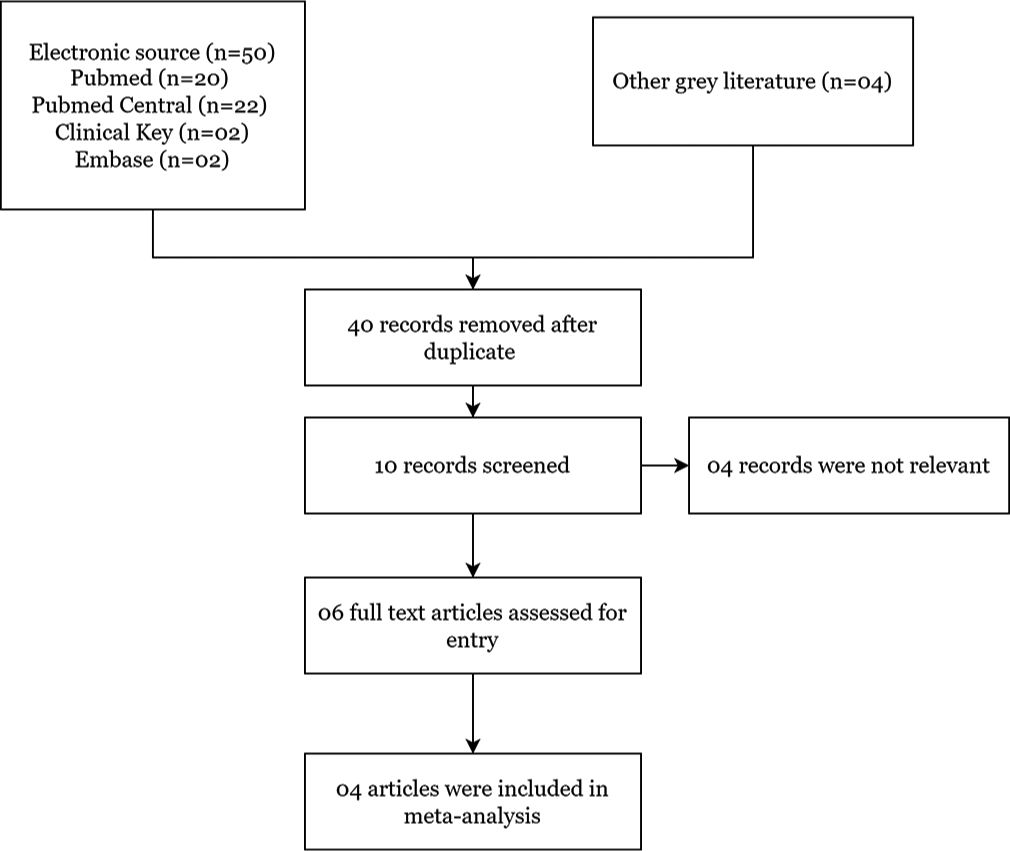
- Diagram of meta-analysis following preferred reporting items for systematic reviews and meta-analyses guidelines.
Extraction and management of data done by two authors (CVK and KKR) extracted relevant data from RCTs using a data extraction form. Review Manager (RevMan 4.0) was used to enter data (RevMan 2014). The data extraction form was previously used in a study and again assessed for its efficacy. We gathered enough information about the included studies to create an ‘Included Studies Characteristics’ list [Table 1]. Included studies’ risk of bias done by following Cochrane criteria, two reviewers (CVK and KKR) assessed the risk of bias by following the risk of bias assessment tool and creating a risk of bias graph and risk of bias summary for the included study [Figures 2 and 3].
| Author | Intervention | Sample size (intervention/control) | Life expectancy | Outcome | Certainty of evidence (GRADE) |
|---|---|---|---|---|---|
| Tattersall et al. (2014) [14] | Nurse-led intervention | 60/60 | Life expectancy of <12 months | MQoL questionnaire; RSC checklist; SCNS-Short Form Questionnaire | Low |
| Ozcelik et al. (2014) [15] | Multidisciplinary team | 22/22 | Life expectancy from 6 and 12 months | ESAS Assessment System; EORTCQLQ-C30 Quality of Life Questionnaire; FAMCARE questionnaire | Very low |
| McCorkle et al. (2015) [16] | Multidisciplinary team | 66/80 | Late-stage cancer diagnosis within 100 days |
SDS Scale; PHQ-9 Questionnaire; ESDS Scale; SF-12 | Low |
| Bakitas et al. (2015) [17] | Multidisciplinary team | 104/103 | Prognosis of 6–24 months | FACIT-Pal Index; End-of-life symptom impact scale; Epidemiological Studies Depression | Low |
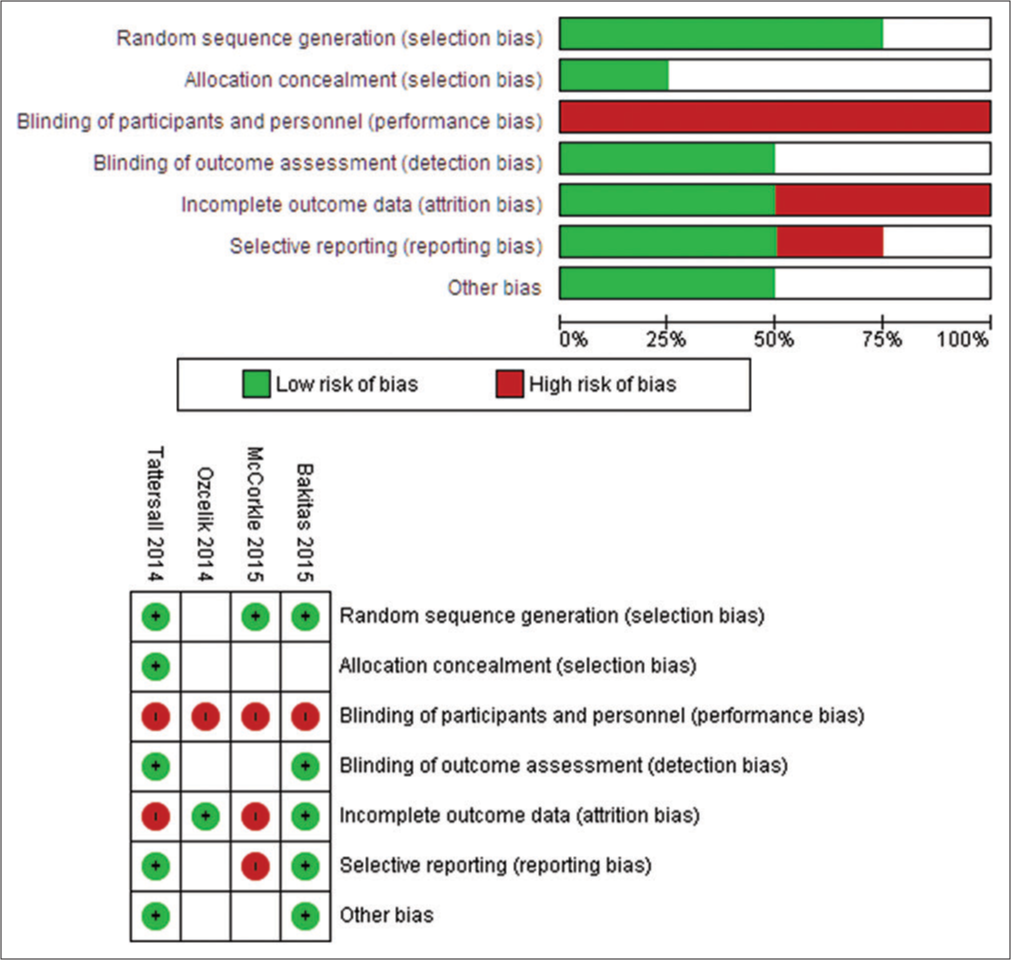
- Graph showing risk of bias and risk of bias summary.
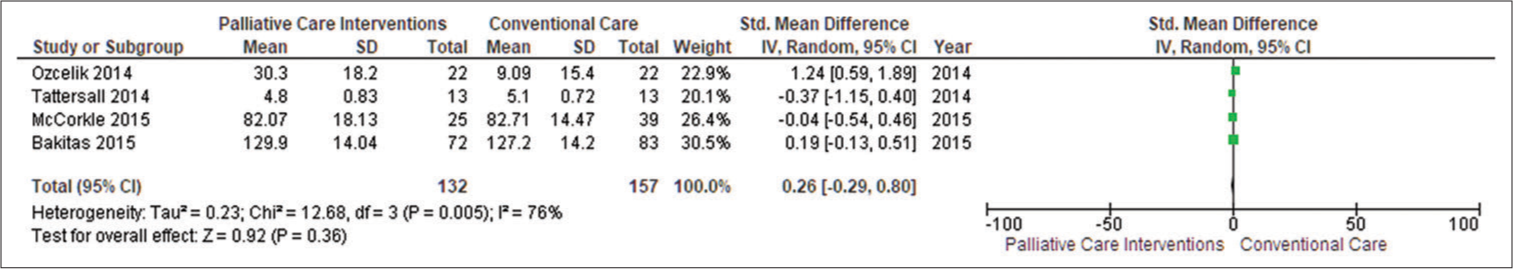
- Forest plot of patient’s quality of life. SD: Standard deviation, CI: Confidence interval.
Assessment of heterogeneity amongst four included studies was inspected for checking heterogeneity based on the findings of our meta-analysis, i.e., inspection of forest plots and use of I2 statistics for assessing the extent of heterogeneity (Higgins 2011a). Data synthesis was done by including means, standard deviations and frequencies of the included study and tabulated to provide the main elements of included studies that were eligible for meta-analysis (Rodgers 2009). Evidence of high quality of included studies’ outcomes was judged by two authors (CVK and KKR) independently using Grade Profiler Guideline Development Tool (GRADE pro-GDT 2015) software and the Cochrane Handbook for Systematic Reviews of Intervention criteria. The GRADE method assessed the quality of the body of evidence for each included study outcome using five criteria (publication bias, consistency of effect, study limitations, imprecision and indirectness) (Higgins 2011a). The grading system assigns grades to high to very low evidence based on their criteria [Table 1].
RESULTS
We included 50 studies searched by records retrieved from various electronic searching databases and four additional records from other grey sources. By removing duplicate studies by two authors (CVK and KKR), four studies were finally included [Figure 1]. The design of all four included RCTs were comprised of one fast-track RCT, one cluster RCT and two studies that had parallel design. Sample sizes ranged from 22 to 104 participants. Total recruitment time in RCTs ranges from 1 month to 12 months. We used data from 670 people in total, including 289 adults with advanced cancer patients, including gynaecological cancer and 381 unpaid caregivers.
Advanced cancer patient participants, including gynaecological cancer and their unpaid caregivers/family members, were subjects of four included studies (Tattersall et al., 2014,[14] Ozcelik et al., 2014; [15] McCorkle et al., 2015,[16] and Bakitas et al., 2015[17]). The average age of cancer patients ranged from 34.2 to 62.2 years. Four studies were included, each with the same number of male and female patients.
We included four studies, in which one study (Bakitas et al., 2015)[17] provides palliative services intervention based on the telephone for rural populations, another outpatient service (Tattersall et al., 2014)[14], an inpatient consultation (Ozcelik et al., 2014)[15] and a service provided across various settings, including hospital (McCokle 2015). One study (Bakitas et al., 2015)[17] included an advanced PC team including PC clinicians and nurse specialists, while the other three studies stated that professionals who delivered specialist-level interventions were involved (Tattersall et al., 2014; Ozcelik et al., 2014; McCorkle et al., 2015).[14-16] In 3 studies, early PC was included (Tattersall et al., 2014; Ozcelik et al., 2014; McCorkle et al., 2015).[14-16] In one study, patients with advanced cancer were diagnosed between 30 and 60 days before (Bakitas et al., 2015).[17] One study (McCorkle et al., 2015)[16] looked at patients who had been diagnosed with advanced-stage cancer within the previous 100 days. In one study, ambulatory patients with newly diagnosed metastatic cancer were included (Tattersall et al., 2014).[14] Theoretically grounded: Case conference/management was included in one study, i.e., Ozcelik et al. 2014.[15] PC participated in two studies (Ozcelik et al., 2014; Bakitas et al., 2015)[15,17] that provided unpaid caregiver/family assistance and provided counselling to assist patients and unpaid caregiver/family members. One study was only focused on the patient (Ozcelik et al., 2014)[15], while the other three were focused on both the patient and the family (Tattersall et al., 2014; McCorkle et al., 2015 and Bakitas et al., 2015).[14,16,17] We included care coordination as a new category since the need for coordinated care with advanced disease is not always met, leading to more hospitalisations and poor clinical outcomes. The results of PC were compared with the control group by following conventional care. RCTs showed a poor description of conventional care, with very little information supplied. The control group in Bakitas et al. 2015 trial was kept under specialist care, including PC physicians, nurse specialists, physiotherapists and other treatment services. Inpatient palliative treatment was also available to all patients as needed. After 4 weeks, observation was done for the control group. In the remaining three studies, standard care was included, and engagement of PC professionals was done if needed (Tattersall et al., 2014; Ozcelik et al., 2014; McCorkle et al., 2015).[14-16]
Out of the four included studies, the key outcomes were health-related quality of life (Tattersall et al., 2014; Ozcelik et al., 2014; McCorkle et al., 2015; Bakitas et al., 2015)[14-17] and symptom burden (Tattersall et al., 2014, Ozcelik et al., 2014, McCorkle et al., 2015, Bakitas et al., 2015).[14-17] All four studies included early PC and reported symptom burden in cancer populations, including gynaecological cancer (Tattersall et al., 2014; Ozcelik et al., 2014; McCorkle et al., 2015; Bakitas et al., 2015).[14-17] Depression was also reported in two studies among patients (McCorkle et al., 2015; Bakitas et al., 2015)[16,17] and their caregivers (Ozcelik et al., 2014; Bakitas et al., 2015)[15,17] [Figure 2].
We excluded four studies because one was not RCT, one RCT followed PC as routine care, one RCT did not follow sequence allocation, and one RCT intervention was not given by the PC team. Risk of bias in included studies was done using the Cochrane risk-of-bias tool (Higgins 2011b), i.e., selection, performance, detection, attrition, reporting and other biases were all identified and reported and found high risk for bias for included studies.
Primary outcome
Patient’s health-related quality of life
Four studies included quality of life with adjusted endpoints (Ozcelik et al., 2014; Tattersall et al., 2014; McCorkle et al., 2015; Bakitas et al., 2015).[14-17] PC was found helpful in enhancing patient’s quality of life (standardised mean differences [SMD] = 0.26; 95% confidence interval [CI] −0.29–0.80; I2 = 76%) when data from four studies reporting endpoint data with 289 patients were pooled where positive SMDs imply that higher level of patient’s quality of life.
According to traditional standards, the effect size obtained (0.92) is high (Cohen 1988). By computing SMDs across RCTs in meta-analyses, we were able to combine diverse scales for assessing patient health-related quality of life. The funnel plot revealed some symmetry in general. Egger’s asymmetry test yielded a P = 0.36. This symmetry is not indicative of any publishing bias, as evidenced by the publication of positive research in the funnel plot [Figure 3].
Patient’s symptom burden
We extracted data from four studies (Tattersall et al., 2014; Ozcelik et al., 2014; McCorkle et al., 2015; Bakitas et al., 2015).[14-17] SMDs demonstrated that PC was beneficial in reducing patients’ symptom burden (SMD −0.75, CI −1.75–0.25; I2 = 89%). Negative SMDs suggest benefits, i.e., lower symptom burden faced by patients in PC intervention. The funnel plot revealed symmetry in general. Egger’s asymmetry test yielded a P = 0.14. This symmetry is indicative of no publishing bias, as evidenced by the publication of positive research in the funnel plot. Due to high heterogeneity (I2 = 89%) in our main meta-analysis, we performed subgroup analysis, too [Figure 4].
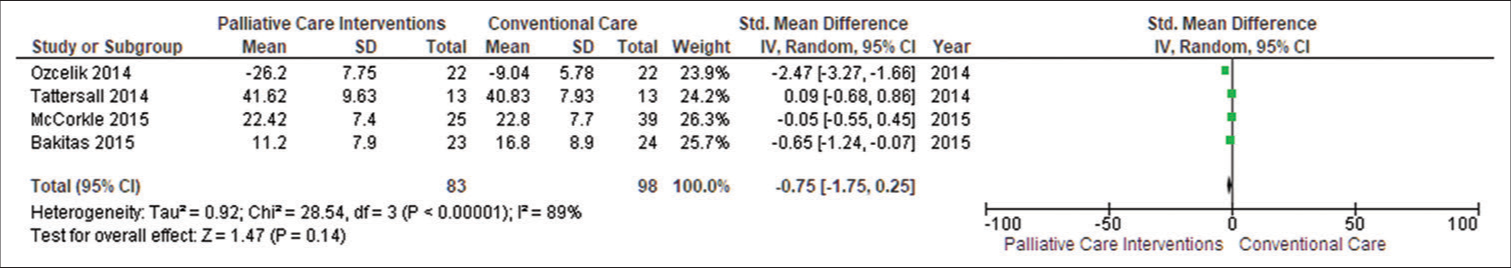
- Forest plot of patient symptom burden. SD: Standard deviation, CI: Confidence interval.
Secondary outcome
Patient’s depression
We included data from two studies (McCorkle et al., 2015; Bakitas et al., 2015)[16,17], and SMDs demonstrated that PC was beneficial in reducing patient depression (SMD 0.08, CI −0.19–0.34; I2 = 0%). Positive SMDs imply increased patient depression, indicating that patients were under mild depression. The funnel plot revealed some symmetry in general. Egger’s asymmetry test yielded a P = 0.57. This symmetry is indicative of no publishing bias, as evidenced by the publication of positive research in the funnel plot with low heterogeneity (I2 = 0%) [Figure 5].
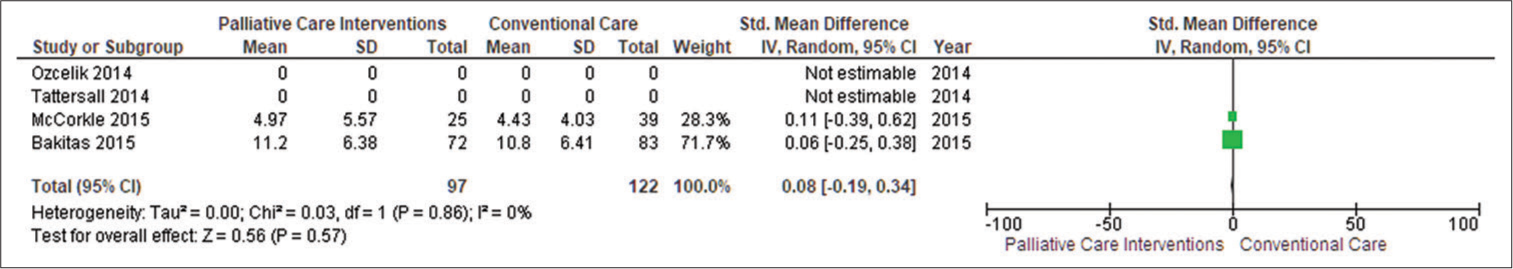
- Forest plot of patient depression. SD: Standard deviation, CI: Confidence interval.
Caregiver’s depression
Two studies (n = 381) reported caregivers’ depression, and they discovered that PC did not affect caregivers’ depression (SMD −0.16, 95% CI −0.56–0.24; I2 = 59%). Negative SMDs indicate benefit, i.e., unpaid caregivers who were receiving PC intervention had lower depression as compared to the conventional care group. The funnel plot revealed some symmetry in general. Egger’s asymmetry test yielded a P = 0.44. This symmetry is indicative of no publishing bias, as evidenced by the publication of positive research in the funnel plot. Sensitivity analysis yielded an SMD of −0.16 (95% CI −0.56–0.24; I2 = 59%; n = 2 studies; n = 381 individuals) [Figure 6].
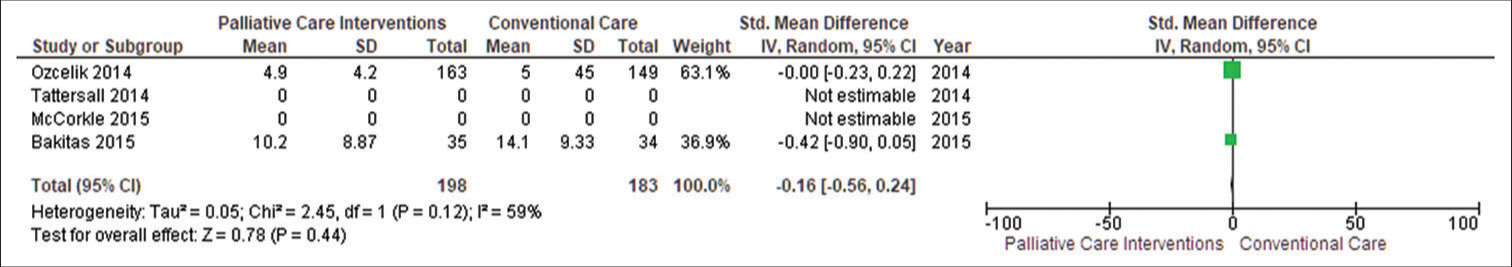
- Forest plot of unpaid caregiver burden. SD: Standard deviation, CI: Confidence interval.
Information given by PC intervention was valuable to patients and caregivers/families since it ensured awareness of illness and treatment alternatives too. The PC team’s diverse nature and specialised knowledge were valued by patients and caregivers/families, and integrating PC with oncology resulted in improved patient care.
DISCUSSION
Significant healthcare costs have been incurred due to a rise in the incidence of gynaecological cancer in older female populations. The main results summary showed that evidence for advanced cancer patients, including gynaecological cancer, is of low to poor quality. It further demonstrated minimal benefits for patients’ quality of life and burden of symptoms. Comparing PC with conventional care, PC improves patients’ quality of life, as evident from positive SMD values. When PC symptom burden was compared with conventional care, the results showed negative SMD values, which suggested its benefit, i.e., PC is also helpful in lowering symptom burden amongst patients. RCT results suggested that PC reduces patient depression on average. Evidence also suggests that PC decreases depression in unpaid caregivers through PC intervention.
Symptom management, coping and support were a key component of PC addressed in the research.[18] Care coordination and future planning were also addressed in several of the studies. Certified PC experts were included in the included RCTs, but they were unsure about the PC training of those providing PC team members for symptom control, care coordination, coping and support.[19]
The transition from a hospital to a home-based care feature was also very challenging and inconsistent. Health policy, PC and resources in developed countries differ from those in developing countries, where PC is still in its early stages (WHO 2014).[20] The findings from developing countries’ healthcare systems may not be applicable to developing countries’ environments. The included papers were related to all cancer patients, but this study revealed that the PC of gynaecological cancer still needs to be revealed more.[21]
In certain ways, this review agrees with previous reviews, particularly in terms of health-related quality of life. With small effect sizes, we discovered that PC improves patient health-related quality of life by reducing symptom burden and decreasing patient and caregiver depression.[11] We also discovered that PC improved some of the secondary outcomes we looked at, i.e., patient depression level. Evidenced quality ranged from very low to low level. Another meta-analysis (Gaertner et al. 2017)[22] also identified the effect of PC on health-related quality of life (SMD 0.16 with moderate-quality evidence).
Potential risk of bias
Given that subjective decisions may influence decisions made during meta-analysis, it is critical to address any potential biases that have occurred. In general, meta-analysis procedures promote transparency and standardisation, improving the process’s reproducibility. We merged RCTs reporting adjusted endpoint data because these studies employed various scales and combined their SMDs for meta-analysis outcomes such as patient’s quality of life, burden of symptoms and depression amongst patients and unpaid caregivers. Pooled studies were lower, which again limited our major meta-analysis findings.
Implications for practice
According to low to very low-quality evidence, advanced cancer patients may benefit from PC in terms of small improvements in quality of life, less burden of symptoms and reduced patient and caregiver depression levels. There was no evidence that PC caused significant harm, and included RCT evidence was poor quality and insufficient to form a firm judgement. Cancer patients can talk to their physicians and ask for a referral to a PC unit. Population-based forecasts show that in the future, PC requirements will rise (May et al., 2019) [23] so policymakers must focus their efforts on expanding PC commissions.
CONCLUSION
PC improves cancer patients’ quality of life and reduces their burden of symptoms. It also reduces depression among patients and their caregivers as compared to conventional care. PC assists cancer patients in dying at the place of their choice (home death), including gynaecological cancer. We believe that until more recent exclusive RCTs are available, the findings should be interpreted with caution. Evidence of PC’s influence on major harms was found to be of very low quality. PC appears to have cost no more than standard care.
Ethical approval
Institutional Review Board approval is not required. This meta-analysis was registered in Prospero number CRD42022299063
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Challenges Faced by Caregivers of Patients with Cancer in the Sub-Himalayan Region: An Exploratory Survey. Cancer Res Stat Treat. 2022;5:220-5.
- [CrossRef] [Google Scholar]
- HealthCare-Related Quality of Life and Lived Existential Experiences among Young Adults Diagnosed with Cancer: A Mixed-Method Study. Indian J Palliat Care. 2020;26:19-23.
- [CrossRef] [PubMed] [Google Scholar]
- A Systematic Review of the Use of the Electronic Health Record for Patient Identification, Communication, and Clinical Support in Palliative Care. JAMIA Open. 2018;1:294-303.
- [CrossRef] [PubMed] [Google Scholar]
- Does a Hospital Palliative Care Team Have the Potential to Reduce the Cost of a Terminal Hospitalization? A Retrospective Case-Control Study in a Czech Tertiary University Hospital. J Palliat Med. 2022;25:1088-94.
- [CrossRef] [PubMed] [Google Scholar]
- The Effectiveness and Cost-effectiveness of Hospital-based Specialist Palliative Care for Adults with Advanced Illness and their Caregivers. Cochrane Database Syst Rev. 2020;9:CD012780.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of Life of People with Cancer in the Era of the COVID-19 Pandemic in India: A Systematic Review. Clin Pract Epidemiol Ment Health. 2021;17:280-6.
- [CrossRef] [PubMed] [Google Scholar]
- Social Relationships and Health: A Flashpoint for Health Policy. J Health Soc Behav. 2010;51:S54-66.
- [CrossRef] [PubMed] [Google Scholar]
- Pain and Symptom Management in Palliative Care and at End of Life. Nurs Outlook. 2012;60:357-64.
- [CrossRef] [PubMed] [Google Scholar]
- How Many People will Need Palliative Care in 2040? Past Trends, Future Projections and Implications for Services. BMC Med. 2017;15:102.
- [CrossRef] [PubMed] [Google Scholar]
- Identification of Factors Influencing Delayed Presentation of Cancer Patients. Int J Community Med Public Health. 2020;7:1705-10.
- [CrossRef] [Google Scholar]
- Reducing Hospital Readmission Rates: Current Strategies and Future Directions. Annu Rev Med. 2014;65:471-85.
- [CrossRef] [PubMed] [Google Scholar]
- Family Caregiving for Persons with Heart Failure at the Intersection of Heart Failure and Palliative Care: A State-of-the-Science Review. Heart Fail Rev. 2017;22:543-57.
- [CrossRef] [PubMed] [Google Scholar]
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097.
- [CrossRef] [PubMed] [Google Scholar]
- Early Contact with Palliative Care Services: A Randomized Trial in Patients with Newly Detected Incurable Metastatic Cancer. J Palliat Care Med. 2014;4:170.
- [CrossRef] [Google Scholar]
- Examining the Effect of the Case Management Model on Patient Results in the Palliative Care of Patients With Cancer. Am J Hosp Palliat Care. 2014;31:655-64.
- [CrossRef] [PubMed] [Google Scholar]
- An Advanced Practice Nurse Coordinated Multidisciplinary Intervention for Patients with Late-Stage Cancer: A Cluster Randomized Trial. J Palliat Med. 2015;18:962-9.
- [CrossRef] [PubMed] [Google Scholar]
- Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. J Clin Oncol. 2015;33:1438-45.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care and Symptom Management in Older Patients with Cancer. Clin Geriatr Med. 2016;32:45-62.
- [CrossRef] [PubMed] [Google Scholar]
- The Impact of the Advanced Practice Nursing Role on Quality of Care, Clinical Outcomes, Patient Satisfaction, and Cost in the Emergency and Critical Care Settings: A Systematic Review. Hum Resour Health. 2017;15:63.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to Access to Palliative Care. Palliat Care. 2017;10 Doi: 10.1177/1178224216688887
- [CrossRef] [PubMed] [Google Scholar]
- Family-Centered Primary Care for Older Adults with Cognitive Impairment. Contemp Fam Ther. 2022;44:67-87.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Specialist Palliative Care Services on Quality of Life in Adults with Advanced Incurable Illness in Hospital, Hospice, or Community Settings: Systematic Review and Meta-Analysis. BMJ. 2017;357:j2925.
- [CrossRef] [PubMed] [Google Scholar]
- Population-Based Palliative Care Planning in Ireland: How Many People Will Live and Die with Serious Illness to 2046? HRB Open Res. 2019;2:35.
- [CrossRef] [PubMed] [Google Scholar]






