Translate this page into:
Palliative Surgery for Advanced Cancer: Clinical Profile, Spectrum of Surgery and Outcomes from a Tertiary Care Cancer Centre in Low-Middle-Income Country

*Corresponding author: S. V. S. Deo, Department of Surgical Oncology, All India Institute of Medical Sciences, New Delhi, India. svsdeo@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Deo SV, Kumar N, Rajendra VK, Kumar S, Bhoriwal SK, Ray M, et al. Palliative surgery for advanced cancer: Clinical profile, spectrum of surgery and outcomes from a tertiary care cancer centre in low-middle-income country. Indian J Palliat Care 2021;27(2):281-5.
Abstract
Objectives:
Palliative surgery for cancer plays an important role in the overall management, especially in low-middle countries with a significant burden of advanced cancers. There is a paucity of literature related to the field of palliative surgery. In this study, we present the clinical spectrum, profile of surgical interventions and outcomes of palliative surgical procedures performed at a tertiary cancer centre involving multiple organ systems.
Materials and Methods:
A retrospective analysis of prospectively maintained surgical oncology database of a tertiary care cancer centre was performed. Patients fulfilling the criteria of palliative surgery were analysed for clinical spectrum, indications for surgery, palliative surgical procedures and post-operative outcomes.
Results:
A total of 678 out of 8300 patients fulfilled the criteria for palliative surgery. Palliative surgical procedures were performed most commonly for gastro-oesophageal malignancies (36.4%) followed by colorectal cancers (24%) and breast cancer (12%). Palliative mastectomy was the most common procedure performed for advanced breast cancer and 7% of sarcoma patients had amputations. Symptom relief could be achieved in 80–90% of patients and post-operative morbidity was relatively high among hepatobiliary, gastrointestinal and gynaecological cancer patients.
Conclusion:
Globally, a significant number of cancer patients need palliative surgical intervention, especially in LMIC with a high burden of advanced cancers. Results of the current study indicate that gastrointestinal cancer patients constitute a major proportion of patients undergoing palliative surgery. Overall results of the current study indicate that excellent palliation can be achieved in majority of patients with acceptable morbidity and hospital stay.
Keywords
Palliative surgery
Advanced malignancy
Outcomes
INTRODUCTION
Cancer is one of the leading causes of mortality globally and cancer care involves many forms of treatment intended for either cure or palliation. According to the WHO, each year an estimated 40 million people are in need of palliative care, 78% of whom live in low- and middle-income countries.[1]
Surgery plays an important role in the overall management of cancer. Majority of early solid tumours can be potentially cured with surgery, however, a significant number of advanced cancer patients require some form of surgical intervention for palliation of symptoms. The importance of palliation of cancer symptoms has received increasing attention in recent years and the field of palliative care is gaining increasing recognition. Surgeons are alleviating the suffering of cancer patients knowingly or unknowingly since the late 18th century, however, there is a lack of consistent and uniform policy of defining palliative surgery and its outcomes.[2] Conventionally palliative surgery is defined as ‘surgery performed for relief of symptoms caused by advanced cancer not amenable for cure’ and some surgeons also include the presence of gross residual malignant disease at completion of surgery as palliative surgery.[3,4] Palliative cancer surgery plays an important role in the overall cancer management, especially in developing countries with a significant burden of advanced cancers. There is a paucity of literature related to the field of palliative surgery and there is a need to encourage clinical studies and publications pertaining to palliative surgery. In this study, we present the clinical spectrum and outcomes of palliative surgical procedures performed at a high-volume tertiary cancer centre in India.
MATERIALS AND METHODS
This study was approved by the Institute Ethical Committee. A retrospective analysis of prospectively maintained surgical oncology database of a tertiary care cancer centre was performed. The department caters to a broad spectrum of cancers involving different organ systems including breast, extremities, gastrointestinal, head and neck, thoracic and genitourinary tract. A total of 8300 major cancer surgeries were performed between 2007 and 2015 including both curative and palliative surgeries. For the purpose of the study, palliative surgery was defined as ‘surgery performed for relief of cancer-related symptoms in patients with advanced and incurable cancers.’ Advanced malignancy was defined as the presence of locally advanced incurable disease or presence of distant metastasis at the time of operation. The indications for surgery included fungation, intractable pain, obstruction, bleeding or perforation due to tumours. R-2 resections and pulmonary and hepatic metastectomies performed with curative intent were excluded from the analysis.
A descriptive analysis of palliative surgery data was performed for frequency, the pattern of organ system involvement, clinical indications for palliative surgery, types of surgical procedures, post-operative hospital stay and procedure-related morbidity.
RESULTS
A total of 678 patients out of 8300 met the criteria for major palliative surgery and were included for analysis. The frequency of organ system involvement and indications for palliative surgery are shown in Table 1. Palliative surgical procedures comprised 8.2% of all major surgeries performed during the study period. Palliative surgical procedures were performed most commonly for gastro-oesophageal malignancies (36.4%). The most common indication was absolute dysphagia due to the advanced presentation of oesophageal cancer. Most of the gastric cancer patients presented with gastric outlet obstruction. The second most common indication for palliative surgery is colorectal cancer presenting with intestinal obstruction. Fungating and ulcerated tumours with or without bleeding were the most common indications for palliative surgery among breast cancer patients. Among patients with gynaecological malignancies, the majority of ovarian cancer patients presented with intestinal obstruction whereas malignant rectovaginal fistula was the most common indication for palliative surgery in patients with cervical cancer. Fifty-two patients of metastatic musculoskeletal malignancies underwent palliative surgical procedures mainly for fungating painful masses involving extremities. The most common indication for palliative surgery among patients with head-and-neck cancers was dysphagia followed by airway obstruction. The surgical obstructive jaundice with pruritis was most common indication for palliative surgery in patients with hepatopancreaticobiliary malignancies. Table 2 shows different types of palliative surgical interventions. Majority of the patients with oesophageal cancer patients with dysphagia had feeding jejunostomy. Two-thirds of the patients with gastric cancer underwent palliative gastrojejunostomy and palliative gastric resection was performed in remaining patients. Diversion stoma was the most common palliative procedure performed in colorectal cancer patients and colonic resections were performed in remaining patients. Palliative mastectomy was the most common procedure performed for advanced breast cancer patients and 12% of these patients required flap reconstruction for soft-tissue defect closure. Majority of the gynaecologic malignancy patients required diversion ostomy or intestinal bypass procedures for palliation of intestinal obstruction or fistulae. Amputation or disarticulation as palliative surgical intervention was performed for extremity sarcoma patients and majority of retroperitoneal sarcoma patients had palliative debulking surgery. As far as head-and-neck cancer patients are concerned, entral feeding procedures or tracheostomy for airway obstruction were the most common palliative surgical procedures performed.
| Type of cancer (%) | Indications for palliative surgery |
|---|---|
| Gastro-oesophageal cancers (36.3%) | Dysphagia – 70% Gastric outlet obstruction – 30% |
| Colorectal cancers (24%) |
Obstruction – 83.4% Bleeding – 4.9% Incontinence – 4.9% Perforation – 3.6% Pain (0.6%) Recto vaginal fistula (0.6%) |
| Breast cancer (12%) | Infected ulcer (42.8%) Fungating mass (27.3%) Breast mass with intractable pain (17.9%) Bleeding (8.3%) Mass/ulcer in axilla (3.5%) |
| Gynaecological cancers (10%) | Intestinal obstruction (59.4%) Malignant rectovaginal fistula (37.6%) Malignant ileovaginal fistula (1.4%) Radiation-induced rectal perforation (1.3%) Bleeding (1.3%) |
| Musculoskeletal cancers (7.2%) | Fungating tumours (50%) Bleeding tumours (15.3%) Tumours causing deformity and intractable pain (23.1%) Abdominal mass, pain, obstruction (11.6%) |
| Head-and-neck cancers (6.2%) | Dysphagia (73.6%) Airway obstruction (26.4%) |
| Hepatobiliary cancers (4.1%) | Obstructive jaundice (68.8%) Gastric outlet obstruction (21.9%) Intractable pain (9.3%) |
| Type of cancer | Palliative surgical procedures |
|---|---|
| Breast cancer | Simple mastectomy (35.7%) Modified radical mastectomy (58.3%) Wide excision of local recurrence (5.9%) |
| Colorectal cancers | Diversion ostomy (69.9%) Resection and anastomosis/bypass (18.4%) Abdominoperineal resection (1.8%) Hemicolectomy (8.6%) Intrathecal drug delivery pump implant (1.2%) |
| Gynaecological cancers | Ileostomy (34.7%) Colostomy (47.9%) Bypass procedures (13%) Resection (4.4%) |
| Gastro-oesophageal cancers | Feeding jejunostomy (65.6%) Gastrojejunostomy (25.1%) Gastrectomy (4.5%) Feeding gastrostomy (4.8%) |
| Musculoskeletal cancers | Amputations (48.1%) Disarticulations (15.4%) Wide excision (17.3%) Debulking surgery (19.2%) |
| Head-and-neck cancers | Feeding jejunostomy (47.6%) Feeding gastrostomy (26.2%) Tracheostomy (26.2%) |
| Hepatobiliary cancers | Biliary bypass procedures (62.5) Gastrojejunostomy (12.5%) Triple bypass (15.6%) Intrathecal drug delivery pump implant (9.3%) |
Figure 1 shows outcomes of palliative surgery. Post-operative stay was approximately 2 days for breast cancer patients and 7.8 days for hepatobiliary cancer patients. Patients with other organ system cancers had hospital stay ranging between 4 and 5 days. Post-operative morbidity was relatively high among hepatobiliary, gastrointestinal and gynaecological cancer patients most of the patients experiencing wound infection or wound dehiscence. Overall, majority of patients had significant symptom relief following palliative surgery.
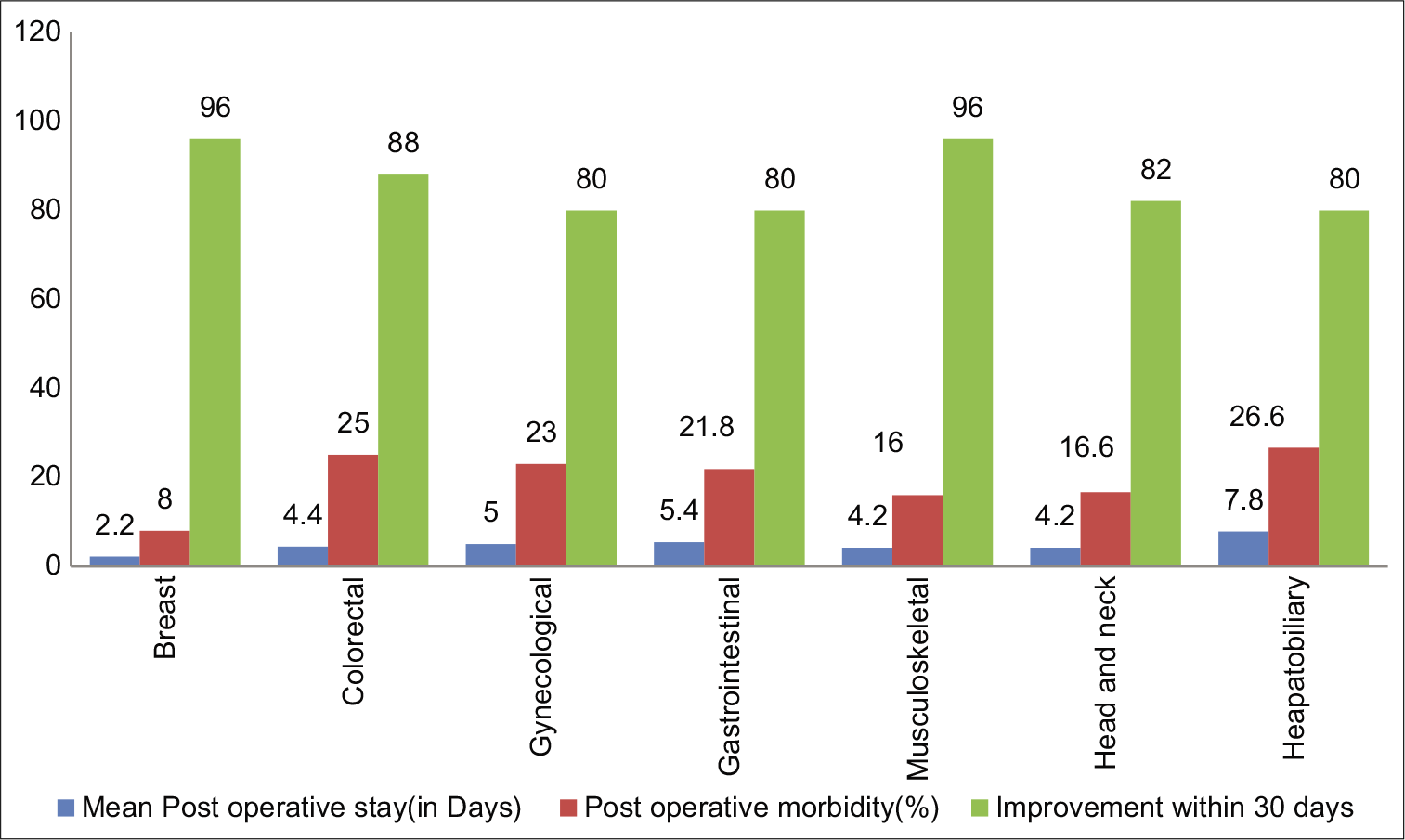
- Post-operative hospital stay, morbidity and symptom improvement rate.
DISCUSSION
Conventionally, surgery played an important role in the field of palliative medicine with numerous examples of surgical interventions for terminal and distressing symptoms suc as pain, bleeding and obstruction involving various organ systems.[5] Palliative surgery is mainly directed toward alleviating symptoms and suffering and improving quality of life (QOL), whether or not treatments are being directed at modifying the underlying disease or prolonging life.[6] However, the field of palliative surgery has not received due attention or recognition it deserved. There are grey areas in the field of palliative surgery which includes the definition of palliative surgery, indications and timing of palliative surgery and standardisation of outcomes measures. A number of international surgical organisations have started paying attention to the field of palliative surgery in the recent past and attempts are being made to mainstream palliative surgery in the surgical training and curriculum.[7]
Review of surgical literature reveals paucity and heterogeneity of publications related to palliative surgical field.[5] There is a need to have a comprehensive and standardised database of palliative surgical procedures performed in cancer centres across the world including LMICs. The current study included palliative surgery data related to multiple organ systems and analysed data related to pertinent issues of palliative surgical field.
The current study was conducted in a high-volume tertiary care cancer centre from a LMIC and the results indicate that approximately 8% of cancer patients had palliative surgery across all organ systems. Multiple factors influence rates of palliative surgery of a hospital, including presence of a dedicated palliative care service, availability of non-surgical palliative interventions including palliative chemotherapy, radiotherapy and interventional radiology and last but not the least a committed and experienced surgical oncology team.
As far as the frequency of organ systems is concerned, gastrointestinal cancers constituted 60% of the palliative surgical procedures predominantly involving gastroesophageal and colorectal cancers. This may be a reflection of the nature of disease causing gastrointestinal tract obstruction resulting in a need for surgical intervention as revealed by the indication and symptom of presentation in the current study. In a retrospective study by Badgwell et al., gastrointestinal obstruction (43%) was the most common indication followed by wound infections and local complications (10%), whereas in a prospective study, Podnos et al. had shown that pain is the most common indication for palliative surgery.[8,9] Malignant bowel obstruction (MBO) is a challenging clinical situation of advanced cancer with several pathophysiologic mechanisms. The treatment of MBO requires a collaborative approach of surgical, interventional and medical specialists. Watt et al. in a systemic review of various published articles showed the role of self-expanding metallic stents as an alternative option for surgery, however, due to lack of availability of expertise and cost factors, majority of gastrointestinal and gynaecological cancer patients had ostomies, especially in LMIC.[10] Next most common group of patients undergoing palliative surgery was breast cancer. During the past decade, breast cancer has replaced cervical cancer as leading cancer among women in LMIC and locally advanced (Stage III) and metastatic (Stage IV) breast cancer comprises 70–80% of breast cancer load.[11] A significant number of these patients have no access to chemotherapy or radiotherapy and a good proportion of these patients needs a palliative mastectomy to improve QOL. Results of the current study indicate that ulcerated and fungated breast cancers are the most common indication for palliative mastectomy.[12,13] Gynaecological cancers including cervical and ovarian cancer are the next most common cancers requiring palliative surgery mainly for malignant rectovaginal fistulae and MBO. These conditions are difficult to treat and diversion colostomy is the most common surgical procedure performed in this group of patients. Head-and-neck cancer is one of the common cancers in LMIC and majority present in Stage III or IV not amenable for curative therapy. In the current study, head-and-neck cancers constituted 11% of patients, and dysphagia and airway obstruction are the common symptoms needing palliative intervention. Recently, percutaneous endoscopic gastrostomy has emerged as a preferred option for enteral feeding in head-and-neck cancer patients, however, due to non-availability of expertise, cost factors and advanced stage of growth precluding endoscopy, majority of head-neck cancer patients in LMIC undergo a surgical feeding gastrostomy or a jejunostomy as shown in the current study.[14] A subset of extremity sarcoma patients presenting with advanced growth and lung metastases sometime need palliative amputations for relief of intractable and severe pain not responding to medications and rarely for fungation and bleeding. Advanced hepatobiliary cancers comprised 4% of patients undergoing palliative surgical intervention mainly for obstructive jaundice and duodenal obstruction. Advances in the field of therapeutic endoscopy, stenting and interventional radiology have revolutionised the management of malignant surgical obstructive jaundice and a very small percentage of patients require surgical intervention in the current era.[15]
Surgical outcome assessment is extremely important in the field of palliative surgery as the main goals of intervention include, relief of symptoms, minimise hospital stay improve QOL without adding significant surgical morbidity. Hospital stay reported in the current study ranged between 2 and 8 days with breast cancer patients requiring a minimum hospital stay and patients with hepatobiliary and gastrointestinal cancers requiring a longer hospital stay. Overall, 24% of patients had perioperative morbidities in the current study mostly in the form of wound complications. Review of literature shows morbidity for palliative surgery ranging between 25 and 40%.[8,16,17] As far as symptom resolution is concerned, we could achieve a good symptom relief in 80–90% of patient population, with high rates being reported among breast and sarcoma patients and moderate rates among hepatobiliary and gynaecologic cancer patients.
CONCLUSION
Results of the current study indicate that gastrointestinal cancer patients constitute a major proportion of patients undergoing palliative surgery followed by breast, gynae and head-and-neck cancers. Tumour ablation was main operative approach among breast and extremity sarcoma patients whereas tube placement, bypass or diversion procedures were common among gastrointestinal, head-and-neck and gynaecologic cancer patients. Overall results of the current study indicate that excellent palliation can be achieved in majority of patients with acceptable morbidity and hospital stay.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Available from: https://www.who.int/news-room/fact-sheets/detail/palliative-care [Last accessed on 2020 Aug 02]
- Decision making on surgical palliation based on patient outcome data. Am J Surg. 1999;177:150-4.
- [CrossRef] [Google Scholar]
- Indications and use of palliative surgery-results of society of surgical oncology survey. Ann Surg Oncol. 2002;9:104-12.
- [CrossRef] [Google Scholar]
- Palliative Care in Surgery: Defining the Research Priorities. Ann Surg. 2018;267:66-72.
- [CrossRef] [Google Scholar]
- Education about death and dying during surgical residency. Am J Surg. 1991;161:690-2.
- [CrossRef] [Google Scholar]
- Surgery, palliative care, and the American College of Surgeons. Ann Palliat Med. 2015;4:5-9.
- [Google Scholar]
- Indicators of surgery and survival in oncology inpatients requiring surgical evaluation for palliation. Support Care Cancer. 2009;17:727-34.
- [CrossRef] [Google Scholar]
- Surgical palliation of advanced gastrointestinal tumors. J Palliat Med. 2007;10:871-6.
- [CrossRef] [Google Scholar]
- Self-expanding metallic stents for relieving malignant colorectal obstruction: A systematic review. Ann Surg. 2007;246:24-30.
- [CrossRef] [Google Scholar]
- Changing indications for surgery in patients with stage IV breast cancer: A current perspective. Cancer. 2008;112:1445-54.
- [CrossRef] [Google Scholar]
- Head and neck cancer patients' perceptions of quality of life and how it is affected by the disease and enteral tube feeding during treatment. Ups J Med Sci. 2015;120:280-9.
- [CrossRef] [Google Scholar]
- Current status of percutaneous transhepatic biliary drainage in palliation of malignant obstructive jaundice: A review. Indian J Palliat Care. 2016;22:378-87.
- [CrossRef] [Google Scholar]
- Surgical palliation at a cancer center: Incidence and outcomes. Arch Surg. 2001;136:773-8.
- [CrossRef] [Google Scholar]
- A prospective, symptom related, outcomes analysis of 1022 palliative procedures for advanced cancer. Ann Surg. 2004;240:719-26.
- [CrossRef] [Google Scholar]






