Translate this page into:
Parents' Knowledge and Attitude Regarding Their Child's Cancer and Effectiveness of Initial Disease Counseling in Pediatric Oncology Patients
Address for correspondence: Dr. Manjusha Nair, PRA-19, Prasanth, Pathirappally Road, Poojappura P. O, Trivandrum, Kerala, India. E-mail: drmanjushanair@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To examine parent's knowledge, attitude and psychosocial response regarding their child's cancer and treatment after initial disease counseling by doctor.
Materials and Methods:
Structured questionnaire based study of 43 mothers of newly diagnosed pediatric cancer patients undergoing treatment in pediatric oncology division. Mothers received initial counseling regarding their child's cancer and treatment from the doctor. Questionnaire was administered 2-6 months after initial counseling and mothers self-reported their responses.
Results:
83% mothers had school level education only and 84% belonged to lower and middle socio-economic status. More than 80% mothers knew the name of their child's cancer, type of treatment received by child and approximate duration of treatment. 93% knew regarding painful procedures and 84% mothers reported knowledge about chemotherapy side effects. Hope of cure and satisfaction with treatment were reported by 90% mothers. 81% mothers reported high levels of anxiety and 66% worried regarding painful procedures. As high as 60% of parents were afraid to send their child outside to play and 40% were afraid to send their child to school. 40% mothers wanted more information regarding child's higher education, married life & fertility. On statistical analysis, mother's age, educational status or family background did not influence their knowledge and attitude.
Conclusion:
Relevant information about child's cancer and treatment can be imparted effectively even to mothers with school level education. This knowledge helps to instill hopeful attitude, confidence and satisfaction in parents. Anxiety and fear related to cancer persists in mothers even after the initial stress period is over. Pain related to injections and procedures is a major concern in parents. Involvement of counselor in the treating team is desirable to overcome these problems.
Keywords
Counseling
parents' knowledge and attitude
pediatric oncology
BACKGROUND
Cancer continues to be a stigma in our society, and knowledge regarding pediatric cancer is almost nonexistent among the general population. The psychological, social, and financial impact of their child being diagnosed with cancer is devastating for majority of the parents. Treatment often involves painful procedures, long hospital stays, restrictions imposed on food and activities, side effects of antineoplastic therapy, and chronicity of disease, and imparts psychological burden on child and his/her family. Studies have supported the view that providing psychological and emotional support to the cancer-affected children and their family through their time of crisis adds enormously to the effectiveness of treatment. Screening of parents and families on factors known to be predictive of ongoing psychological difficulties, emotional demand, and response can help us anticipate the adjustment problems and provide means for quickly and effectively giving care to families on the basis of their needs.
Kerala being a state with high literacy rates, health indices, and health awareness, combined with less number of children per family, we would expect that higher educational status of parents would influence their emotional responses. At Regional Cancer Centre, we see around 600 new pediatric cancer patients in a year, of which leukemias are the most common. Comprehensive and state-of-the-art diagnostic facilities, medical treatment, and supportive care are rendered for pediatric oncology patients in our institution. However, there exist lacunae as far as providing effective emotional and psychological support is concerned. We feel that it is important for us to identify parent's psychosocial impact of their child's disease, to understand their responses, and to identify appropriate support systems which will help them cope with their problems.
MATERIALS AND METHODS
A study was carried out to assess mothers' knowledge of their child's cancer and treatment after initial disease counseling, to examine their attitude and psychosocial responses after a brief period, and thereby assess the effectiveness of the initial counseling. Mothers of 43 newly diagnosed pediatric cancer patients undergoing treatment in pediatric oncology division were invited to be part of this study during one of their hospital visits. Initial counseling about diagnosis and treatment was provided to all parents as is the standard practice, wherein information regarding name of the cancer, type and duration of treatment, side effects of chemotherapy, risk of relapse, and need for supportive care was communicated to them in a single session. A time frame of 2–6 months from diagnosis was arbitrarily decided to allow for mothers to get over the acute posttraumatic stress period and for completion of intensive phase of chemotherapy when complications are more frequent. After this period, mothers were provided a structured questionnaire containing simple questions in Malayalam and requested to self-report their responses. Written informed consent was obtained from the participants before conducting and recording the interviews. Non-Malayalam speaking parents and those with sick children or with recurrent/relapsed disease were excluded from the study. The responses were analyzed using statistical tests of significance.
Designing of questionnaire
Questions were generated based on commonly shared doubts and queries of parents of children attending the pediatric oncology division during the previous few years and in consultation with experienced doctors. Themes discussed in the questionnaire included parents' perception of their child's illness (what is their child's disease, what according to them likely caused it, etc.), knowledge responses (medical name of their child's cancer, type of treatment given, duration of treatment, knowledge about painful procedures, side effects of medication, risk of relapse, etc.), and attitude responses (hope of curability, satisfaction with treatment, anxiety regarding child's future, studies, play, etc.). The questions were simplified to close-ended entities with yes/no responses. Content validity was checked by two pediatric oncologists and approved after expert opinion. Translation to Malayalam was done by the social worker and back-translation was performed to eliminate confusing or vague terms. The questionnaire was then piloted on five parents who were not part of the study for assessing comprehensibility.
RESULTS
Demographics
Mothers of 36 leukemia patients, 3 non-Hodgkin's lymphoma patients, and one each brain tumor, neuroblastoma, Ewing's sarcoma, and synovial sarcoma were studied. Majority of mothers (36 out of 43) had school-level education (12th class or less) while only a few were graduates or postgraduates. Thirty mothers (70%) were younger than 35 years of age. Thirty-six mothers (84%) belonged to lower socioeconomic status. Twenty-six mothers (61%) came from nuclear families while 17 mothers had the support of joint family.
Knowledge responses
Thirty-eight out of 43 mothers (88%) knew the name of their child's cancer, 34 mothers (79%) knew the type of treatment received by child, and 39 mothers (90%) were aware of the approximate duration of treatment. 40/43 mothers (93%) knew that their child would be subjected to painful procedures such as lumbar puncture (LP)/bone marrow examination and 35 mothers (81%) were aware that these procedures would be repeated multiple times during the course of treatment. All parents were aware of the common side effects of treatment such as nausea, vomiting, and hair loss and 36 mothers (84%) reported knowing about serious side effects such as bleeding or life-threatening infection.
Attitude responses
Hopeful attitude of getting cure with treatment and satisfaction with present treatment were reported by a high number of mothers (90%). Thirty-five mothers (81%) reported being preoccupied with thoughts regarding their child's disease and having high levels of anxiety. Twenty-seven mothers (62%) were worried regarding painful injections and 28 mothers (66%) regarding painful procedures. Only eight mothers (20%) reported being worried about nausea and vomiting related to chemotherapy. Ten mothers (25%) felt that their child knew about his/her cancer; however, not a single parent wanted their child to be told regarding the same, reasons being that child would become afraid, depressed, may not co-operate with treatment, or may become difficult to handle. As high as 60% of parents were afraid to send their child outside to play and 40% were afraid to send their child to school. Interestingly, 40% of parents wanted more information regarding their child's higher education, married life, and fertility.
Statistical analysis
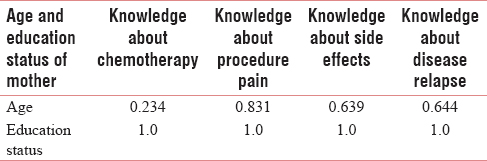
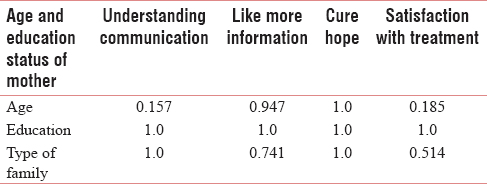
On univariate analysis, mothers' age, educational status, or family background did not have significant association with their knowledge and attitude [Tables 1 and 2].
DISCUSSION
Cancer diagnosis in a child is associated with negative emotions such as fear, anxiety, uncertainty, stress, depression, and guilt. Moreover, most families tend to crash down from feeling safe and in control of their lives to living with vulnerability and insecurity. The emotionally charged nature and demands of treatment such as invasive procedures, frequent hospitalizations, side effects of drugs, and disruption of daily routine lead to coping problems and disequilibrium in many families.[1] In our society, the major factor which dissuades the general parent from seeking information and awareness regarding childhood cancer is the stigma itself. Parents feel that even speaking about cancer in relation to their child is associated with misfortune, and they make their own assumptions based on experience in their family members or advice given by acquaintances or mere hearsay. Added on to this is the traditional paternalistic pattern of physician–patient relationship in our country, which puts a barrier for most parents to talk openly about the disease as well as their queries to their doctor. Hence in societies like ours, the need of the hour is for the medical fraternity to go proactively into the parents' psychological realm and provide correct and scientific information in a gentle manner that can be absorbed by them.
Parental fear and anxiety arise mostly due to lack of knowledge about the disease and treatment, association of cancer with incurability, pain and death, and the accompanying uncertainty. In a qualitative research study among mothers of cancer-affected children in Iran, the authors found that inadequate knowledge of disease, treatment, and complications is the main challenge among mothers of children with cancer. They also report that it may influence other aspects such as psychological problems and social communications, and may even lead to lack of trust in health-care team and lack of children's co-operation with treatment.[2] In fact, parental stress has been identified as an independent predictor of children's emotional, behavioral, and social adjustment.[3]
Studies have shown that most parents of children with cancer demonstrate reasonably good levels of cancer knowledge as they course through their child's treatment. Mack et al. determined that there is tendency on the part of providers to withhold upsetting information despite the parents' desire for truthfulness, because of concern that knowing more about disease will lead to increased fear.[4] A study among Hong Kong Chinese families suggested that knowing more about disease did not necessarily result in increased fear among parents.[5] On the other hand, providing adequate information has found to reduce uncertainty and help parents regain a sense of control over the situation pertaining to their child's illness, thus facilitating better coping.
Much research has been done to evaluate whether educational status of parents influences their cancer knowledge and adjustment skills, and there are results favoring both ways. A study from Malaysia showed that parents with higher level of education showed better cancer knowledge, and had lesser stress and anxiety.[5] A few studies evaluating the impacts of education and socioeconomic status of parents on pediatric cancer survival rates have shown that these constructs may influence treatment understanding and risk for psychological distress.[6] Contrary to this, other researchers have found that mothers' education level was not significantly correlated with cancer-related stress.[7] A study linking cancer knowledge and problem-solving ability of mothers demonstrated that, even though cancer knowledge was significantly associated with educational level of the parent, it did not contribute to the variance in psychological adjustment such as depression and mood states or problem-solving ability.[5]
All mothers included in our study had at least primary education, confirming the high female literacy rate in our state, which has contributed to the better health awareness and higher health indices when compared to the rest of the country. We compared age of mothers and family background because they influence an individual's psychosocial response. With increasing age comes emotional maturity and life experience, and we would expect older mothers and those hailing from joint families to have more receptive attitude and better coping skills. When we analyzed these factors in our study sample using tests of significance, we found that parents' age, education status, or type of family did not influence their knowledge, attitude, and psychosocial response. Similar inferences were reported in a comprehensive review of ninety papers from world over focusing on psychosocial impact of parents of cancer-afflicted children, in which aspects such as educational level, socioeconomic status, and sociodemographic variables were not associated with better or worse psychological conditions of parents.[1]
We found that, after adequate time for getting over the initial shock and stress of cancer diagnosis, almost all mothers demonstrated hopeful attitude for cure and satisfaction with treatment. This may be because their children were clinically stable, were tolerating the treatment without much problems, and had gotten relief from their initial symptoms.
Previous research has demonstrated that the negative effects of the stress of dealing with a child's cancer are multifactorial and persist long after the initial shock of the diagnosis. Dolgin et al. found different patterns of the manifestation of symptoms 6 months after treatment: high levels of symptoms at the time of diagnosis, which declined over time, moderate symptomatology over a period of 6 months, and low levels that remain from the time of the diagnosis.[8] But in our mother cohort, high anxiety levels were demonstrated even after enough time for initial adjustment had elapsed, suggesting that magnitude and duration of posttraumatic stress disorder may be higher than what we anticipate. Disease information, child's physical condition, pain related to procedures, and side effects of treatment have been identified as crucial stressors for parents over the course of child's treatment.[1] In our mother cohort also, procedures and procedure-related pain were reported as major sources of anxiety in over 60% of the participants. Acceptance of common side effects of treatment was also high among mothers, only a minority of them reported concern regarding these. We also found that, out of their fear and anxiety, most of the mothers wanted to restrict the child's outdoor activities and attending school for fear of catching infection. Even well-educated mothers were afraid to send the child to play outdoors. In our statistical analysis, we found that mothers' educational or socioeconomic status did not influence their attitude responses.
Apart from the assessment of knowledge and attitude of mothers in this cohort, we were able to assess indirectly the effectiveness of our initial counseling. We found that, with the amount of information that was given in the initial counseling session by the doctor, most of the mothers were able to reciprocate satisfactory knowledge about disease and treatment including serious side effects. A good majority of them also demonstrated awareness regarding painful procedures such as bone marrow and LP, and that these needed to be done multiple times during treatment. Even though the chance of disease relapsing after treatment was communicated to them initially itself, only a third of them acknowledged knowing this. This may be part of selective retaining of positive information and building of hope of cure because of clinical improvement in condition of the child. Hence, we concluded that adequate disease information was imparted to mothers at the start of treatment itself without unnecessarily alarming them. We were also able to identify gaps and lacunae in our initial counseling. A good percentage of mothers wanted more information regarding the child's physical and mental growth, prospects of education and employment, and married life. Though these aspects may seem less important to clinicians for the purpose of treatment, there are issues which are close to a mother's heart, and we feel that these need to be addressed in the initial counseling itself.
CONCLUSIONS
This study indicates that child's disease-related stress and anxiety persist in many parents even after acute period of adjustment to stress is over. A good amount of relevant information about cancer and its treatment can be imparted in simple language even to parents with school-level education, and this may help their psychosocial response in a positive manner. Parental knowledge about disease and various aspects of treatment may help in allaying disease-related threat and make them more confident and co-operative toward staff. Pain related to injections and procedures is a major concern in parents. Even if prognosis of cancer is good, parents remain vulnerable to psychological distress despite child's stable clinical condition. This reveals the unmet areas of psychological needs of parents for which involvement of counselor as part of treating team may be beneficial.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Psychosocial impact of pediatric cancer on parents: A literature review. Paidéia. 2012;22:119-29.
- [Google Scholar]
- Challenges of children with cancer and their mothers: A qualitative research. Iran J Nurs Midwifery Res. 2014;19:334-9.
- [Google Scholar]
- Communication about prognosis between parents and physicians of children with cancer: Parent preferences and the impact of prognostic information. J Clin Oncol. 2006;24:5265-70.
- [Google Scholar]
- Psychological distress and associated factors in parents of children with cancer. Int J Soc Sci Humanity. 2011;1:37-42.
- [Google Scholar]
- Factors affecting maternal coping in Korean mothers of children with cancer. Open J Nurs. 2016;6:751-66.
- [Google Scholar]
- Childhood cancer in context: Sociodemographic factors, stress, and psychological distress among mothers and children. J Pediatr Psychol. 2015;40:733-43.
- [Google Scholar]
- Trajectories of adjustment in mothers of children with newly diagnosed cancer: A natural history investigation. J Pediatr Psychol. 2007;32:771-82.
- [Google Scholar]
Questionnaire
Pro forma for Analysis of Knowledge and Attitude of Parents of Children Affected with Cancer
Name of child:
Age: _________ Male/Female: _________
Diagnosis:
Date of diagnosis: _________
Date of interview: _________
General Information:
Primary caretaker: Mother/father/grandparent/aunt/uncle/elder sibling/others
Age of father: _________ Educational status: ________
Age of mother: _________ Educational status: ________
Birth order of this child:
Family structure: _________ Joint/nuclear/extended/broken
Place of domicile: _________ Rural/urban
Employment of parent: _________unemployed/unskilled/skilled/semi.professional/professional
House: _________own/rented/labor camp/slum
Family history of cancer: _________Yes/No
No. of siblings:
Age: _________ Sex: _________
Parent's perception about child's disease:
Do you know what disease your child has?: _________Yes/No
What was your first reaction on hearing the diagnosis?
Shock/disbelief/numbness/fear/denial/anger/helplessness
Duration of child's illness before diagnosis_________<2 weeks/2.8 weeks/>8 weeks
Is there any delay in consulting doctor after the onset of problems?: _________ Yes/No
If yes, reason for delay: ignorance/tried self.medication/family issues/economic problems
According to you, why is you child having cancer? _________ My fault/spouse's fault/God's curse/unknown cause/family member has cancer.
Parents' knowledge about their child's disease and treatment:
Knows medical name of child's cancer: _________Yes/No
Knows about names of medicines (at least some): _________ Yes/No
Knows about duration of treatment: _________Yes/No
Knows about painful procedures (LP, bone marrow, etc.): _________Yes/No
Knows about curability with treatment: _________ curable/incurable
Knows that cancer can re.occur: _________Yes/No
Knows about the common side effects of treatment (nausea, vomiting, hair loss): _________Yes/No
Knows about serious side effects (bleeding, major organ dysfunction, infection): _________Yes/No
Do you have difficulty in understanding the information received? _________Yes/No
Do you think that the child knows about the disease? _________Yes/No
Should child be told about the disease? _________Yes/No
If yes, who should tell him/her? _________Doctor/nurse/parents/others
If No, give reason _________ may get frightened/may get depressed/may not co.operate with treatment/may become unmanageable
Attitude Responses
Do you feel anxiety about needle pricks/pain? _________Yes/No
Do you feel anxiety about LP/bone marrow tests? _________Yes/No
Do you worry about child's disease? _________Most of the time/sometimes/not very often
Do you worry that treatment is not working? _________Most of the time/sometimes/not very often
Do you worry about medicine's side effects? _________ Most of time/sometimes/not very often
Do you worry that child's cancer will come back? _________Most of time/sometimes/not very often
Are you afraid of letting child play/run? _________ Yes/No
Are you afraid of sending child to school? _________Yes/No
Are you afraid that other siblings will get cancer? _________Yes/No
Are you worried about future of the child? _________Yes/No
If Yes, specify: _________ Studies/marriage/social stigma/disease recurrence/hereditary
Do you think that you know all the necessary information about your child's illness and treatment? _________Yes/No
If No, what additional information would you like? _________About disease/about medicines/about child's education/about child's marriage, etc
Would you like to have written information about child's disease and treatment? _________Yes/No
Are you satisfied with present hospital treatment? _________Yes/Partially/No
If not yes, give reason _________
What will you do when you have doubts? _________Ask doctor/ask staff/ask other parents/ask relatives/consult Internet
What gives you more relief when you feel stressed? _________Praying to God/seeking help from family members/talking to staff/talking to other parents/support of friends/considering as fate.






