Translate this page into:
Multiple Nutritional Deficiencies in Cerebral Palsy Compounding Physical and Functional Impairments
Address for correspondence: Dr. PG Hariprasad, Department of Pediatrics, Government Medical College, SAT Hospital, Thiruvananthapuram, Kerala, India. E-mail: pghariprasad@yahoo.co.in
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Cerebral palsy (CP) refers to a spectrum of disorders causing physical and intellectual morbidity. Macro and micro nutrient deficiencies often contribute to the subnormal physical and mental capabilities of them.
Objectives:
To assess the growth, nutritional status, physical and functional ability and quality of life in cerebral palsy children and to determine any relation with their gross motor and functional capabilities.
Method:
The study was conducted at a Tertiary Care Centre, with the participants in the age group 1-16 years. A pretested evaluation tool was prepared which included Anthropometric measurements, tests for hemoglobin and Vitamin D estimation, evidence of micronutrient deficiencies, Dietary patterns, Epidemiological factors, Functional assessment using GMFM (Gross Motor Function Measure ) and FIM (Functional Independent Measurement) scales and Quality of life (QOL) assessment. The data was statistically analyzed.
Results:
Out of the 41 children, 30 had quadriplegia, 3 had hemiplegia and 8 had spastic diplegia. 34 (82.9%) were severely underweight, 35 (85.4%) had severe stunting and 38 (92.7%) had severe wasting. Micronutrient deficiencies were noted like vitamin B complex deficiency in 37 (90.2%), vitamin A deficiency in 31 (75.6%), low vitamin D levels in 27 (65.9%) and insufficient levels in 9 (22%), severe anemia in 5 (12.2%) and moderate anemia in 26 (63.4%). The gross motor and functional scores were suboptimum in the majority of patients and the care givers had significant impairment in the quality of life.
Conclusion:
Majority of children with cerebral palsy had multiple nutritional deficiencies, gross motor and functional disabilities. QOL of the children and their care givers were suboptimum. A comprehensive package that address dietary intake, correction of micronutrient deficiencies especially anemia and vitamin D deficiency, physical and emotional support is recommended for the wellbeing of the affected children.
Keywords
Cerebral palsy
functional ability
malnutrition
micronutrient deficiency
physical disability
INTRODUCTION
Cerebral palsy (CP) is a nonprogressive neuromotor disorder of central origin in children with multiple neurological deficits and variable intellectual disabilities. They also suffer from seizures, feeding problems, multiple nutritional deficiencies, and social isolation. The quality of life is also affected and the caretakers perceive various hardships. The prevalence is as high as 3.5 per 1000 children all across the globe with a slightly growing trend in incidence over the years.[1] The available data from India also show the prevalence of 3 per 1000 children.[2] Various risk factors operating during prenatal and natal period have been proved as risk factors for the cause of CP.[3]
The physical and mental disabilities due to the disease pose serious challenges; both to the patient and to the caregiver.[456] Providing proper care to them requires massive commitment from the part of all caregivers, particularly the parents. With increased physical disability or decreased functional capability of the patient, the stress on the caregiver rises.
Malnutrition and feeding problem among these children pose a great challenge both for the patient and the caregiver.[6] Severely affected children require more time or assistance for each feed. Nutritional inadequacy and problems arising due to it contribute to a sizeable proportion of the problem.[78910] Increasing severity of the disease contributes to increasing nutritional problems and vice versa, forming a vicious cycle.[10]
Children having severe motor impairment such as spastic quadriplegia will experience greater oropharyngeal dysphagia than diplegics, resulting in both macro- and micro-nutrient deficiencies,[78] pulmonary complications,[11] decreased gross motor attainment,[811] and decreased generalized well-being.[11] Anemia due to decreased iron or folic acid absorption is also rampant.[12] Malnutrition has also been found to cause decreased secretion of insulin-like growth factor 1 in affected children, resulting in growth and developmental delay.[1314]
Decreased serum Vitamin D level is another major deficiency noted in these children. Inadequate exposure to sunlight and anticonvulsant medications along with decreased food intake contribute to this. This results in decreased mean bone mineral density, causing muscular weaknesses, development of contractures,[15] functional impairment, and pathological fractures.[16]
The incidence of anemia also tends to be significantly high among these children due to lack of nutritional food intake, families depending on staple diet, recurrent infections, and multiple drug intake, adding on to their morbidity. Other deficiencies such as Vitamin B complex and Vitamin A deficiency are also high among them due to inadequate intake of all food groups including fruits and vegetables.
These multiple deficiencies along with physical and functional impairment add on to the suffering of the child and the family. Addressing these problems will significantly help in rehabilitating and improving the quality of life of these children and their families.
Aim of the study
To assess the Anthropometry, Biochemical estimation of Vitamin D and hemoglobin, Clinical assessment, Dietary intake, Epidemiological factors, Functional ability, and Quality of life of children including perception of caretakers using a composite assessment (ABCDEFQ) package. This is expected to help in planning comprehensive intervention for the well-being of the affected children and their families.
MATERIALS AND METHODS
The study was conducted as a hospital-based, cross-sectional survey in a tertiary care center, SAT Hospital, Government Medical College, Thiruvananthapuram, during the period of July–December 2015. Approval of the Institution's Ethics Committee and written informed consent from the caregivers of the children were obtained prior to enrollment.
The study participants were diagnosed cases of CP in the age group of 1 to 16 years. Relevant data were collected from caregivers and hospital records. Consecutive cases during the study period were enrolled. A composite evaluation tool, ABCDEFQ, was prepared to assess the Anthropometry, Biochemical assessment of Vitamin D and hemoglobin, Clinical assessment, Dietary intake, Epidemiological factors, Functional ability, and Quality of life. The suggested tool was derived from the observed data of the pilot study conducted.
The anthropometric measurements were taken using standardized methods ensuring inter- and intra-observer reliability. The physical grades of underweight (weight for age), stunting (height for age), and wasting (weight for height) were determined. Functional assessment of the children was carried out, and 24 h dietary recall method was used to estimate dietary intake.
Vitamin D estimation was done by the “ELISA” technique and hemoglobin level by “CALORIMETRIC” method at an accredited laboratory. Clinical evidence of Vitamin A deficiency (conjunctival xerosis or Bitot's spots) and that of Vitamin B (angular stomatitis and cheilitis) was looked for.
The physical disability was assessed by a modified version of Gross Motor Function Measure (GMFM) and functional ability by a modified functional-independent measure (FIM) scale. GMFM is a standardized observational instrument designed to measure change in gross motor function over time. The GMFM assesses motor function (how much of a task the child can do) rather than the quality of the motor performance (how well the child performs the task). Modified GMFM-66, adapted from GMFM-88 scale, was used to assess children with CP aged 5 months to 16 years. With the GMFM-66 scale, each child was assessed by a pediatrician, a physiatrist, and a physiotherapist at a 3 monthly interval starting from the initial visit. It tests activities in five dimensions: lying and rolling, sitting, crawling and kneeling, standing and walking, and running and jumping. It is a standardized observational instrument designed and validated to measure the changes in gross motor function in children over time.
The FIM instrument is a basic indicator of severity of disability. The functional ability of a patient changes during rehabilitation and the FIM instrument is used to track those changes. Functional change is a key outcome measure of rehabilitation episodes. It comprises 18 items, each of which is assessed with a 7-point ordinal scale. Higher the score for an item, the more independently the patient can perform the tasks assessed by that item. The items are divided into two major groups; 13 motor items and 5 cognitive items. Total scores range from 18 to 126. The rating scale designates major graduations in behavior from dependence to independence and provides for the classification of individuals by their ability to carry out an activity independently versus their need for assistance from another person or a device.
The GMFM-66 and FIM questionnaires were modified in such a way that the modified tools contained the items more suited for the study population. The content of the modified scale was given to a group of expert team comprising a pediatrician, a pediatric neurologist, a physiatrist, a palliative care physician, a psychologist, a physiotherapist, and an occupational therapist and it was validated qualitatively. The tool also contained a subset of WHO-BREF questionnaire to get an insight into the quality of life of the caregiver. The overall scores of the tools were used for cross-tabulations. The study is reported as per the STROBE statement.
Statistical analysis
The observations were computed and analyzed using SPSS software version 16 (SPSS Inc. Released 2007. SPSS for Windows, Trial Version 16.0. Chicago, SPSS Inc.). Quantitative variables were expressed as mean (standard deviation) and categorical variables as percentages. The outcome variables for the study were the nutritional status measured in terms of anthropometry, clinical evaluation, and biochemical evaluation. Motor and functional activities of the study participants were also assessed.
The association between the type of CP and nutritional deficiencies was analyzed. The type of CP was categorized into quadriplegic CP and nonquadriplegic CP for cross-tabulations. Grade of disability on GMFM was categorized into “Grade 5 disability” and others while functional independence on FIM scale was dichotomized into “complete dependence” and others. Fisher's exact test was used to determine the strength of association in most of the occasions because of inadequacy in numbers. All the categorical outcome variables were changed into dichotomous format with the most severe in one group and the rest into another group for this analysis.
RESULTS
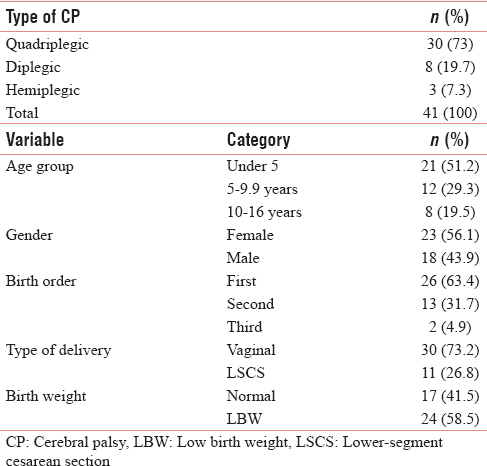
The participants in the present study were 41 children with a minimum completed age of 1 year and maximum of 16 years. The mean (standard deviation [SD]) age of the participants was 5.50 (3.83) years. Among the participants, 56.1% (n = 23) were girls and the rest were boys. Two-third of the participants (n = 26, 63.4%) were of first birth order and three-fourth (n = 30, 73.2%) were born out of term vaginal delivery [Table 1]. The range of birth weights was 1.43–3.5 kg with a mean (SD) of 2.34 (0.56) kg. Twenty-four of the 41 participants (58.5%) were of low weight at birth (LBW babies) for a cutoff of 2.5 kg [Table 1].
Various anthropometric, clinical, and biochemical parameters were assessed to estimate the nutritional status of the study participants [Table 2]. Out of the 41 children, majority, i.e. 34 (82.9%) were severely underweight with weight for age <50%, 35 (85.4%) had severe stunting with height for age <85%, and 38 (92.7%) had severe wasting with weight for height <70% of the expected.
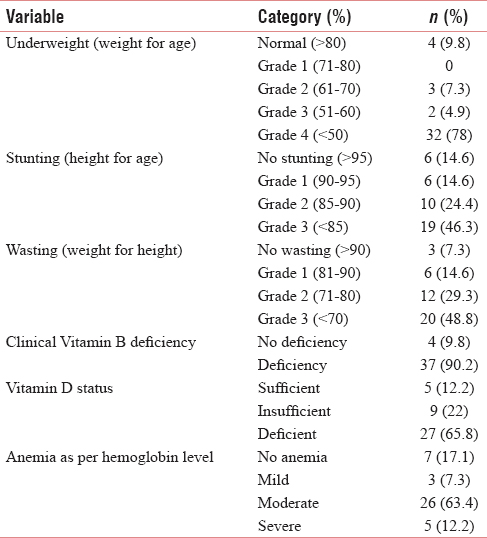
Clinically, Vitamin B complex deficiency was noted in 37 (90.2%) participants and Vitamin A deficiency in 31 (75.6%).
As per the US Endocrine Society Classification of Vitamin D (sufficient: above 30 ng/ml, insufficient: 20–30 ng/ml, and deficient: <20 ng/ml), levels were found to be deficient in 27 (65.9%) and insufficient in 9 (22%) participants. Mean Vitamin D level was found to be 20.1 mg/ml with a minimum and maximum of 6.6 ng/ml and 68.0 ng/ml, respectively.
Severe anemia was detected in 12.2% (n = 5) of the participants while 63.4% (n = 26) suffered from moderate anemia. The mean hemoglobin of the study population was found to be 9.19 g/dl with a minimum of 3.7 g/dl and a maximum of 13.0 g/dl. Severities of anemia in various age groups among participants were categorized with respect to the WHO guidelines.
Accordingly, the normal hemoglobin value in the age groups of 6 months to 5 years was 11 g/dl or more with an addition of 0.5 g/dl each in the age groups of 5–11 years and 11–14 years, respectively. Severe anemia was detected in 12.2% (n = 5) of the participants while 63.4% (n = 26) suffered from moderate anemia and 7.3% (n = 3) from mild anemia [Table 2].
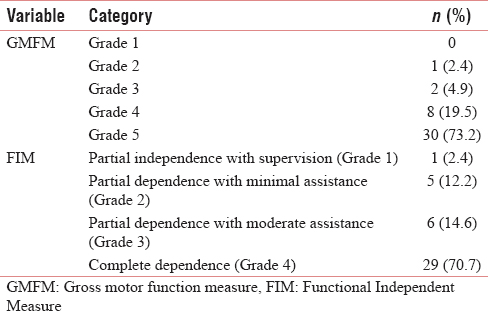
Physical disability and functional independence of the study participants were estimated at the beginning of the study [Table 3]. Physical disabilities were assessed by a series of questions adapted from the GMFM questionnaire. Increasing severity of disability was graded from 1 to 5. Maximum disability of Grade 5 was present in 73.2% (n = 30) of the participants. In a similar manner, functional independence of the participants was assessed by questions adapted from the FIM questionnaire. Most of the patients (n = 29, 70.7%) fell into the category of Grade 4 (complete dependence). The GMFM and FIM scores were well correlated with Spearman's rank correlation coefficient of 76.9% (P < 0.001).
The participants were categorized on the basis of type of CP and the majority (73.3%, n = 30) were suffering from the quadriplegic type. Hemiplegic type of CP was found in 7.3% (n = 3) of the participants while diplegic type in 19.5% (n = 8). The relation between Grade 4 undernutrition and type of CP was assessed. The odds ratio was found to be 77.3 with a confidence interval of 7.05–847.95 and P < 0.001. Similarly, Grade 3 stunting (P = 0.038), Grade 3 wasting (P < 0.001), moderate-to-severe anemia (P < 0.001), and Grade 5 disability (P = 0.003) were found to have statistically significant association with quadriplegic CP. Mean Vitamin D levels and type of CP were also found to be statistically significantly associated using the Student's t-test (P = 0.043). Clinical features of Vitamin B deficiency, Vitamin A deficiency, and complete dependence (FIM scale) were reported more in quadriplegic group, but the association was not found to be significant [Table 4].
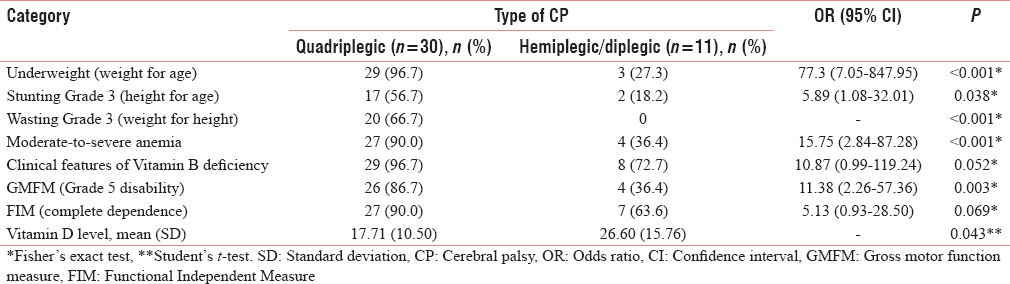
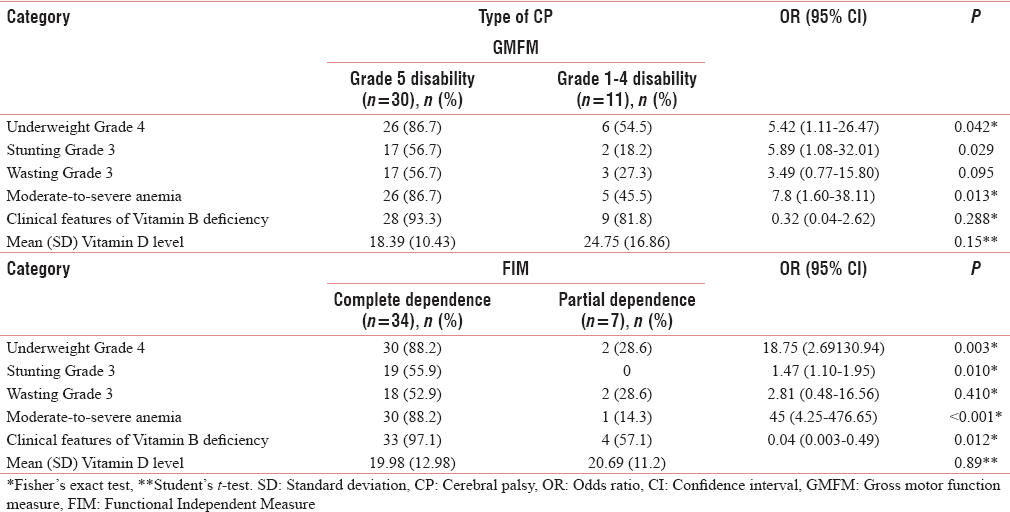
Participants were also categorized on the basis of severity of disability into Grade 5 disability (n = 30) and Grade 1–4 disability (n = 11) on the GMFM scale. Undernutrition of Grade 4 (P = 0.042), stunting of Grade 3 (P = 0.029), and moderate-to-severe anemia (P = 0.013) were also found to have significant association with Grade 5 disability on the GMFM [Table 5]. Dependence of the patient on caregiver was assessed using the FIM scale and was categorized into complete dependence (n = 34) and partial dependence (n = 7) on caregiver. Here also, undernutrition of Grade 4 (P = 0.003), stunting of Grade 3 (P = 0.010), moderate-to-severe anemia (P < 0.001), and features of Vitamin B deficiency (P = 0.012) were found to have significant association with complete dependence on the FIM scale [Table 5].
DISCUSSION
Children suffering from neuromotor disorders have varying types of nutritional inadequacies.[3] This phenomenon is clearly seen by the very high rates of protein–energy malnutrition, stunting and wasting in the study participants. The current study revealed that more than 90% of the children were found to be suffering from some form of undernutrition and three-fourth of them were suffering from its severest form. It has been shown previously in similar settings that, with increasing severity of undernutrition, developmental, motor, and mental quotients of these children deteriorate substantially.[17] Apart from the inadequate intake, this could be due to deficiencies in the release of growth hormone contributing to a delayed rate of increase in height.[11] Inadequate growth was observed significantly more in quadriplegic CP as documented elsewhere by Brazilian researchers.[13] Quadriplegic CP is more severe in comparison with the other forms of CP in this study. Children with quadriplegic CP were suffering from more physical and neurological abnormalities.
Nutritional deficiencies indicated by the presence of anemia, Vitamin B deficiency, Vitamin A deficiency, and Vitamin D deficiency were found to be more among severe forms of CP which is consistent with the opinions stated by experts from around the world.[561318] Even though other data along with that of the present study show that low Vitamin D levels are associated with CP,[19] a study conducted in Uganda could find no significant difference in Vitamin D values between the malnourished and normal children.[20] Nonnutritional factors such as exposure to sunlight might have contributed to the differences in the pattern of Vitamin D deficiencies in different parts of the world. However, there is enough evidence that hidden hunger is also prominent in these children along with macronutrient deficiencies. The current study also documented that the children with quadriplegic CP were more prone foremost of the micronutrient deficiencies compared to less severe forms of CP.
Correlation between GMFM and FIM scores also indicated that motor capabilities are directly contributing to the level of self-dependence in children with CP. Severe forms of disease were more associated with extreme forms of motor and functional difficulties, resulting in increased dependence on the caregivers. Hence, categorizing children under various types of CP at the earliest is of utmost importance as their nutritional and other requirements could be catered to, in a more comprehensive manner. It is evident from the current data that anthropometric (height and weight), nutritional (nutritional deficiencies), clinical (types of CP), and functional (assessed by GMFM and FIM) parameters are well correlated in these children. A comprehensive “ABCDEFQ” assessment approach is recommended for monitoring these children which includes Anthropometric, Biochemical, Clinical, Dietary, Epidemiological, Functional parameters, and Quality of life.[21]
The severity of undernutrition increases with the extent of disabilities. The conventional approaches to tackle malnutrition may not be suited for this special group of children because of their physical and physiological inabilities. Most of these children belong to socioeconomically disadvantageous families and were more vulnerable to malnutrition.[4] Similar to children with severe malnutrition, nutritional rehabilitation centers and locally prepared therapeutic food is recommended to children with CP also.[22] Other community feeding programs such as Integrated Child Development Scheme may be re-directed to tackle the nutritional problems of these special group of children.
CONCLUSION
Majority of children with CP had growth faltering and various nutritional deficiencies due to multiple problems such as poor dietary intake and feeding difficulties. Most of them had significant gross motor and functional disabilities, which were more in quadriplegic CP. Quality of life of the children and their caregivers was also suboptimum.
A comprehensive package that addresses dietary intake, correction of micronutrient deficiencies, especially anemia and Vitamin D deficiency, physical and emotional support is recommended for the well-being of the affected children.
Financial support and sponsorship
This study was financially supported by the State Council for Persons with Disability, Trivandrum, Kerala.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. Selvan, physiatrist, and Mr. Sunaj, physiotherapist, for giving their input in assessing physical disability using the GMFM.
REFERENCES
- Trends in the prevalence of autism spectrum disorder, cerebral palsy, hearing loss, intellectual disability, and vision impairment, metropolitan Atlanta, 1991-2010. PLoS One. 2015;10:e0124120.
- [Google Scholar]
- Prevalence of cerebral palsy in children <10 years of age in R.S. Pura town of Jammu and Kashmir. J Trop Pediatr. 2011;57:293-5.
- [Google Scholar]
- Nutritional problems in children with neuromotor disabilities: An Italian case series. Ital J Pediatr. 2014;40:61.
- [Google Scholar]
- Elementary school enrolment and its determinants among children with cerebral palsy in Thiruvananthapuram district, Kerala, India. J Neurosci Rural Pract. 2013;4:S40-4.
- [Google Scholar]
- Feeding children with cerebral palsy and swallowing difficulties. Eur J Clin Nutr. 2013;67(Suppl 2):S9-12.
- [Google Scholar]
- Dietary intakes and nutritional issues in neurologically impaired children. Nutrients. 2015;7:9400-15.
- [Google Scholar]
- Child characteristics, caregiver characteristics, and environmental factors affecting the quality of life of caregivers of children with cerebral palsy. Disabil Rehabil. 2016;38:2374-82.
- [Google Scholar]
- Quality of life of primary caregivers of children with cerebral palsy: A controlled study with short form-36 questionnaire. Dev Med Child Neurol. 2004;46:647-8.
- [Google Scholar]
- Comparison of impact on mood, health, and daily living experiences of primary caregivers of walking and non-walking children with cerebral palsy and provided community services support. Eur J Paediatr Neurol. 2010;14:239-46.
- [Google Scholar]
- Increased incidence of iron deficiency anemia secondary to inadequate iron intake in institutionalized, young patients with cerebral palsy. Int J Hematol. 2008;88:495-7.
- [Google Scholar]
- Puberty, statural growth, and growth hormone release in children with cerebral palsy. J Pediatr Rehabil Med. 2009;2:131-41.
- [Google Scholar]
- Longitudinal cohort protocol study of oropharyngeal dysphagia: Relationships to gross motor attainment, growth and nutritional status in preschool children with cerebral palsy. BMJ Open. 2012;2(4)
- [Google Scholar]
- Food pattern and nutritional status of children with cerebral palsy. Rev Paul Pediatr. 2013;31:344-9.
- [Google Scholar]
- Impact of gastrostomy tube feeding on the quality of life of carers of children with cerebral palsy. Dev Med Child Neurol. 2004;46:796-800.
- [Google Scholar]
- The impact of caring for a child with cerebral palsy: Quality of life for mothers and fathers. Child Care Health Dev. 2010;36:63-73.
- [Google Scholar]
- Effect of Vitamin D and calcium on bone mineral density in children with CP and epilepsy in full-time care. Dev Med Child Neurol. 2000;42:403-5.
- [Google Scholar]
- Growth faltering and developmental delay in children with PEM. Indian Pediatr. 1991;28:255-8.
- [Google Scholar]
- Cerebral palsy in children as a risk factor for malnutrition. Ann Nutr Metab. 2015;66:224-32.
- [Google Scholar]
- Effect of supplementation with a single dose of vitamin D in children with cerebral palsy. preliminary randomised controlled study. Rev Chil Pediatr. 2015;86:393-8.
- [Google Scholar]
- Serum Vitamin D status in children with protein-energy malnutrition admitted to a national referral hospital in Uganda. BMC Res Notes. 2015;8:418.
- [Google Scholar]
- Crusade against malnutrition: Nutrition education program. Indian Pediatr. 2016;53:203-5.
- [Google Scholar]
- Nutrition rehabilitation centers and locally prepared therapeutic food in the management of severe acute malnutrition. Pediatrician's perspective. Indian Pediatr. 2014;51:19-20.
- [Google Scholar]






