Translate this page into:
“Post-COVID-19 syndrome:” The New Pandemic Affecting Healthcare Workers and How the Frontline Warriors Are Battling it

*Corresponding author: Souvik Chaudhuri, Department of Critical Care, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India. souvikchaudhuri1207@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rao S, Amara V, Chaudhuri S, Rao BK, Todur P. “Post-COVID-19 syndrome:” The new pandemic affecting healthcare workers and how the frontline warriors are battling it. Indian J Palliat Care 2021;27(2):313-8.
Abstract
Objectives:
“Post-COVID-19 syndrome,” which may be the new pandemic, has affected various domains of quality of life; even among those who have recovered from mild COVID-19 disease. The aim of our study was to explore the health, social and psychological impact on healthcare workers (HCWs) who have recovered from active COVID-19 illness and highlight their needs post-recovery.
Materials and Methods:
It was a web-based survey study. A total of 163 eligible consenting HCWs participated in this survey. The Institutional Ethical Committee approval was obtained before study recruitment and the study was registered with the Clinical Trial Registry of India. Each participant responded to 25 questions.
Results:
Among those participated, 51% were doctors, 32% were nurses and others were allied health professionals and students. About 82% had mild COVID-19 illness and 40% required hospitalisation for COVID-19 treatment. In the post-recovery period, 66% experienced health issues and fatigue on mild exertion was the most common symptom (42.94%). It was followed by anosmia and ageusia (21.47%), headache and myalgia (15.34%) and breathlessness (8.59%). About 82% HCW felt the need for a post-COVID-19 recovery health care unit. Potential risk of infecting family members was the most common concern (53.46%) followed by the fear of contracting the virus again (46.54%). About 35% of HCW experienced the fear of developing post-COVID-19 complications. About 78% of HCW did not report any psychological concerns, but one-third were stressed due to the financial impact.
Conclusion:
Post-COVID-19 syndrome impacts all domains of quality of life. Fatigue, loss of taste and smell, headache, myalgia and breathlessness continue to persist beyond recovery of active illness. Most of the HCWs emphasised the need to set up post-COVID-19 care units. The fear of contracting the virus again and financial drain due to hospital expenses continued to distress HCWs.
Keywords
Healthcare workers
Heath issues
Post-COVID-19 syndrome
INTRODUCTION
“Post-COVID-19 syndrome” has affected millions of COVID-19-recovered patients, with about 87% of hospitalised patients suffering from it.[1] Even those with mild COVID-19 are suffering from persistent health issues after initial recovery.[1] Healthcare workers (HCWs) are always at a high risk of infection due to the nature of their work and pose the risk of disease transmission to their family members.[2] With the ever-increasing number of post-COVID-19 patients, the new pandemic is the “post-COVID-19 syndrome.” Studies in COVID-19-recovered patients are recognised as an important need of the hour.[3] Even with the initial recovery, it is a battle half won, and often, the post-COVID-19 issues continue to linger. We wanted to assess and highlight the various health, social and psychological issues faced by HCW themselves after recovery from COVID-19 infection and need for setting-up of post-COVID-19 clinics at health care establishments. The aim of our study was to assess the health, social and psychological impact on HCWs who had recovered from COVID-19 and highlight their specific needs post-recovery.
MATERIALS AND METHODS
The study was a web-based single-centre survey study. It was conducted over 8 weeks during January–March 2021. The Institutional Ethics Committee permission was obtained (KH/KMC IEC 714/2020) and Clinical Trial Registry of India (CTRI) registration was done CTRI/2021/01/030430 before recruitment for the study.
Study design
The questions of the survey study were validated by six experts from various fields of health care who had themselves recovered from COVID-19. The questionnaire was then sent as a weblink to the institutional authorities, which was then sent by the institutional authorities to the respective HCW who had recovered from COVID-19. The questionnaire had a total of 25 questions, with 5 about demographics, 3 about their COVID-19 experience and remaining 17 about the post-COVID period, incorporating health, social, psychological issues and their change in behaviour and practices in the post-COVID recovery period. The questions were closed ended with more than 1 options in some, where it was deemed necessary. Each HCW was allowed to participate only once in the study.
Statistical analysis
The answers of the survey were analysed using the web-based platform analysis tool and were expressed as percentage, with depiction as bar graphs or pie charts.
RESULTS
Out of 163 participants, 51% were doctors, 32% were nurses, 9% were allied health professionals and 9% were students. The demographics of the HCS are depicted in Table 1.
| Category of HCW | Doctors (51%) | Nurses (31%) | Allied health professional (9%) | Students (9%) | |
|---|---|---|---|---|---|
| Age group of HCW | <30 years (52%) | 30–40 years (32%) | 40–50 years (11%) | 50–60 years (3%) | >60 years 1% |
| Gender | Male (41%) | Female (59%) | |||
| Pre-existing comorbidities | Nil (80%) | Hypertension (8%) | Diabetes mellitus (4%) | Bronchial asthma (6%) | Other (6%) |
| Category of COVID-19 | Mild (82%) | Moderate (7%) | Severe (1%) | Unsure about category (10%) |
The majority of the participants did not require hospitalisation during the COVID-19 disease period (60%). Fever and myalgia (64%), headache (35%), cough (32%) and sore throat (30%) were the predominant symptoms during active illness [Figure 1].

- Chief complaints of the healthcare workers during the period of COVID-19 illness.
Post-COVID-19 recovery, the most common health issue was fatigue with mild exertion (43%), followed by loss of taste and smell (21%), headache and myalgia (15%) and breathlessness 9% [Figure 2].

- Health issues affecting the healthcare workers in the post COVID-19 period.
Up to 28% of HCWs faced daily health issues post-recovery, 19% had health issues about 3–4 times per week and 44% experienced them once in 2 weeks [Figure 3].

- Frequency of the health issues faced by healthcare workers in the post COVID-19 period.
Majority of our HCW (85%) did not have any pre-existing illnesses. A formidable majority (82%) of the HCW recovered from COVID-19 expressed the need to have post-COVID-19 dedicated health care set ups in all hospitals [Figure 4].
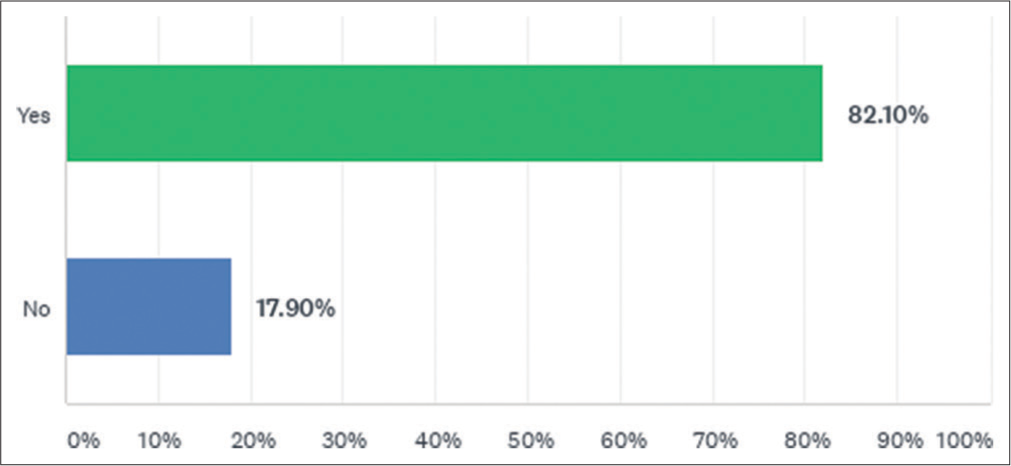
- Majority of healthcare workers who have recovered from COVID-19 expressing the need to make “post COVID-19 recovery clinics” mandatory in healthcare set-ups.
Post-recovery, 71% were leading a healthier lifestyle, with 65% practising some form of physical exercise or yoga, and 47% taking health supplements, mostly multivitamins and Vitamin C [Figure 5].

- Various supplements used by healthcare workers in the post COVID-19 recovery period.
About 79% of HCWs never got their antibody levels checked post-recovery, and 69% continued to be cautious about infection control practices. The three major concerns among HCW post-recovery were fear of contracting the virus again in a more severe form (47%), risk of infecting family members (53%) and developing post COVID-19 complications (35%) [Figure 6].
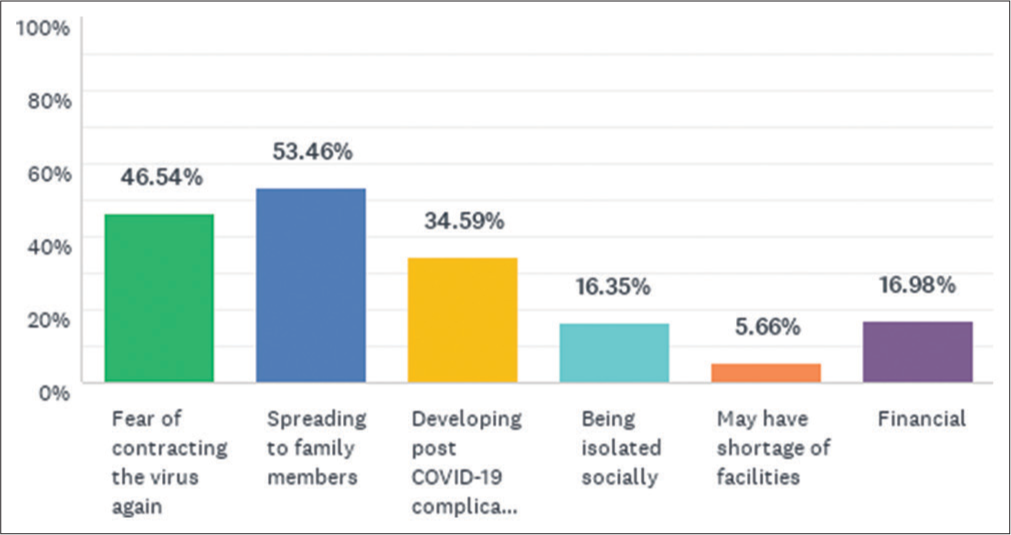
- Major concerns of the healthcare workers in the post COVID-19 recovery period.
About 51% of HCWs were anxious about getting reinfected, and about half of those seek help of friends and do meditation/yoga to relieve anxiety. About 78% of the participants did not report any psychological issues but 32% were stressed due to financial toxicity, which might arise out of hospitalisation. Majority of the HCWs (84%) did not face any sort of social stigma post-recovery.
DISCUSSION
“Post-COVID-19 syndrome” refers to various physical and psychological symptoms experienced by patients for 3 months after recovery from active COVID-19 illness, despite receiving adequate medical care during active COVID-19 illness.[1] The syndrome is reported in 95% of the COVID-19-recovered patients, irrespective of nature of COVID-19 illness or need for hospitalisation.[1] Another report corroborated the above study and found that these symptoms may be present in 35% outpatients and 87% inpatients recovering from COVID-19 illness.[4] There may be a myriad of symptoms that the patient might continue to experience in the post-COVID-19 period.[5] Severe fatigue, breathlessness, neuropsychological disorders, memory impairment, anxiety, depression, pain, persistent cough, difficulty in swallowing, voice change, incontinence, diarrhoea and dysphagia can be present post-recovery.[5] This wide spectrum of symptoms encompassing the post-COVID-19 recovery period is due to the fact that COVID-19 is not just a respiratory disorder, but a multisystem disease and so is “post-COVID-19 syndrome.”[3] The presence of fatigue with the mild exertion was the major component of “post-COVID-19 syndrome” as identified by our study participants; even though they had mild COVID-19. This feature was similar to the findings of the previous studies on post-COVID-19-recovered patients.[5,6] Fatigue incorporates multiple health issues such as breathlessness, cognitive dysfunction and psychological distress.[5] The cause of fatigue has been correlated to anaemia, Vitamin D deficiency and hypothyroidism.[5,7] However, breathlessness, which is a common symptom in post-COVID period, was found in only 9% of our HCW, probably because the majority had mild disease and breathlessness is usually a sequela of acute respiratory distress syndrome.[5] The second most common symptom in the post-COVID-recovered HCW in our study was loss of taste and smell which is likely due to damage to olfactory bulb by the virus.[3] Persistence of headache and myalgia, similar to that of our study even in non-hospitalised patients, was also found in the study by Goërtz et al.[1] The establishment of a multidisciplinary team to address these lingering health issues among all COVID-19-recovered patients, more so for our own HCWs require utmost priority.[8] Such patients may require both pharmacological and non-pharmacological treatments for the resolution of above-mentioned issues.[8] It is precisely for the evaluation and assessment of these issues in the post-COVID-19-recovered patient that mandatory follow-up clinics have been advised.[3] The disturbing fact is that up to 50% of the HCWs in our survey continue to face these health issues more than 3–4 times per week or even daily. For the assessment of the health issues post-COVID-19, a functional status scale also has been proposed.[9] The scale has a Grade 0 for no limitation in everyday life along with no symptoms, pain, depression or anxiety and Grade 4 indicating severe limitations wherein the COVID-19-recovered patient is dependent on nursing care for dealing with the symptoms.[9] Such objective ordinal scales used to monitor post-COVID-19 functional status will be extremely useful to monitor prognosis and improvement of a COVID-19-recovered patient.[9] Previous epidemic of coronaviruses has also led to post-recovery pulmonary dysfunction, fatigue, myalgia, depression, anxiety and reduction in the quality of life.[9-12] Thus, these post-coronavirus health implications have been observed in the past too, only need a greater emphasis and astute action in the present pandemic scenario because of the massive scale involved. Our survey shows that significant majority of the HCWs who have recovered from COVID-19 have echoed the need of post-COVID care clinics as a mandatory requirement. Similar recommendations were voiced in previous literature as well, where it has been stressed to follow-up the signs and symptoms of post-COVID-19-recovered patients regularly.[3] Comprehensive post-COVID centre at Yale (RECOVERY) programme is a model clinic for post-COVID-19 patients, which should be implemented in India as well.[13] The aim of RECOVERY programme is to provide a holistic evaluation of post-COVID-19 complications and issues, reduce the pulmonary complications and resolve symptoms of post-COVID-19 patients, including rehabilitation and cognitive dysfunction.[13] The post-COVID centre consists of four aspects – referral pathway, initial assessment, subsequent care and disposition.[13] The referral pathway includes a pre-discharge respiratory and physical evaluation, and the initial assessment consists of pulmonary consultation, pulmonary imaging like computerised tomography, pulmonary function tests along with mental health screening.[13] These steps were followed up by subsequent care stage, which include pulmonary rehabilitation and extrapulmonary diagnostics as well.[13] Similar clinics may be set up at hospitals in India to cater to the ever-increasing needs of post-COVID-19-recovered patients as well as the HCW on a priority basis, as it will serve a long way to ameliorate the health issues faced post-recovery. Just like the RECOVERY program design, the clinics should cater to all the categories of COVID-recovered patients, mild, moderate or severe, and will be key components of hospitals in the coming years of post-pandemic era.[13,14]
It has also been recommended that post-COVID-19 recovery, patients should lead a healthy lifestyle, have nutritious foods to enhance immunity and do regular physical activity, breathing exercises or yoga.[3] Likewise, HCW, in our survey, post-recovery was focussed on a nutritious diet (71%) and a majority (65%) were practising some form of physical activity, which was in tune with the recommendations. However, only 46% were taking health supplements. A majority of those taking supplements were having Vitamin C and other multivitamins. HCWs seem to be more aware of the role of Vitamin C in prevention and enhanced recovery as well as the anti-inflammatory, antioxidant and antiviral effects of Vitamin C.[15] About 22% of the HCW got their antibody levels checked post-COVID-19. Even though the level of antibody is highly variable post-COVID-19, antibody monitoring has been advised in studies to reduce reinfection.[16,17] However, with the advent of vaccines given to HCW on a priority basis, further recommendations are required and awaited. Post-vaccination with messenger RNA vaccine, mRNA-1273 and adequate neutralising antibodies have been detected on day 119 post-vaccination.[17] Natural infection without vaccination produces an unpredictable antibody longevity.[18,19] The HCW probably knew the fact that natural antibodies were not enough to provide reinfection, and thus, about 70% of HCWs in our survey were implementing infection control practice even after getting the recovery from the infection. However, they had the fear of contracting the virus again and risk of infecting family members. One positive outcome which we found in our survey was that up to 78% of HCWs did not report any psychological issues and 51% never had any anxiety issues. This is in contrast to the study done by Selvaraj et al. and Chaudhuri et al., where a majority of the HCWs had psychological morbidity and anxiety.[20,21] This variation and reduction in the anxiety and psychological issues could be due to two reasons. First, the participants in our survey had already suffered and successfully recovered from COVID-19 and that probably lead to reduction in the anxiety and psychological symptoms. Second, with the number of COVID-19 cases decreasing countrywide and vaccination drive being seen over the horizon at the time of the study, the HCW would have been relieved of the on-going stress. HCWs have been known to be more resolute and diligent at the workplace than general population.[22] With the initial tide of apprehension passing off, when there was no known effective treatment and no possibility of vaccination evident, HCWs have now become more resilient mentally while caring for COVID-19-positive patients. However, another worrisome fact is the recent appearance of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants in many nations with genetic variability.[23] Thus, the psychological issues faced by HCW may show waxing and waning as per the prevailing scenario. Factors such as effective COVID-19 treatment availability and vaccination may ameliorate the anxiety issues whereas the new genetic variations of SARSCoV-2 may accentuate the stress of HCW. Rather, financial stress due to hospital expenditure of self and family preoccupied the minds of the HCW post-COVID-19 recovery in up to 32% of respondents. Recommendations on wellness of HCW during pandemic era have suggested individualised hassle free access to health resources for HCW.[24] The same should also apply to their families, to relieve the stress of finances due to hospital expenditure.
COVID-19 being a multisystemic disease requires a vigilant follow-up post-recovery as the chronicity of the disease has been elucidated in literature.[25] HCWs who have recovered from COVID-19 have the simmering effects of the disease and urge for well-structured post-COVID-19 clinics. Such clinics will not only be of tremendous significance to our frontline warriors who have battled COVID-19 and got the initial victory, but also help us understand the disease course in the long run. Post-acute COVID-19 (“long COVID”) is the new pandemic which is exasperating our HCW and may strike those with mild COVID-19 disease as well.[26]
Our study had few limitations. Even though we intended to have a larger sample size, there was a lack of inclination to participate in the study from many HCWs who have recovered from COVID-19, due to a relatively smaller sample size. It was a single-centre study. Majority of our respondents were in the younger age group and the results may have been different if the majority were >60 years. We did not use any physical disability scale in our survey, which could have been more informative.
CONCLUSION
Health issues such as fatigue, headache and myalgia, loss of taste and smell continue to persist among HCW even after recovery from COVID-19, which is a quality of life concern. Most of the participants felt the need to set up post-COVID-19 health care units in all hospitals. A majority of HCWs have adopted a healthier lifestyle and pursue physical activity. Multivitamins and Vitamin C are the most common health supplements chosen by HCWs who have recovered from COVID-19. The fear of contracting the virus again, infecting family members, having post-COVID-19 complications and financial drain due to hospital expenses continue to impact the HCW in the post-COVID-19 recovery period.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Persistent symptoms 3 months after a SARS-CoV-2 infection: The post-COVID-19 syndrome? ERJ Open Res. 2020;6:542-2020.
- [Google Scholar]
- COVID-19: The case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395:1418-20.
- [CrossRef] [Google Scholar]
- Follow-up studies in COVID-19 recovered patients-Is it mandatory? Sci Total Environ. 2020;729:139021.
- [Google Scholar]
- Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2021;93:1013-22.
- [CrossRef] [Google Scholar]
- Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603-5.
- [CrossRef] [Google Scholar]
- Thyroid function analysis in 50 patients with COVID-19: A retrospective study. Thyroid. 2021;31:8-11.
- [CrossRef] [Google Scholar]
- COVID-19 and pulmonary rehabilitation: Preparing for phase three. Eur Respir J. 2020;55:2001822.
- [CrossRef] [Google Scholar]
- The post-COVID-19 functional status scale: A tool to measure functional status over time after COVID-19. Eur Respir J. 2020;56:2001494.
- [CrossRef] [Google Scholar]
- The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010;15:543-50.
- [CrossRef] [Google Scholar]
- One-year outcomes and health care utilization in survivors of severe acute respiratory syndrome. Arch Intern Med. 2007;167:1312-20.
- [CrossRef] [Google Scholar]
- Fatigue symptoms during the first year following ARDS. Chest. 2020;158:999-1007.
- [CrossRef] [Google Scholar]
- Clinic blueprint for post-coronavirus disease 2019 RECOVERY: Learning from the past, looking to the future. Chest. 2020;159:949-58.
- [CrossRef] [Google Scholar]
- British Thoracic Society survey of rehabilitation to support recovery of the post-COVID-19 population. BMJ Open. 2020;10:e040213.
- [Google Scholar]
- Possible application of high-dose vitamin C in the prevention and therapy of coronavirus infection. Glob Antimicrob Resist. 2020;23:256-62.
- [CrossRef] [Google Scholar]
- Preliminary study of the antibody level in confirmed patients with COVID-19 after discharge. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54:1448-52.
- [Google Scholar]
- Durability of responses after SARS-CoV-2 mRNA-1273 vaccination. N Engl J Med. 2021;384:80-82.
- [CrossRef] [Google Scholar]
- Humoral immune response to SARS-CoV-2 in iceland. N Engl J Med. 2020;383:1724-34.
- [CrossRef] [Google Scholar]
- Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;371:1-22.
- [CrossRef] [Google Scholar]
- Psychological impact of COVID-19 pandemic on health-care professionals in India-A multicentric cross-sectional study. Indian J Med Sci. 2020;72:141-7.
- [CrossRef] [Google Scholar]
- Weathering the storm: Psychological impact of COVID-19 pandemic on clinical and nonclinical healthcare workers in India. Indian J Crit Care Med. 2021;25:16-20.
- [CrossRef] [Google Scholar]
- Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am J Emerg Med. 2020;38:1530-1.
- [CrossRef] [Google Scholar]
- SARS-CoV-2 variants and ending the COVID-19 pandemic. Lancet. 2021;397:952-4.
- [CrossRef] [Google Scholar]
- The impact of COVID-19 on healthcare worker wellness: A scoping review. West J Emerg Med. 2020;21:1059-66.
- [CrossRef] [Google Scholar]
- Post-COVID-19 follow-up clinic: Depicting chronicity of a new disease. Acta Biomed. 2020;91:22-8.
- [Google Scholar]






