Translate this page into:
Opioid Use Disorders among Patients on Long-Term Morphine for Management of Chronic Cancer Pain: A Pilot Study from a Tertiary Palliative Care Facility

*Corresponding author: Dr. Sushma Bhatnagar, Department of Onco-Anaesthesia and Palliative Medicine, All India Institute of Medical Sciences, New Delhi, India. sushmabhatnagar1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhary N, Singh S, Rathore P, Ambekar A, Bhatnagar S. Opioid use disorders among patients on long-term morphine for management of chronic cancer pain: A pilot study from a tertiary palliative care facility. Indian J Palliat Care 2021;27(2):264-8.
Abstract
Objectives:
Long-term opioid use can be associated with misuse and addiction. In the backdrop of increasing burden of cancer patients in India, it is important to assess the rate of opioid use disorders among those with chronic cancer pain. The objectives were to measure the rate of opioid use disorder in chronic cancer pain patients being managed with morphine and to assess its association with demographic and clinical characteristics.
Materials and Methods:
A cross-sectional study was conducted on chronic cancer pain patients who were prescribed morphine for ≥12 months, dosage of ≥60 mg/day. They were assessed using MINI version 7.0.0, WHO-ASSIST Hindi questionnaire, Addiction Behavior Checklist, and DSM-5 for opioid use disorder.
Results:
Forty patients who were treated with morphine for a total of 1479 months participated. The average morphine consumption was 159.50 ± 327.90 mg/day. Six (15%) showed possible inappropriate opioid analgesic use and none of the patients had opioid use disorder.
Conclusion:
This study reports the absence of opioid use disorder due to vigilant use of morphine in chronic cancer patients.
Keywords
Chronic cancer pain
Lng-term opioid analgesics
Morphine
Opioid-related disorders
Opioid use in India
INTRODUCTION
India is facing a cancer epidemic, with around 2.25 million patients living with the disease.[1] Sixty percent cancer patients in India suffer from severe pain, yet only about 1% of cancer patients receive adequate dosage of morphine and other opioid analgesics as per the established guidelines.[2] Tough regulations on medical and scientific use of opioids and “opioidophobia” among medical practitioners are key reasons for inadequate opioid use in India.[3,4] On the contrary, United States is dealing with a different kind of opioid crisis.[5] Due to easy availability of opioids, the rates of inappropriate opioid use and opioid disorder have risen dramatically. In this scenario, information on opioid use disorders among these chronic cancer pain patients would provide valuable insight on how to optimize the pain management guidelines.
A review of literature of studies measuring the prevalence of opioid addiction in chronic pain patients indicates that the sub-population with cancer pain had lower addiction rates varying between 0% and 7.7%.[6] Indian patients in need of opioid analgesics for cancer pain management are underdosed due to fear of iatrogenic dependence. Rajagopal et al. reported zero instance of misuse or diversion upon longitudinal assessment of 1723 patients who were on oral morphine on an outpatient home care basis.[7] Apart from this report, research on exploring the prevalence of opioid dependence in those with chronic cancer pain has been scarce in India. This study aimed to find the prevalence rate of opioid use disorder in cancer patients who are being treated with opioids at a tertiary cancer hospital in India and to assess its association with demographic and clinical characteristics.
MATERIALS AND METHODS
The study was carried out at the Department of Onco-Anesthesia and Palliative Medicine, AIIMS, New Delhi. It was a cross-sectional observational study and data collection took place for a continuous period of 6 months in 2018. Purposive sampling method was used. The inclusion criteria were those who were receiving uninterrupted morphine for chronic cancer pain for ≥12 months; most recent prescription showing morphine equivalent dosage of ≥60 mg; age ≥18 years; and those willing to give consent. Patients who could not be interviewed due to a communication disability were excluded from the study. Instruments used in the study included (a) a semi-structured pro forma to record sociodemographic details, (b) a semi-structured pro forma to collect clinical details (current diagnosis, details about pain complaints, history of analgesics use and current management status, number of proxy visits, and follow-up history), (c) MINI version 7.0.0 (a brief, reliable, and valid structured diagnostic interview to screen for comorbid mental disorders),[8] (d) WHO-ASSIST v 3.0 (WHO-Alcohol, Smoking, and Substance involvement screening test – Hindi version,[9] to screen for the presence of probable substance use disorders), and (e) Addiction Behavior Checklist (ABC).[10] To avoid misreporting due to multiple testing, the alcohol use disorder and non-alcohol use disorder sections of MINI7.0.0 were not used. The WHO-ASSIST questionnaire was used as it has the inherent property of not testing for misuse of prescribed opioids. The ABC is a dichotomous rating scale and a score of ≥3 suggests inappropriate use of opioid analgesics for chronic pain. The questionnaire was translated to Hindi and back translated to English to ensure content equivalence. The study subjects were assessed through these instruments in a single sitting. Those who screened positive for a psychiatric disorder on applying MINI 7.0 questionnaire and/or scored higher than 4 on WHO-ASSIST questionnaire and/or scored ≥3 on ABC were referred to a psychiatrist. Within the next 7 days, a psychiatrist carried out an assessment for opioid use disorder in referred cases as per the DSM-5 criteria.[11] Figure 1 outlines the study method. The study was conducted after obtaining ethical clearance from the institutional ethics committee.
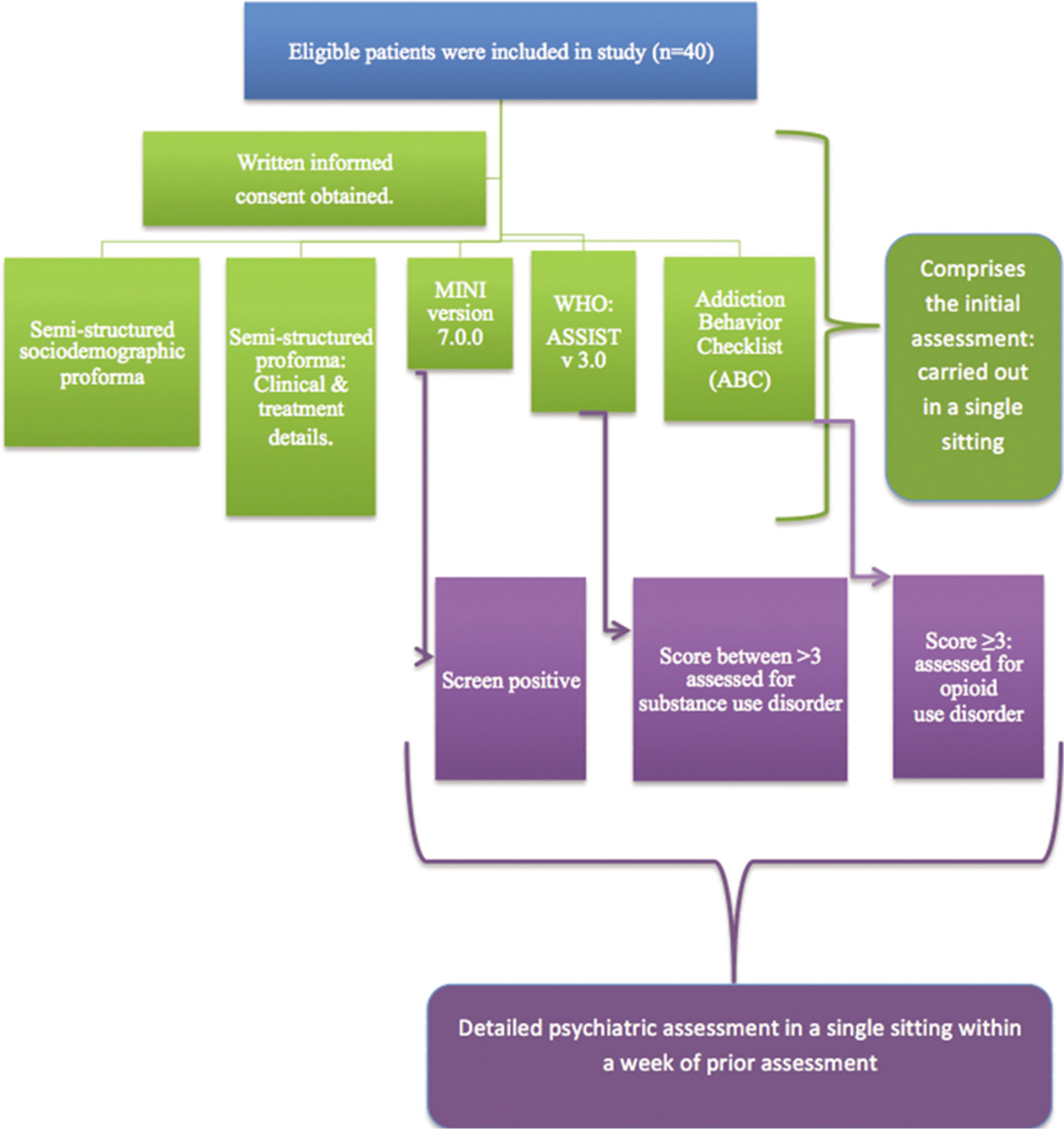
- A flowchart outlining the study procedure
Statistical analysis
Descriptive statistics were used for outlining sociodemographic and clinical characteristics of the sample. Comparative analysis was done using Chi-square test and correlation analysis was carried out using Spearman’s Rho coefficient. P < 0.05 was considered statistically significant.
RESULTS
We assessed 40 cancer patients who experienced cancer pain and were treated with morphine for a total of 1479 months. The maximum duration of opioid use for pain management was 216 months and average duration was 36.98 (standard deviation [SD]: 36.73) months. Most of the patients (77.5%) were in the age group of 30–60 years. Carcinoma breast (32.5%) was the most common diagnosis followed by head and neck cancer (20%). The most common site of pain was lower back (22.5%), followed by the chest (20%) and abdomen (20%). A majority (77.5%) of the participants had mixed pain, while 10% of participants had neuropathic pain. All of the patients received morphine exclusively. The sociodemographic and clinical parameters are detailed in Tables 1 and 2, respectively. Dosing on a PRN basis was used by 30% (n = 12) of the participants in the past 3 months. The mean pain rating scale scores (0 for no pain to 10 for maximum pain) in the past 3 months and 24 h were 7.07 (SD: 2.014) and 6.59 (SD: 2.16), respectively. The mean dose of morphine used by the studied sample was 159.50 ± 327.90 mg/day and the dose ranged from 20 to 240 mg/day.
| Variables | n (%) |
|---|---|
| Age | |
| Mean years±SD | 47.50±11.40 |
| Range(years) | 28-75 |
| Sex (%) | |
| Male | 14 (35) |
| Female | 26 (65) |
| Employment status | |
| Employed | 16 (40) |
| Unemployed | 24 (60) |
| Education | |
| Illiterate | 14 (35) |
| Graduate | 24 (60) |
| Postgraduate | 2 (5) |
SD: Standard deviation
| Variables | n (%) |
|---|---|
| Stage of disease (%) | |
| I | 14 (35) |
| II | 6 (15) |
| III | 3 (7.5) |
| IV | 17 (42.5) |
| Disease status | |
| Disease progression | 10 (25) |
| Stable disease | 25 (62.5) |
| On active therapy | 5 (12.5) |
| Diagnosis | |
| Head and neck | 8 (20) |
| Carcinoma of the lung | 2 (5) |
| Carcinoma of the breast | 13 (32.5) |
| Gastrointestinal | 1 (2.5) |
| Genitourinary | 2 (5) |
| Bone and soft tissue | 5 (12.5) |
| Hematological | 4 (10) |
| Miscellaneous | 5 (12.5) |
| Type of pain | |
| Mixed | 31 (77.5) |
| Neuropathic | 4 (10) |
| Nociceptive | 5 (12.5) |
Those who had higher morphine daily doses were more likely to require PRN dosing, although the difference is not statistically significant (U = 58.5, P = 0.354). No significant association was found between higher pain rating scale scores and higher rates of PRN dosing in this sample (U = 52, P = 0.217). None of the participants screened positive for moderate or severe substance use involvement.
Six participants (15%) screened positive for inappropriate opioid analgesic use based on ABC. However, on the subsequent clinical evaluation by a psychiatrist, none of them met the diagnostic criteria for opioid use disorder. Figure 2 illustrates the relationship between PRN opioid analgesic use and ABC scoring. Having possible inappropriate opioid analgesic use was significantly associated with a higher rate of PRN dosing (Chi-square = 21.75, P < 0.01) but not with a higher dose of morphine being prescribed (U = 6, P = 0.383). Possible inappropriate opioid analgesic use was not significantly associated with a higher value on the pain rating scale, U = 7.5, P = 0.484. None of the participants had psychiatric or substance use disorder.
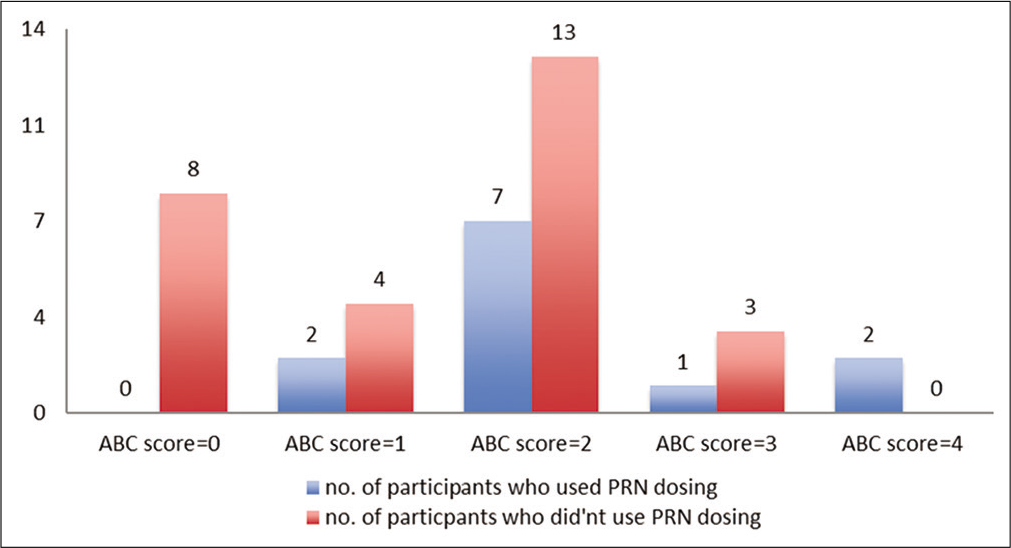
- Relationship between the number of participants who used opioid analgesics on a PRN basis and their scores on the Abnormal Behavior Checklist. An Addiction Behavior Checklist score of ≥3 indicates inappropriate opioid analgesic use. The y-axis denotes the number of participants. Having inappropriate opioid analgesic use was significantly associated with a higher rate of PRN dosing (P = 0.028)
DISCUSSION
The rate of possible inappropriate use of opioid analgesics in this study is 15%, higher than that recorded in a previous such study on oncology inpatients (7.7%).[12] None of the patients diagnosed with inappropriate use in our study met the DSM-5 criteria for opioid use disorder. Previously, Rajagopal et al. reported no misuse of opioid analgesic when prescribed for management of cancer pain in Indian patients.[7] No study has assessed the prevalence of opioid use disorder systematically in Indian patients receiving opioid analgesics for chronic cancer pain. Moreover, previous studies did not use DSM-5 diagnostic criteria or other standardized diagnostic criteria to diagnose addiction to opioid analgesics.[6]
In a previous study (n = 568), all six patients (0.02%) who had misused opioid analgesics had “significant psychological disease” along with cancer-related pain.[13] None of the patients in our study had psychiatric or substance use disorders. A high false discovery rate of substance use disorder was avoided by using the MINI 7.0.0 and WHO-ASSIST exclusively for screening psychiatric and non-prescription opioid use disorders, respectively. In our study, we found that there is a significant association between possible inappropriate opioid analgesic use and PRN dosing. This could be because of the resultant higher dose of morphine used and use of morphine for reasons other than symptomatic management of pain. However, this could not be established in our study. The results of our study are altogether different from the current crisis of opioid epidemic going on in the western world. This is mainly attributed to the vigilant clinical practice of prescribing opioids being followed at our institute for more than a decade. Another reason for the lower rates of opioid use disorder in our sample could be the preponderance of the female population.[14]
This study has limitations. It is a cross-sectional analysis at a tertiary care hospital, with convenience sampling and a small sample size. Hence, the findings are not generalizable and many of the significant associations might have been missed. Second, the use of illicit drugs by participants was not ruled out by a urinalysis for psychoactive substances, though Indian research has found self-reports by Indian patients in the clinical settings to be quite reliable.[15] The tool used for detecting aberrant drug use, ABC, is not culturally adapted for the Indian population. Finally, this ABC identifies PRN use of opioids for chronic pain management as one of the qualifiers for possible inappropriate opioid analgesic use. However, PRN dosing is a common practice in those suffering from chronic cancer-related pain.
CONCLUSION
The rate of possible inappropriate opioid use was 15% and no opioid use disorder due to prescription of opioids was detected in this sample. Further research on a larger sample size needs to be done to ascertain rate of prescription opioid abuse and addiction in India. The risk factors and protective factors associated with opioid misuse in those with chronic pain need to be ascertained in further studies.
Acknowledgments
The authors would like to express their sincere gratitude to all the participants and medical staff of onco-anesthesia and palliative medicine department for their support throughout this study.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cancer Statistics (nd.) From India against Cancer. Available from: http://cancerindia.org.in/cancer-statistics/ [Last retrieved on 2019 Aug 13]
- [Google Scholar]
- India: Opioid availability: An update. J Pain Symptom Manage. 2007;33:615-22.
- [CrossRef] [Google Scholar]
- Predictors and prevalence of pain and its management in four regional cancer hospitals in India. J Glob Oncol. 2018;4:1-9.
- [CrossRef] [Google Scholar]
- An ethnographic study of barriers to cancer pain management and opioid availability in India. Oncologist. 2014;19:515-22.
- [CrossRef] [Google Scholar]
- Opioid abuse in chronic Painâ Misconceptions and mitigation strategies. New England J Med. 2016;374:1253-63.
- [CrossRef] [Google Scholar]
- Addiction to opioids in chronic pain patients: A literature review. Europ J Pain (London, England). 2007;11:490-518.
- [CrossRef] [Google Scholar]
- Medical use, misuse, and diversion of opioids in India. Lancet. 2001;358:139-43.
- [CrossRef] [Google Scholar]
- The validity of the mini international neuropsychiatric interview (MINI) according to the SCID-P and its reliability. Europ Psychiatry. 1997;12:232-41.
- [CrossRef] [Google Scholar]
- A randomized controlled trial of a brief intervention for illicit drugs linked to the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in clients recruited from primary health-care settings in four countries. Addiction (Abingdon, England). 2012;107:957-66.
- [CrossRef] [Google Scholar]
- The addiction behaviors checklist: Validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manag. 2006;32:342-51.
- [CrossRef] [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders. 2013. (5th ed). Arlington: American Psychiatric Association; Available from https://www.psychiatry.org/psychiatrist/practice/dsm [Last accessed on 2017 Dec 04]
- [Google Scholar]
- A pilot survey of aberrant drug-taking attitudes and behaviors in samples of cancer and AIDS patients. J Pain Symptom Manage. 2000;19:274-86.
- [CrossRef] [Google Scholar]
- Opioid abuse and misuse in a cancer pain population. J Pain Symptom Manag. 1988;3:S24.
- [Google Scholar]
- Self-Reported Drug use and Urinalysis Results. 2004. Available from: http://www.ijpp.com http://imsear.hellis.org/handle/123456789/106326 [Last accessed on 2019 May 23]
- [Google Scholar]






