Translate this page into:
Metastatic Primary Duodenal Adeno-Carcinoma Responding to Metronomic Oral Cyclophosphamide Chemotherapy
Address for correspondence: Dr. Anis Bandyopadhyay; E-mail: anish_b123@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary adenocarcinoma of duodenum is a very rare tumour with a prevalence of only 0.3 to 1% of among all the tumours of gastrointestinal tracts. Localised tumours, if resected have good prognosis but those with metastates entails a poor prognosis, where generally palliation may be the only feasible option. Low dose continous cytotoxic treatment or metronomic chemotherapy prevents neoangiogenesis and chemoresistance thereby, provides excellent symptom relief and palliation in many advanced heavily pretreated solid malignancies. It offers as an affordable, less toxic therapy with moderate to good efficacy. Here we report a case of a 52 year female who, presented with history of maleana, pallor and pedal edema for last 2 months. Her performance status was poor (KPS 40) and she had enlarged left supraclavicular lymph node, palpable liver and vague mass in paraumbilical region. Upper GI endoscopy revealed large ulceroproliferative growth in the D2 segment and HPE showed moderately differentiated adenocarcinoma. CT scan revealed paratracheal and retroperitoneal lymphadenopathy and bone scan revealed vertebral metastasis. Patient received oral cyclophosphamide and hematinic and vitamin support, along with radiation to spine. There was near complete clinical response, and progression free period of about 32 weeks. Thus, single agent cyclophosphamide in the present case provided near total clinical response and prolonged period of freedom from disease progression with excellent palliation of symptoms. Hence in patient of advanced and metastatic small bowel cancer, with poor performance status metronomic therapy with single agent cyclophosphamide may provide viable option both for treatment and palliation.
Keywords
Cyclophosphamide
Duodenal adenocarcinoma
Metronomic chemotherapy
BACKGROUND
Primary adenocarcinoma of duodenum is a rare tumour, constituting 0.3-1% of all gastroinstestinal tumours with second part being the most common site of involvement[12]. Resection is the primary treatment for localized disease, with unresectable tumor having poorer prognosis than resectable ones.[3] Metastatic primary adenocarcinoma of duodenum has grave prognosis with very little treatment options other than palliation[4]. Metronomic chemotherapy is an option in such palliative settings of various cancers because of its low cost and low toxicity with good efficacy. Oral daily Cyclophosphamide has shown to have promising activity in heavily pretreated advanced carcinomas and is in use for more than 10 years.[5] Here we report a case of primary adenocarcinoma of duodenum presenting with liver, lung, supraclavicular lymph node and intraabdominal metastases treated with primary metronomic chemotherapy of oral cyclophosphamide with achievement of near complete response and more than seven months of progression free survival.
CASE REPORT
A 52-year-old lady presented with pain and dragging sensation in the abdomen and generalized weakness and fatigue for last 4 months. She also reported few episodes of melaena. The lady had past history of Total Abdominal Hysterectomy plus Bilateral Salphingo-oopherectomy 3 years back and open cholecystectomy 18 months prior to presentation with the above symptoms. There was no history peptic ulcer disease or tuberculosis. On examination the patient's general condition was poor, with Karnofsky's performance status of about 40. She was pale and had bilateral pedal edema. Her face was flushed and she was dyspnoeic, with tachycardia and pounding pulse. There was a hard, nontender enlarged left supraclavicular lymph node, 3 × 3 cm in dimension, fixed to the underlying structures. The chest findings were unremarkable except for tachypnea. On abdominal examination there was mild hepatomegaly and a vague mass in the right loin/paraumblical region.
Her routine blood examinations showed severe anemia, Haemoglobin 5.9 gm%, hypochromic microcytic, total and differential leukocyte count was within normal limits. The plasma random glucose was 117 mg/dl, the serum Urea and creatinine was 42 mg/dl and 0.6 mg/dl, respectively. The liver function was within normal limits. Ultrasonography of abdomen revealed a large ill-marginated heterogeneous mass lesion (11.2 × 5.1) adherent to right kidney, causing hydronephrosis of right kidney as well as causing right renal vein and IVC thrombus with extension within the retoperitoneum in close proximity to aorta. There were also multiple echogenic space occupying lesions (SOLs) within the liver, suggesting secondaries to liver. Upper GI endoscopy showed a large ulceroproliferative lesion in the D2 segment of duodenum with fresh blood in D1 and altered blood in the stomach [Figure 1]. There were no-other mucosal abnormality in the esophagus, stomach and other segments of duodenum. A biopsy from the ulceroproliferative growth revealed histopathological features of a moderately differentiated adenocarcinoma with overlying ulcerated and necrosed surface epithelium [Figure 2].
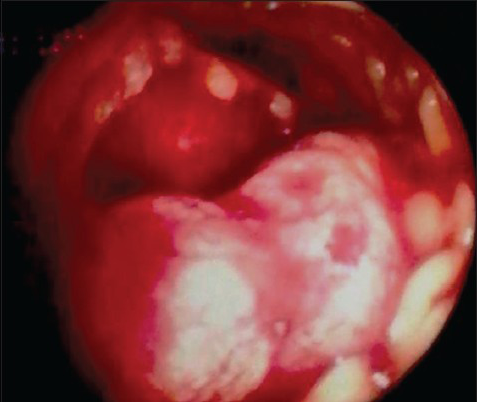
- Endoscopic view of the ulceroproliferative lesion in the D2 segment of duodenum
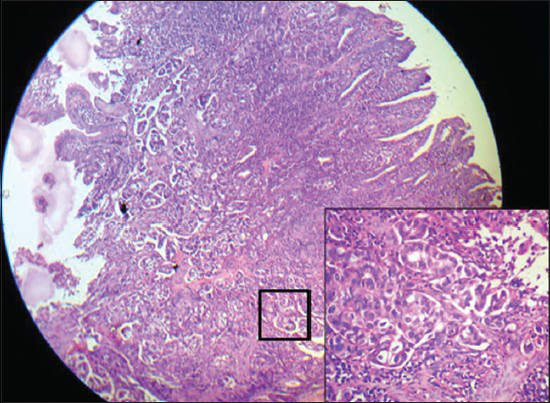
- Duodenal biopsy: low power (×100) showing infiltrative malignant glands with overlying necrotic epithelium. (Inset box, ×400) Shows glandular structures lined by malignant cells
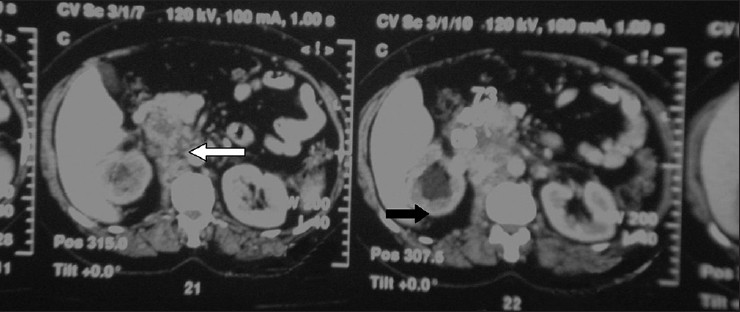
- Computed tomography sections showing a heterogeneous retropritoneal mass (white arrow), of size 7.8 × 7 cm, with irregular calcification was seen centrally and right paramedian plane in the prevertebral region, encasing major vessels, right ureter and causing obstructive hydronephrosis on the right side (black arrow)
A computed tomography (CT) evaluation of thorax and abdomen revealed a large (3.2 × 3 cm) SOL in the left paratracheal region at the root of the neck, suggestive of a nodal mass, along with few other superior mediastinal nodes. An irregular heterogeneous retropritoneal mass, of size 7.8 × 7 cm, with irregular calcification was seen centrally and right paramedian plane in the prevertebral region, encasing major vessels, right ureter and causing obstructive hydronephrosis on the right side [Figure 3]. The mass was in close contiguity with right renal hilum and psoas muscle. There was also presence of a solitary sizable nodule (2.2 × 2.5) in the upper lobe of left lung, suggestive of secondary along with few scattered rounded hypodense lesions in the both lobes of liver.
A whole body bone scan showed abnormal focal spots of activity in the 9th, 11th and 12th ribs with cortical expansion of ribs along with abnormal uptake in the L2 and L3 vertebrae. X-ray of LS spine showed osteophytic changes in the anterior aspect of lumbar vertebrae with reduced disc space of L3-L4 vertebrae. The patient received palliative radiation of 8 Gy/single fraction to the lumbar vertebrae (L1-L4) by 6 MV photon with significant pain relief. She was also put on i.v. bisphosphonate; zoledronic acid 4 mg i.v. every 4 weeks.
Based on above clinical, pathological and radiological findings, a diagnosis of metastatic duodenal adenocarcinoma with metastases to bone, liver, lung and lymph node was made. She was not offered any radical chemotherapy due her low performance status. She received four units of packed red blood cell (PRB) transfusion and was started on oral metronomic chemotherapy of cyclophosphamide 50 mg daily. She also received a multivitamin and heamatinics. After 2 weeks of therapy the symptoms started to improve significantly and clinical evaluation at 12 weeks clinically showed a complete response of supraclavicular lymphadenopathy, the abdominal mass and chest symptoms. Computed tomography (CT) evaluation of abdomen and thorax at 15 weeks revealed complete response of disease in the abdomen and chest, with near complete response of the hepatic lesions (decreased size of hepatic hypodense mass: 1 × 1 cm). An upper GI endoscopy showed no lesion in stomach and D1, and a small nodular lesion in D2 without mucosal break. The patient remained asymptomatic on metronomic cyclosphosphamide till 32 weeks of therapy after which she presented with respiratory distress. On examination and on skiagram of chest, left sided moderate pleural effusion was detected. She underwent palliative thoracocentesis for symptom relief. A repeat CT scan of thorax and abdomen revealed no parenchymal lesion in the thorax or nodes in the abdomen, and the hepatic SOLs were found to be reduced in size. She was put on second-line chemotherapy of oral capecetabine, 500 mg daily and was having progessive disease after receiving 3 months of the same.
DISCUSSION
Primary duodenal adenocarcinoma is a rare tumor of the small bowel and a separate entity in itself, which is often clubbed with periampullary carcinomas.[3] They mostly present with epigastric pain, nausea and vomiting, weight loss and signs of upper gastrointestinal bleeding. Commonly arising from D2, these tumors when localized, are usually treated by surgery (pancreatoduodenectomy, most commonly) with good prognosis (5 yr survival as high as 75%).[14] The presence of lymph node involvement and especially distant metastases are associated with worse prognosis.[1] There is very little literature on the role of adjuvant or systemic chemotherapy in metastatic duodenal adenocarcinoma. Various chemotherapy schedules have been tried in small bowel adenocarcinomas and specially duodenal adenocarcinomas. Overman reported the role of the combination of 5-FU and a platinum based agent in 80 patients with metastatic small bowel adenocarcinomas (of which 30 were duodenal adenocarcinomas) in producing higher response rate and PFS compared with other chemotherapy regimes.[6] In another phase II study, FAM (5 FU, Doxorubicin and Mitomycin C) regimen was found active in metastatic small bowel adenocarcinoma though, the response was not significantly better than other regimens.[7] The role of radiation is also not well defined.
Metronomic chemotherapy involves continuous administering of low dose oral cytotoxic drugs over a prolonged period with an aim of tumor control through overcoming chemoresistance and inhibiting neoangiogenesis.[8] These cytotoxic agent acts on the endothelial cells of the tumor vasculature rather than the tumor cells itself. Anti-angiogenesis is achieved by various mechanisms like selective inhibition of proliferation and/or induction of apoptosis of activated endothelial cells, blockade of circulating endothelial progenitor cells (CEPs) and suppression of HIF-1a expression.[9] The various drugs used with substantial clinical effects are oral cyclophosphamide, capecetabine, methotrexate, etoposide, vinorelbine etc.[1011121314] This strategy has some definite advantages over conventional pulsed course chemotherapy like its lesser toxicity profile, better compliance and suitability for patients otherwise not fit for full dose chemotherapy. Metronomic oral cyclophosphamide (Cy) has been extensively studied and widely used for various advanced and metastatic solid tumors with variable results. It is used singly or in combination with various chemotherapeutic and targeted agents for diverse malignancies like metastatic renal cell carcinoma, multiple myeloma, breast, prostate, head and neck and GI malignancies.[10111213] The heterogenecity of chemotherapy combinations used in above studies has made it difficult to objectively evaluate the additional value of the metronomic administration of cyclophosphamide. The combination of cyclophosphamide with celecoxib for heavily pretreated gastrointestinal tumors is found to be feasible, well tolerated and associated with a promising antitumor activity both demonstrated by pharmacodynamic markers and clinical parameters.[14]
The present patient presented with very low performance status and per se was not suitable for any conventional pulse dose chemotherapy. Moreover, her relatives were not willing for any inpatient treatment and wanted palliation only, preferably by oral drugs. Oral capecetabine was an option but its toxicity, cost and twice daily dosing were not accepted by the patient's family. Based on evidence from literature, oral cyclophosphamide in metronomic dose as a single agent provided simpler and cheaper option for this patient and hence was tried. It was well tolerated and produced near complete clinical response and 32 weeks of progression free survival proving both its efficacy and tolerability in widely metastatic small bowel adenocarcinoma and hence merits documentation.
Metronomic chemotherapy, especially oral low-dose metronomic therapy, has the distinct advantage of continuing and sustaining therapy in a home or hospice-based palliative setting as it needs very little admission due to nil or minimal acute toxicity, over conventional pulse palliative chemotherapy. Monthly monitoring of blood parameters and clinical assessment at monthly or bimonthly interval could suffice. The only toxicity the above patient experienced was mild dysuria, however, on cystoscopy revealed no obvious abnormality. Hence, maintenance of such a therapy after initiation by an oncologist can be undertaken by a palliative care physician. However, there is little or no evidence of use of therapy in metronomic in hospice setting and hence, routine use of oral low-dose chemotherapy for palliation needs more validation in terms of controlled studies.
CONCLUSION
Primary duodenal adenocarcinoma is a rare tumor with modest prognosis after surgical resection. Metastatic duodenal adenocarcinoma has much graver prognosis with very little treatment options, especially, for patients with poor performance status. In this setting, oral cyclophosphamide-based metronomic chemotherapy is a viable option as a first-line therapy in achieving response, symptom relief and prolongation of survival as documented in the present case.
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- Adenocarcinoma of the small bowel: Presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004;101:518-26.
- [Google Scholar]
- Malignant tumors of the small intestine: A histopathologic study of 41 cases among 1,312 consecutive specimens of small intestine. Int J Clin Exp Pathol. 2012;5:203-9.
- [Google Scholar]
- Survival predictors of patients with primary duodenal adenocarcinoma. Int Surg. 2011;96:111-6.
- [Google Scholar]
- Cyclophosphamide-based metronomic chemotherapy: After 10 years of experience, where do we stand and where are we going? Crit Rev Oncol Hematol. 2012;82:40-50.
- [Google Scholar]
- Chemotherapy with 5-fluorouracil and a platinum compound improves outcomes in metastatic small bowel adenocarcinoma. Cancer. 2008;113:2038-45.
- [Google Scholar]
- Phase II study of 5-fluorouracil, doxorubicin, and mitomycin C for metastatic small bowel adenocarcinoma. Oncologist. 2005;10:132-7.
- [Google Scholar]
- Metronomic chemotherapy: An antiangiogenic scheduling. Clin Transl Oncol. 2007;9:93-8.
- [Google Scholar]
- The anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer. 2004;4:423-36.
- [Google Scholar]
- Oral metronomic cyclophosphamide with and without methotrexate as palliative treatment for patients with metastatic breast carcinoma. Anticancer Res. 2012;32:529-36.
- [Google Scholar]
- Metronomic oral combination chemotherapy with capecitabine and cyclophosphamide: A phase II study in patients with HER2-negative metastatic breast cancer. Cancer Chemother Pharmacol. 2012;70:331-8.
- [Google Scholar]
- Complete remission and long-term survival in a child with relapsed medulloblastoma with extensive osteosclerotic bony metastasis with a novel metronomic chemobiological approach. J Pediatr Hematol Oncol. 2012;34:e195-8.
- [Google Scholar]
- Continuous low-dose cyclophosphamide and methotrexate combined with celecoxib for patients with advanced cancer. Br J Cancer. 2011;104:1822-7.
- [Google Scholar]
- Metronomic therapy with cyclophosphamide and dexamethasone for prostate carcinoma. Cancer. 2003;98:1643-8.
- [Google Scholar]
- Clinical, pharmacokinetic and pharmacodynamic evaluations of metronomic UFT and cyclophosphamide plus celecoxib in patients with advanced refractory gastrointestinal cancers. Angiogenesis. 2012;15:275-86.
- [Google Scholar]






