Translate this page into:
‘Patients with Cancer are Distressed!’ Indian Healthcare Provider Perspectives on Distress Screening and Referrals to Psycho-oncology Services – A Mixed Methods Study
-
Received: ,
Accepted: ,
How to cite this article: Normen M, Sahaya FE, Kulkarni K, Vidhubala E, Shewade HD, Kathiresan J. ‘Patients with cancer are distressed!’ Indian healthcare provider perspectives on distress screening and referrals to psycho-oncology services – A mixed methods study. Indian J Palliat Care 2021;27:561-70.
Abstract
Objectives:
Routine screening for distress is a guideline prescribed by the National Comprehensive Cancer Network (NCCN) to adequately assess distress in a cancer setting. Our centre conducted routine screening but failed to utilize psycho-oncology services. Our aim was to assess the extent of self-reported distress, referrals to psycho-oncology services and healthcare provider perspectives about the existing distress management system and psycho-oncology services.
Materials and Methods:
We conducted a record review of adult patients (n=372) who reported to the Out-patient department of the tertiary cancer centre. Semi-structured interviews were conducted with fourteen healthcare providers. We used a concurrent mixed methods study design. Adult patients were screened for distress using NCCN-Distress Thermometer and problem checklist. Healthcare providers from different oncology specialties were interviewed and the data was analysed using descriptive thematic analysis.
Results:
Patients screened for distress were found to report moderate to extreme levels of distress (53.5%). The total referrals to psycho-oncology support services were low (8.6%). Interviews with healthcare providers revealed three major themes: Enablers, barriers and solutions for utilization of distress management system and psycho-oncology services.
Conclusions:
Moderate to extreme distress was found among patients routinely screened for distress, although there was poor utilization of distress management system and psycho-oncology support services due to time constraints, patient’s negative attitudes towards mental health referrals, generic screening tools and use of own clinical judgement to make referrals by healthcare providers. Future research warrants implementation of strategies to integrate psycho-oncology services into routine cancer care by focusing on improving visibility of services.
Keywords
Psycho-oncology
Outpatients
Healthcare Personnel
Referrals
Mental Health
Distress
Screening
INTRODUCTION
Patients with cancer often experience distress at various periods throughout the disease trajectory.[1] Distress is regarded as the sixth vital sign and routine screening procedures followed are often based on guidelines provided by National Comprehensive Cancer Network (NCCN).[2] The American College of Surgeons’ Commission on Cancer, established new accreditation standards for patient-centred care that included Standard 3.2, a mandate requiring that all patients be screened for distress and that there be an appropriate clinical response when patients are identified as distressed.[3] If left unaddressed, psychosocial distress can interfere with treatment, adversely affecting the course of the disease and outcomes.[4,5]
Prompt diagnosis and management of cancer-related distress can result in improved care, better provider-patient communication and efficient utilisation of the entire healthcare team which is a prerequisite for best outcomes for patients.[6] Many tools have been constructed and used in a variety of psychosocial oncology programs to measure distress although shorter distress screening tools (5–20 items) were found to have better chances of being used in busy clinical settings.[7,8]
In India, multiple studies have documented the prevalence of distress and the need for routine screening and appropriate psychosocial interventions.[9-12] Routine distress screening in larger centres in India is a challenge due to the sheer volume of patients, lack of trained workforce, financial constraints and the absence of standard distress screening guidelines.[13] However, some centres in the country are positively trying to adapt distress screening procedures where there is availability of a dedicated team to handle psychosocial distress.[14] In this context, healthcare providers also have role to play along with care administrators in the implementation of distress screening and management protocols to further improve psychosocial care.[15]
Hence, our study explored healthcare provider perspectives on routine distress screening and use of psycho-oncology services (POS) at our tertiary cancer hospital.
MATERIALS AND METHODS
Study design
We conducted a concurrent mixed methods study.[16] The quantitative phase (cross-sectional design using secondary data) was a record review of levels of distress reported by patients and referrals to POS for all new patients attending the outpatient department (OPD) of hospital. The qualitative phase (descriptive design) explored healthcare providers perspectives using in-depth one-to-one interviews on their utilisation of distress management system and POS. Consolidated Criteria for Reporting Qualitative Research was used to structure the qualitative findings.[17]
Setting and distress screening process
All new patients (irrespective of stage of cancer and treatment) attending the OPD are first assessed for their vitals by the nursing team. Subsequently, they are screened for distress by a psycho-oncology professional using the NCCN Distress Thermometer and problem checklist (henceforth called as NCCN-DT) which consists of a single-item, 11-point Likert scale that is represented in the form of a thermometer that ranges from 0 (no distress) to 10 (extreme distress) along with a 39-item problem checklist, consisting of practical, family, emotional, spiritual-religious or physical problems. Patients report level of distress based on their objective assessment of psychological distress over the past week.[18]
The NCCN-DT was translated, face validated and back-translated to Kannada, Tamil and Hindi (local languages) to ease the process of comprehension for all patients. The screening took about 3–5 min to complete. It is most often self-administered unless the patient is illiterate or finds it difficult to understand the questions. Distress scores are documented in the electronic medical record (EMR), which can be accessed by all oncologists/physicians in the hospital. After completing the distress screening, patients consult their respective oncologist/physician. Standard operating procedures (SOPs) of POS based on the NCCN guidelines state that a score of 4–10 on the NCCN-DT is classified as moderate to extreme distress and warrants individual psycho-oncology consultations post-oncologist/physician consultations.
Participants
In the quantitative phase, we included all adult patients (18–90 years) screened for distress using NCCN-DT in the OPD of the hospital between January and June 2017. In the qualitative phase, we included all oncologists and physicians working in the hospital between September 2018 and January 2019 from the departments of medical oncology, surgical oncology, radiation oncology, pain and palliative care and psycho-oncologists. We excluded those unavailable after three attempts of contact over 1 month.
Study procedure
We extracted the quantitative data (demographic details, distress scores and problems reported on the problem checklist, referrals) from the EMR.
For the qualitative phase, we prepared the interview schedule and after pilot testing, rephrased and combined few questions to obtain more meaningful narratives. Healthcare providers were asked for a feasible date and time at the hospital (approached in person) to conduct the interviews. The interview was conducted only once in English and audio recorded (after obtaining separate consent). The mean duration of the interviews was 14 min and 33 s.
Data analysis
We analysed the quantitative data using SPSS v 20.0 and summarised the distress score using median and interquartile range (IQR). We summarised the prevalence of moderate to extreme distress (distress score ≥4 on the NCCN-DT), problems reported on NCCN problem checklist, distribution of distress across age groups, gender and diagnostic groups and referrals to POS as frequencies and proportions.
The interviews were conducted by the researcher (MN) as she was trained in qualitative research methodology. The audio recorded transcripts were transcribed on the same day after the interviews were conducted. Researchers (MN and ESF) read the transcripts to become familiar with the data and conducted manual descriptive thematic analysis independently. A third reviewer (KJ) reviewed it to reduce bias and improve interpretive credibility. We used standard procedures and consensus for the decisions on coding rules and theme generation.[19] We generated codes and combined similar codes into themes.[20] We resolved any differences by discussion or resorting to the third researcher (KJ). To ensure that the results were a reflection of the data, we related the codes/themes to the original data.[21] The verbatim quotes are reported using italicised fonts within double quotation marks, researcher explanations within quotes in square brackets and details of the participants in round brackets and italicised.
RESULTS
Quantitative phase
Of the 375 patients whose records were reviewed, we included 372. We excluded three as they did not meet the inclusion criteria (two patients were aged below 18 years and one patient was 91 years). Of the included patients, 264 (71%) belonged to the age group of 41–80 years and 231 (62.1%) were female. Breast cancer (17.2%), haematological malignancies (13.2%) and a non-cancer diagnosis (33.3%) were the common diagnostic categories [Table 1].
| Patient characteristics | N | % |
|---|---|---|
| Total | 372 | 100.0 |
| Sociodemographic details | ||
| Age (in years) | ||
| 18–40 | 97 | 26.1 |
| 41–60 | 151 | 40.6 |
| 61–80 | 113 | 30.4 |
| 81–90 | 11 | 3.0 |
| Gender | ||
| Male | 141 | 37.9 |
| Female | 231 | 62.1 |
| Place of residence | ||
| Bengaluru | 283 | 76.1 |
| Within Karnataka | 37 | 9.9 |
| Other Indian state | 40 | 10.8 |
| Other country | 11 | 3.0 |
| Missing | 1 | 0.3 |
| Diagnosis | ||
| Genitourinary cancers | 10 | 2.7 |
| Other cancers† | 17 | 4.6 |
| Gynaecological Malignancies | 33 | 8.9 |
| Head-and-neck cancers | 34 | 9.1 |
| Gastrointestinal cancers | 37 | 9.9 |
| Haematological malignancies | 49 | 13.2 |
| Breast cancer | 64 | 17.2 |
| Non-cancer diagnosis‡ | 124 | 33.3 |
| Missing | 4 | 1.1 |
| Clinical characteristics | ||
| Level of distress (range) | ||
| No distress (0) | 109 | 29.3 |
| Mild distress (1–3) | 64 | 17.2 |
| Moderate distress (4–6) | 146 | 39.2 |
| Severe distress (7–9) | 43 | 11.6 |
| Extreme Distress (10) | 10 | 2.7 |
| Health system-related characteristics | ||
| Total referrals to POS | 32 | 8.6 |
| Referrals to POS based on >4 distress score | 25 | 6.66 |
NCCN: National Comprehensive Cancer Network, POS: Psycho-oncology service. Other cancers include melanoma (n=1), brain tumours (n=2), cancer of unknown origin (n=2), sarcoma (n=3) and lung cancer (n=9). ‡Non-cancer diagnosis includes benign breast conditions (fibroadenoma), benign ovarian cyst, general medical conditions, fibromyalgia, chronic pain, supportive care and gastrointestinal conditions
The overall median distress score was 4 (IQR: 0–6) and 199 (53.5%) had moderate to extreme distress. The distribution of moderate to extreme distress was not significantly different across age, sex and diagnostic categories [Table 2]. Referrals to POS were 32 (8.6%) and this was irrespective of the level of distress (mild, moderate or extreme distress), although 189 (91%) who reported moderate to severe distress were not referred [Table 3]. Pain (n = 204, 54.8%), worry (n = 181, 48.7%), sleep (n = 158, 42.5%) and fatigue (n = 141, 37.9%) were key domains reported on the problem checklist [Figure 1].
| Patient characteristics | Total | <4 Distress score | >4 Distress score | ||
|---|---|---|---|---|---|
| N | n | % | n | % | |
| Total | 372 | ||||
| Age (in years) | |||||
| 18–40 | 97 | 38 | 10.2 | 59 | 15.9 |
| 41–60 | 151 | 68 | 18.3 | 83 | 22.3 |
| 61–80 | 113 | 59 | 15.9 | 54 | 14.5 |
| 81–90 | 11 | 8 | 2.2 | 3 | 0.8 |
| Gender | |||||
| Male | 141 | 69 | 39.8 | 72 | 36.2 |
| Female | 231 | 104 | 60.1 | 127 | 63.8 |
| Diagnosis | |||||
| Genitourinary cancers | 10 | 4 | 2.3 | 5 | 2.5 |
| Other cancers† | 17 | 5 | 2.9 | 12 | 6.0 |
| Gynaecological malignancies | 33 | 14 | 8.1 | 19 | 9.5 |
| Head-and-neck cancers | 34 | 16 | 9.3 | 18 | 9.0 |
| Gastrointestinal cancers | 37 | 14 | 8.1 | 23 | 11.6 |
| Haematological malignancies | 49 | 22 | 12.8 | 27 | 13.6 |
| Breast cancer | 64 | 36 | 20.9 | 28 | 14.1 |
| Non-cancer diagnosis‡ | 124 | 58 | 33.7 | 66 | 33.2 |
| Missing | 4 | 3 | 1.7 | 1 | 0.5 |
NCCN: National Comprehensive Cancer Network. †Other cancers include melanoma (n=1), brain tumours (n=2), cancer of unknown origin (n=2), sarcoma (n=3) and lung cancer (n=9). ‡Non-cancer diagnosis includes benign breast conditions (fibroadenoma), benign ovarian cyst, general medical conditions, fibromyalgia, chronic pain, supportive care and gastrointestinal conditions
| Patient characteristics | Total | Patient’s referred | Patient’s not referred | Not recorded | |||
|---|---|---|---|---|---|---|---|
| N | n | % | n | % | n | % | |
| Total | 372 | 32 | 8.6 | 339 | 91.1 | 1 | 0.3 |
| Age in (years) | |||||||
| 18–40 | 97 | 8 | 8.2 | 89 | 91.8 | 0 | 0 |
| 41–60 | 151 | 14 | 9.3 | 136 | 90.1 | 1 | 0.7 |
| 61–80 | 113 | 9 | 8.0 | 104 | 92.0 | 0 | 0 |
| 81–90 | 11 | 1 | 9.1 | 10 | 90.9 | 0 | 0 |
| Gender | |||||||
| Male | 141 | 14 | 9.9 | 127 | 90.1 | 0 | 0 |
| Female | 231 | 18 | 7.8 | 212 | 91.8 | 1 | 0.4 |
| Levels of distress | |||||||
| <4 Distress score | 173 | 14 | 8.1 | 158 | 91.33 | 1 | 0.6 |
| >4 Distress score | 199 | 18 | 9.00 | 181 | 91.0 | 00 | 0 |
POS: Psycho-oncology service
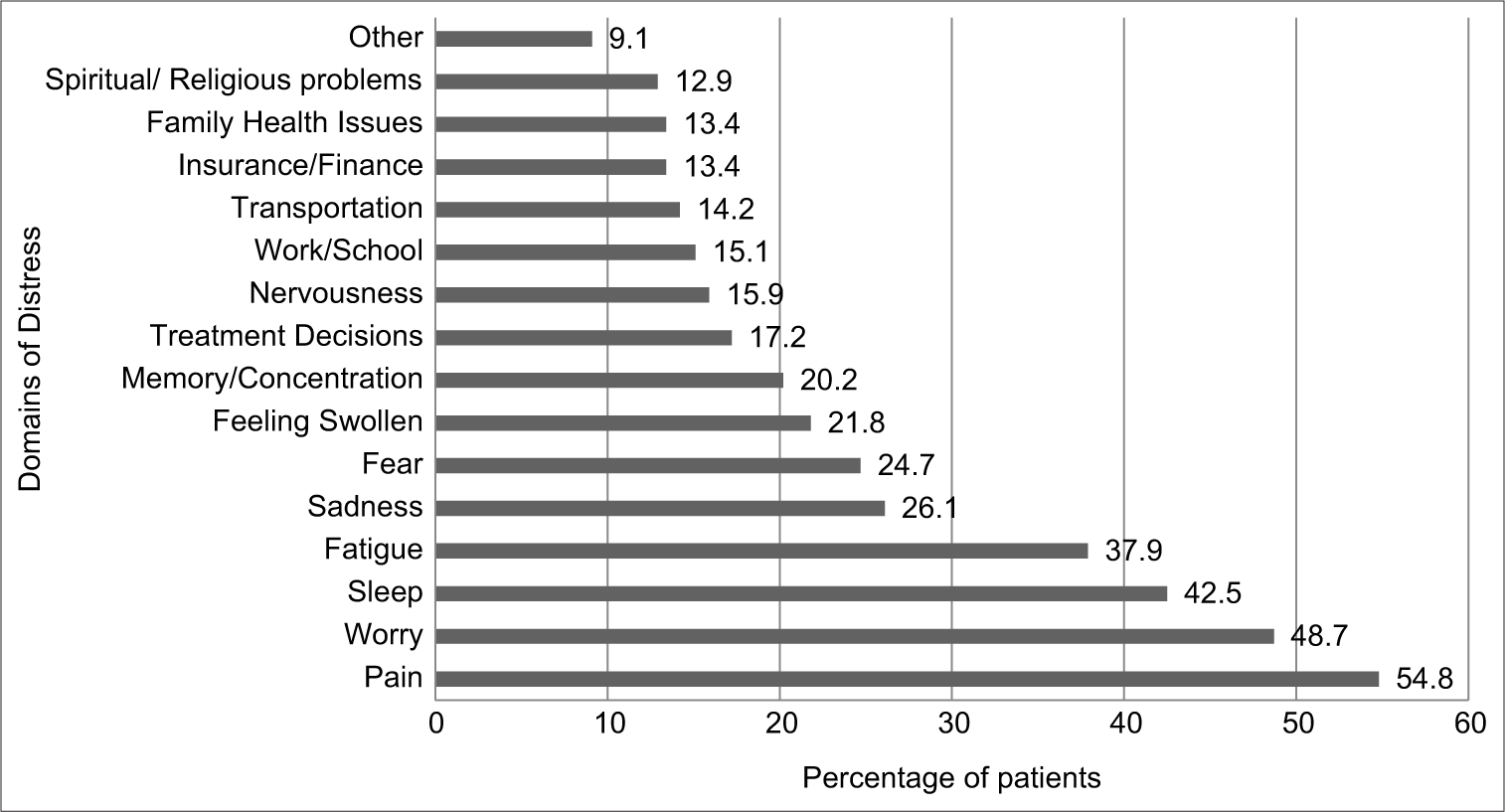
- Key problems reported on the Problem Checklist of the NCCN Distress Thermometer by patients in the Out-Patient Department of a private tertiary cancer hospital in Bengaluru, India (January- June, 2017).
Qualitative phase
We approached 15 healthcare providers for the study of which one oncologist was excluded due to non-availability. The average years of experience in oncology were 9.8 (range: 2–25 years), majority of the healthcare providers were male (71%) and were oncologists/physicians (86%) [Table 4].
| Participant characteristics | n | % |
|---|---|---|
| Total | 14 | 100 |
| Gender | ||
| Male | 10 | 71 |
| Female | 4 | 29 |
| Healthcare providers | ||
| Oncologist/physician | 12 | 86 |
| Psycho-oncologist | 2 | 14 |
| Number of years of experience in oncology | ||
| ≤5 | 5 | 36 |
| 6–15 | 5 | 36 |
| >15 | 4 | 28 |
Three major themes emerged from the semi-structured interviews – Enablers, barriers and solutions for utilisation of distress management system and POS based on factors related to healthcare providers, the system and patient-related factors [Table 5].
| Themes | Enablers | Barriers |
|---|---|---|
| Healthcare provider-related factors |
|
|
| System-related factors |
|
|
| Patient-related factors |
|
|
OPD: Outpatient department, POS: Psycho-oncology service, SOP: Standard operating procedure, INR: Indian rupees, IPD: Inpatient department, HIS: Hospital information system, NCCN: National Comprehensive Cancer Network
Enablers for utilisation of distress management system and POS
Healthcare provider-related factors
Healthcare providers reported that patients and families usually experience very high levels of distress when dealing with a diagnosis of cancer and the reasons for distress can be diverse.
‘It’s 100% but there are different forms of distress’ (HP 8).
‘See the hard data are missing but I would put it at a very high level because you know cancer diagnosis is never going to be pleasant, the level of distress may vary. I think everybody is distressed’ (HP 3).
‘So, I would say in my oncology practice I think everybody would be distressed. I mean even I would be distressed if I am diagnosed with a cancer but the word cancer itself sometimes is perceived a death sentence and so nobody wants to undergo the ill effects which is perceived by the patient so they always have some amount of distress’ (HP 1).
‘Distress, I think all the patients will have to a certain extent and most of the relatives will also have it’s not just the patient. But as far as I have seen I think from the time of diagnosis the shorter that period is the more stressful they are’ (HP 2).
They also acknowledged that patients experienced distress irrespective of demographics, time and diagnosis.
‘I think if you’re well-off socially, there is something…same as low socioeconomically… So, there’s always a flip side of whatever the advantage may be of the socioeconomic status or the financial. So, I feel there is some distress or the other because the need in a person who is actually suffering with cancer is very high’ (HP 7).
‘I really don’t think so. I think it’s distressing at any age to have this thing [cancer]’ (HP 9).
Healthcare providers were found to be sensitive to emotional distress but managed to handle distress only to a certain extent.
‘Every cancer patient is distressed. So, we obviously do a lot of counselling at diagnosis and then there are accessory services like what you’ll [POS]provide’ (HP 9).
‘In the initial phase when they consult us. So, we also make an effort to find their emotional needs and about what they think about cancer but beyond certain things we would actually fail in doing it because we will not understand quite well the social, the spiritual and also the family issues’ (HP 1).
‘I don’t have any experience in treating distress in cancer patients. There is definitely distress but I’m not equipped to handle it. If I feel it particularly that any patient is in distress, I refer them to POS . If I feel that patients are taking it well then, I don’t do it’ (HP 5).
Healthcare providers also described the negative impact of untreated distress on compliance to treatment, outcomes and quality of life.
‘At times due to distress there would be hesitancy and delay in starting treatment sometimes it matters regarding outcomes. And it also makes them vulnerable to go for some other alternative treatments which have not been found to be useful in any scientific studies’ (HP 5).
‘The most important thing is the patient can be non-compliant to treatment. And that will affect directly the outcome of the cancer treatment. This is primarily our concern because without treatment there is no outcome’ (HP 4).
‘Definitely health-related quality of life is a very important aspect, because it’s not only one domain we are looking at. its physical it’s emotional and social, spiritual. It is all areas of their life can get affected due to distress. So, it’s definitely important to understand and look at it as a whole’ (HP 13).
System-related factors
Healthcare providers also conveyed being aware of distress screening for patients in the hospital and were pleased with the availability of dedicated psycho-oncological support.
‘In our hospital, we screen all the patients and we have a distress scoring. This is on par with the international guidelines…’ (HP 1).
‘We actually have an independent assessment of distress itself through the distress thermometer. Each and every patient goes through that. at least we get a full feedback saying that this patient is in distress or the family is in distress’ (HP 12).
‘We have a dedicated team who will look into this [distress management]. There are professionals who come with experience in oncology so they know as to what is expected of them’ (HP 6).
Patient-related factors
Healthcare providers strongly felt that majority patients who availed psycho-oncological services were compliant and benefiting from the services.
‘I think they are very well compliant [patients]. There is a thought that many patients will not comply but the majority. I have not seen a single patient, may be a few patients have refused to speak to psycho oncology team but majority of the patients are or want to speak to somebody’ (HP 4).
‘The stigma like I said it’s sort of coming down…’ (HP 14).
‘So initially when we started out, we got only doctor referrals mainly. Again, now approximately 50% of them [patients]would come by themselves and feel the need to, you know… address their concerns because they know that they have issues and they need help’ (HP 13).
‘It’s 100%. I think it comes out from the person who is recommending and especially when we are saying that this is something that is needed. Compliance is not an issue at all I feel that it is a myth that patients are not complying to POS at all’ (HP 12).
Barriers for utilisation of distress management system and POS
Healthcare provider-related factors
Healthcare providers discussed that often when a patient is diagnosed with cancer the primary focus becomes, cure or control of the disease from a treatment standpoint, and not immediately focussing on the distress.
‘Distress is a big problem. But it is always underestimated only because the focus always remains on the cancer care and cure’ (HP 3).
‘We take care of the distress of cancer patients by different ways. Our main contribution will be by treating the cancer itself because the most important way to treat the distress is to treat the cancer. And if the cancer is cured, most of the time the distress is over’ (HP 4).
Time constraints due to increased volumes of patients were also considered as a challenge for healthcare providers to view the scores on the EMR.
‘Doctors can actually view their [patients]distress scores… sometimes again, lack of time because there’s so many patients who come in… it becomes little tough on the consultant to actually open [EMR]and understand the patient has an issue’ (HP 13).
‘See most of the time I don’t see the distress score. So, unless a psycho-oncology person has intimated me then I refer them back or I call them during consultation’ (HP 2).
System-related factors
Healthcare providers made referrals to POS based on their individual clinical discretion and did not follow a particular system.
‘I think it still remains a vague issue where there are a lot of individual discretions both in part of patients and physicians. I think the patient discretion should always be respected we may not be able to change much on that but I think certain guidelines of physician’s referrals would certainly help’ (HP 3).
‘We do it in a different way. Our referral, we have a very high threshold for referrals. Only when there is probably severe one which is leading to non-compliance then only, we would refer’ (HP 10).
Healthcare providers mentioned the timing of screening and the tool was generic in nature and may not capture distress levels accurately or may underestimate it.
‘But for a patient who does not know he has a cancer but comes for the 1sttime for an investigation it really doesn’t make sense, because screening itself will have a distress factor on him because he may say why am I being screened for distress?’ (HP 8).
‘Also, the current screen is very superficial and it’s quite preliminary. So, it may not reflect the true distress. So, I think we need to start working towards more… a more meaningful screening. Each specialty here would be on a different requirement so I think that should be the code to develop specialty specific screenings’ (HP 3).
Patient-related factors
Healthcare providers reported that distress screening and a referral for psychological support are often viewed negatively due to lack of awareness.
‘I think the most important thing is the basic social factors which come whenever you say the word psychiatry, psychology it’s a lack of understanding in the patients’ (HP 3).
‘I think some people somehow don’t like the idea of being told to go meet the psychology team because they feel like you know they’ve been told that they cannot handle the stress’ (HP 9).
‘I don’t know. sometimes I think it’s an attitude, that some people feel that they are fine and don’t need support they are the people who need maximum support actually’ (HP 4).
‘There were some people [patients]where they were not willing to go in because you had to make a payment for it [POS], But again, that’s a professional advice that you are giving’ (HP 8).
Solutions for better utilisation of distress management system and POS
Suggestions on ways to increase awareness about distress management and improve utilisation of POS are described in [Table 6].
| Themes | Solutions |
|---|---|
| Healthcare provider-related factors |
|
| System-related factors |
|
| Patient-related factors |
|
POS: Psycho-oncology service, NCCN: National Comprehensive Cancer Network: SOP: Standard operating procedure, CME: Continuous medical education
DISCUSSION
Our study found patients reporting moderate to extreme levels of distress on the NCCN-DT in the OPD. Despite the elevated levels of distress and the availability of the distress scores on the EMR, referrals to psycho-oncology support services were very poor. Healthcare providers agreed that patients experienced distress with a diagnosis of cancer and the impact of this distress could affect treatment outcomes and quality of life. They also reported being aware of the distress management system and POS in the hospital, however relied on their individual discernment for managing distress and making referrals to POS.
There were three key findings in our study. First was the underutilisation of POS despite healthcare providers being cognizant about distress, its implications and the management system. The level of distress reported in our study is consistent with other studies which predominantly found moderate to extreme levels of distress being reported by patients.[22-27] The major concerns reported on the problem checklist such as pain, worry, sleep and fatigue were also similar to other studies.[28] Although patients reported distress in the OPD, the rates of referrals to POS were found to be low which questioned the purpose of implementing routine screening for distress. An Indian study which was consistent with our findings described that even though healthcare providers were effective in identifying distress among patients, there were substantial hits and misses.[29] Thus, we understand from literature that the success of any distress screening system is measured only when distress scores are reviewed and acknowledged by oncologists so as to appropriately provide psychological support to patients in a timely manner.[13,30] Healthcare providers in our study relied on their clinical judgement about distress which resulted in lesser utilisation of the POS services. However, we understand that patients are often more receptive to talk about their emotional concerns with their healthcare providers and their recommendation/referral was one of the strongest predictors for patients to avail POS.[31,32] In our study, there was also a felt need for specific physician referral guidelines as the existing SOP was vague, screening tool, generic in nature and screening intervals being unsuitable even though this was based on the distress management guidelines provided by NCCN. Multiple studies recommend the need for training and support for cancer care clinicians to develop and implement an appropriate psychosocial screening programme so as to overcome institutional and patient-related barriers.[33-35] Another study suggested that to increase utilisation of POS services, clinicians can provide a triage to make appropriate referrals to the POS based on the distress scores.[36] Healthcare providers who are more aware of their roles and responsibilities in distress screening and referrals take a more active role in paying attention to distress and psychological concerns of the patients.[37-39]
Second, challenges faced by healthcare providers in utilisation of POS. Healthcare providers had independent views on distress management and POS. The first barrier reported was the focus on cancer treatment and cure where the physical aspect took priority over psychological distress. Research evidence more recently points to incorporating a multidimensional approach to cancer care that focuses on the whole person and that it is as much emotional as it is physical.[40-42] Healthcare providers also discussed about negative attitudes and reactions of patients/families which accompanied a referral to POS. Multiple studies indicate that patients who report moderate to severe distress and are referred for psychosocial support often refrain from taking up services.[39,43-45] Some of the reasons were due to attitudinal issues, feeling that professional help would be futile, perceived to having adequate support from family and friends, etc. Sometimes poor knowledge about availability of psychological support services and its benefits in itself could be a hindrance in uptake of services.[46]
Third, way forward to integrate POS into routine cancer care. Healthcare providers in our study stressed on the need to have capacity building initiatives, design educational pamphlets and patient advocacy groups, engage in evidence-based research to improve awareness about POS. An Indian study reported similar findings that described the benefits of having professional and trained psycho-oncology professionals to implement strategies to improve visibility of services.[13] From a research standpoint, a systematic review conducted in India suggested the need for concentrated efforts from interested clinicians and psycho-oncology professionals to bring to the forefront the relevance of psychosocial research in a clinical setting.[47]
We believe to the best of our knowledge that this was the first study in India which explored healthcare providers perspectives about distress screening system and POS in a cancer setting. Our study findings have implications on the current practices which are being followed by POS in the OPD of the hospital. (i) The existing SOP on distress screening and management will have to be revised in terms of intervals of screening, physician referral guidelines and devising site-specific screening tools. (ii) Increase visibility and improve awareness about POS to reduce overall negative outlook toward availing psycho-oncological support.
CONCLUSION
It is evident that effective distress screening, implementation and management are a real concern in cancer which is consistent with the narratives of healthcare providers. The reasons for underutilisation of existing psycho-oncological services were time constraints, patient’s negative attitudes toward mental health referrals, generic screening tools and use of own clinical judgement to make referrals. The enablers and solutions provided focused on implementing strategies to integrate POS into routine cancer care by focusing on improving visibility of services.
ACKNOWLEDGEMENT
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Program for Research and Training in Tropical Diseases at the World Health Organisation (WHO/TDR). The training model is based on a course developed jointly by the International Union against Tuberculosis and Lung Disease (The Union) and Medécins sans Frontières (MSF/Doctors Without Borders). The specific SORT IT program which resulted in this publication was jointly developed and implemented by: Fenivi Research Solutions Private Limited, Chennai, India; The Union South-East Asia Office, New Delhi, India; and the Centre for Operational Research, The Union, Paris, France. Mentorship and the coordination/facilitation of this particular SORT IT program were provided through Fenivi Research Solutions Private Limited, Chennai, India; The Union South-East Asia Office, New Delhi, India; the Centre for Operational Research, The Union, Paris, France; Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India; All India Institute of Medical Sciences (AIIMS), Nagpur, India, and Velammal Medical College Hospital and Research Institute, Madurai, India. The author would also like to thank all the oncologists/physicians and psycho-oncology professionals who consented to be interviewed for the study. A special mention to my colleague in the department of psycho-oncology services for her support and timely help. My gratitude to all members at Fenivi Research Solutions for their encouragement and guidance.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Screening for distress, the 6th vital sign: Where are we, and where are we going? Psychooncology. 2011;20:569-71.
- [CrossRef] [PubMed] [Google Scholar]
- A practice-based evaluation of distress screening protocol adherence and medical service utilization. J Natl Compr Canc Netw. 2017;15:903-12.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494-502.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological intervention and health outcomes among women treated for breast cancer: A review of stress pathways and biological mediators. Brain Behav Immun. 2009;23:159-66.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for distress and unmet needs in patients with cancer: Review and recommendations. J Clin Oncol. 2012;30:1160-77.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for emotional distress in cancer patients: A systematic review of assessment instruments. J Natl Cancer Inst. 2009;101:1464-88.
- [CrossRef] [PubMed] [Google Scholar]
- Distress screening using distress thermometer in head and neck cancer patients undergoing radiotherapy and evaluation of causal factors predicting occurrence of distress. Indian J Palliat Care. 2013;19:88-92.
- [CrossRef] [PubMed] [Google Scholar]
- Distress management in patients with head and neck cancer before start of palliative chemotherapy: A practical approach. J Glob Oncol. 2018;4:1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of distress among patients and primary caregivers: Findings from a chemotherapy outpatient unit. Indian J Palliat Care. 2020;26:42-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pilot study of single-day distress screening with the NCCN distress thermometer to evaluate the feasibility of routine distress screening in tertiary cancer center in rural India. Psychooncology. 2015;24:832-4.
- [CrossRef] [PubMed] [Google Scholar]
- Integrating psycho-oncology services in cancer care in India. Indian J Cancer. 2021;58:290-3.
- [Google Scholar]
- Progress toward integrating distress as the sixth vital sign: A global snapshot of triumphs and tribulations in precision supportive care. J Psychosoc Oncol Res Pract. 2019;1:e2.
- [CrossRef] [Google Scholar]
- Feasibility of implementing the 'screening for distress and referral need' process in 23 dutch hospitals. Support Care Cancer. 2017;25:103-10.
- [CrossRef] [PubMed] [Google Scholar]
- A methodology for conducting integrative mixed methods research and data analyses. J Mix Methods Res. 2010;4:342-60.
- [CrossRef] [PubMed] [Google Scholar]
- Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349-57.
- [CrossRef] [PubMed] [Google Scholar]
- The distress thermometer: Cutoff points and clinical use. Oncol Nurs Forum. 2017;44:329-36.
- [CrossRef] [PubMed] [Google Scholar]
- The coding manual for qualitative research Los Angeles, CA, United States: SAGE Publications; 2010.
- [Google Scholar]
- Designing and Conducting Mixed Methods Research London, United Kingdom: SAGE Publications Ltd.; 2007.
- [Google Scholar]
- Psychological problems of cancer patients: A cancer distress screening with a cancer-specific questionnaire. Br J Cancer. 2004;91:504-11.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic screening for distress in oncology practice using the distress barometer: The impact on referrals to psychosocial care. Psychooncology. 2014;23:804-11.
- [CrossRef] [PubMed] [Google Scholar]
- The distress thermometer: A rapid and effective tool for the oncology social worker. Int J Health Care Qual Assur. 2013;26:353-9.
- [CrossRef] [PubMed] [Google Scholar]
- Integration of the national comprehensive cancer network (NCCN) distress screening tool as a guidepost for telephonic oncology case management. Prof Case Manag. 2019;24:148-54.
- [CrossRef] [PubMed] [Google Scholar]
- Implementing screening for distress, the 6th vital sign: A canadian strategy for changing practice. Psychooncology. 2011;20:463-9.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of psychological distress and its effect on quality of life and social functioning in cancer patients. Indian J Palliat Care. 2018;24:72-7.
- [Google Scholar]
- An analysis of the distress thermometer problem list and distress in patients with cancer. Support Care Cancer. 2015;23:1225-32.
- [CrossRef] [PubMed] [Google Scholar]
- Oncologists' proficiency in identifying psychological distress in cancer patients: Hits and misses. J Clin Oncol. 2014;32:e20572.
- [CrossRef] [Google Scholar]
- Best practices in oncology distress management: Beyond the screen. Am Soc Clin Oncol Educ Book. 2018;38:813-21.
- [CrossRef] [PubMed] [Google Scholar]
- Oncologist recommendation matters!-Predictors of psycho-oncological service uptake in oncology outpatients. Psychooncology. 2019;28:351-7.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to mental health service use and preferences for addressing emotional concerns among lung cancer patients. Psychooncology. 2014;23:812-9.
- [CrossRef] [PubMed] [Google Scholar]
- Interventions to improve screening and appropriate referral of patients with cancer for psychosocial distress: Systematic review. BMJ Open. 2018;8:e017959.
- [CrossRef] [PubMed] [Google Scholar]
- Managing psychosocial distress: Lessons learned in optimizing screening program implementation. Oncology (Williston Park). 2018;32:488-90, 492-3
- [Google Scholar]
- Advancing the science of distress screening and management in cancer care. Epidemiol Psychiatr Sci. 2020;29:e85.
- [CrossRef] [PubMed] [Google Scholar]
- Nursing expertise and the evaluation of psychosocial distress in patients with cancer and survivors. Clin J Oncol Nurs. 2014;18:598-600.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of pharmacist-assisted screening and psychiatric referral program for outpatients with cancer undergoing chemotherapy. Psychooncology. 2011;20:647-54.
- [CrossRef] [PubMed] [Google Scholar]
- Does routine psychosocial screening improve referral to psychosocial care providers and patient-radiotherapist communication? A cluster randomized controlled trial. Patient Educ Couns. 2013;93:289-97.
- [CrossRef] [PubMed] [Google Scholar]
- Physicians' attitudes towards psycho-oncology, perceived barriers, and psychosocial competencies: Indicators of successful implementation of adjunctive psycho-oncological care? Psychooncology. 2019;28:415-22.
- [CrossRef] [PubMed] [Google Scholar]
- Integrative oncology for the whole person: A multidimensional approach to cancer care. Integr Cancer Ther. 2010;9:105-21.
- [CrossRef] [PubMed] [Google Scholar]
- Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American society of clinical oncology guideline adaptation. J Clin Oncol. 2014;32:1605-19.
- [CrossRef] [PubMed] [Google Scholar]
- Management of distress in patients with cancer-are we doing the right thing? Ann Behav Med. 2020;54:978-84.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding why cancer patients accept or turn down psycho-oncological support: A prospective observational study including patients' and clinicians' perspectives on communication about distress. BMC Cancer. 2017;17:385.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer patient utilisation of psychological care in Germany: The role of attitudes towards seeking help. Eur J Cancer Care (Engl). 2019;28:e13165.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to psychosocial oncology service utilization in patients newly diagnosed with head and neck cancer. Psychooncology. 2018;27:2786-93.
- [CrossRef] [PubMed] [Google Scholar]
- Patient and health professional's perceived barriers to the delivery of psychosocial care to adults with cancer: A systematic review. Psychooncology. 2014;23:601-12.
- [CrossRef] [PubMed] [Google Scholar]
- Psycho-oncology research in India: Current status and future directions. J Indian Acad Appl Psychol. 2008;34:7-18.
- [Google Scholar]







