Translate this page into:
Primary Peritoneal Serous Carcinoma: A Rare Case and Palliative Approach
Address for correspondence: Dr. Viral M Bhanvadia; E-mail: drviral2001@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary peritoneal serous carcinoma (PPSC) is a rare primary malignancy that diffusely involves the peritoneum, indistinguishable clinically and histopathologically from primary serous ovarian carcinoma. The origin of PPSC has not been well characterized. Here we present a case of PPSC diagnosed in ultrasonography-guided fine needle aspiration cytology (FNAC) in a 76- old female presenting with ascites, abdominal pain, distension and constipation. PPSC is an unusual tumour but cytomorphology is distinctive enough to diagnose preoperatively. In the case report hereby described PPSC is an inoperable malignancy, hence chemotherapy and palliative care are the only offered treatment.
Keywords
Primary peritoneal serous carcinoma
Chemotherapy
Fine needle aspiration cytology
INTRODUCTION
Primary peritoneal serous carcinoma (PPSC) is a rare primary malignancy that diffusively involves the peritoneum, indistinguishable clinically and histopathologically from primary serous ovarian carcinoma.[1] Primary peritoneal carcinoma was first described in 1959 by Swerdlow.[2] The origin of PPSC has not been well characterized. The epithelial layer of the ovary and the peritoneum shares a common embryonic heritage, deriving from coelomic epithelium early in life. PPSC appears to be a part of the hereditary breast-ovarian cancer syndrome as the frequency of BRCA mutations in peritoneal and ovarian cancer cases is comparable.[3] Patients with germ line mutation of BRCA1 develop multifocal origin of PPSC.[45]
CASE REPORT
We present a case of PPSC of a 76- old female who presented with ascites, abdominal pain and distension, constipation, respiratory distress and weight loss. Patient is on treatment for hypertension and Ischemic heart disease. On gynecological examination, uterus and cervix were unremarkable, no adnexal mass was found but nodularity and hardening was felt in peritoneum/pouch of douglas. Patient was sent for Ultrasound (USG) examination of abdomen and pelvis that showed gross ascites and marked pelvic peritoneal thickening. On computerized tomography (CT scan) of the abdomen and pelvis omental caking, nodularity, pelvic peritoneal thickening and ascites were observed, uterus appears small and atrophic [Figures 1a and b]. Further Magnetic resonance imaging (MRI) was performed for evaluation of ovaries and adnexa. On MRI, uterus and both ovaries appear unremarkable and no adnexal mass was found [Figures 2a and b]. Preoperatively Serum CA-125 was 337 U/ml (normal range, 0-35 U/ml). Ascitic fluid cytology was positive for malignant cells. USG-guided fine needle aspiration cytology (FNAC) of thickened pelvic peritoneum Was performed and smears stained with Papanicolaou, hematoxylin and eosin stain showed three-dimensional clusters of malignant epithelial cells having eccentric round vesicular nuclei and prominent nucleoli. At places papillaroid, adenoid, cluster-like arrangement, and multinucleation of tumour cells are also seen [Figures 3 and 4a and b]. Considering cytological findings, radiological examination repeated and found no disease elsewhere, which favors the diagnosis of PPSC and advice for radical hysterectomy, omentectomy, and biopsy of thickened pelvic peritoneum to confirm the diagnosis. Peritonealbiopsy showed malignant stratified epithelial cells, papillary architecture along fibrovascular core and necrosis, suggest the diagnosis of primary peritoneal serous adenocarcinoma. Histopathologically, differential diagnosis includes malignant mesothelioma, metastatic peritoneal carcinomatosis, primary peritoneal psammoma carcinoma, and benign papillary mesothelioma. Immunohistochemistry stain is positive for CK7, ER, CA-125, WT1, P53 in PPSC and negative for calretinin and CK20 to confirm the diagnosis.
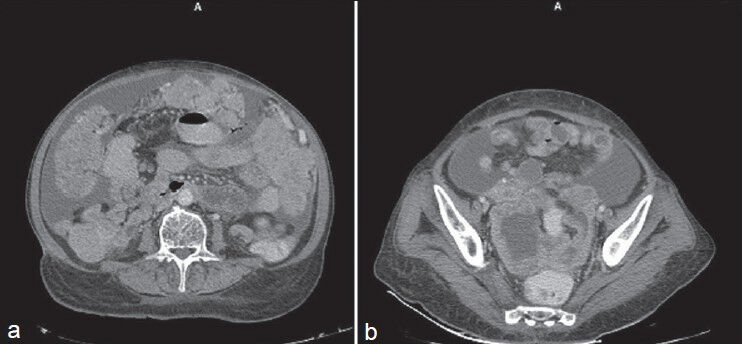
- (a) Contrast-enhanced CT scan showsomental caking and ascites (b) Contrast-enhanced CT scan shows ascites and pelvic peritoneal thickening
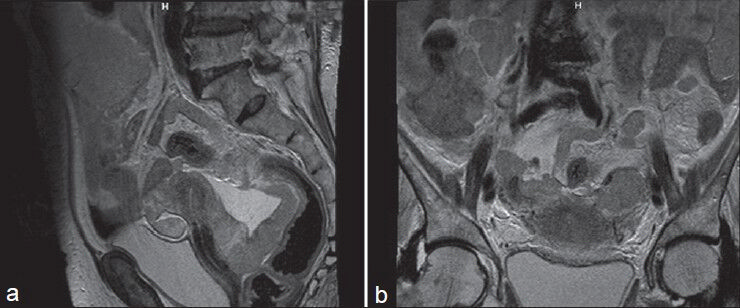
- (a) T2 MRI showsuterus appear small and atrophic and thickened pelvic pritoneum. (b) T2 weighted MRI shows uterus and both adnexa appear unremarkable
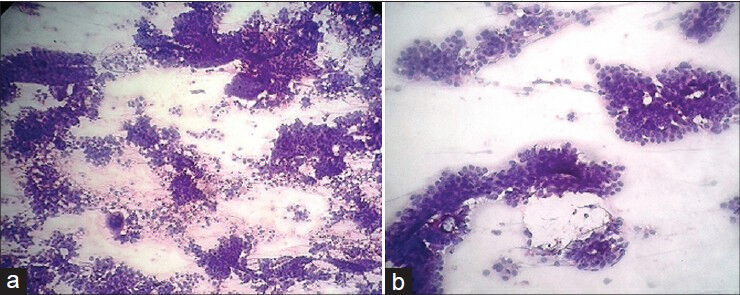
- (a) Hematoxylin and eosin stain (H and E stain), (40) shows three-dimensional clusters, papillaroid arrangement, and multinucleated giant cells. (b) H and E stain (100) shows palisading of typical tumour cells
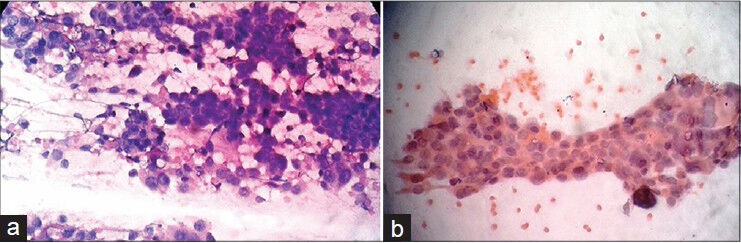
- (a) H and E stain (×400) shows sheets and clusters of tumour cells having eccentric nuclei, prominent nucleoli. (b) Papanicolaou stain (400) shows papillary cluster of tumour cells
DISCUSSION
Primary peritoneal serous carcinoma is a rare tumor of similar histogenic origin as primary ovarian carcinoma, which spreads widely on the peritoneal surfaces involving mostly the omentum with minimal or no ovarian involvement. The incidence of PPSC is considerably lower than that of epithelial ovarian cancer, 6.78 cases per million versus 120.5 cases per million, respectively.[6]
In 1993, the diagnostic criteria of PPSC described by the Gynecology Oncology Group include (1) ovaries must be normal size or enlarged as result of benign process (2) extraovarian involvement is must be greater than the surface involvement of either ovary (3) ovarian involvement must be absent, confined to the ovarian surface epithelium without stromal invasion, or involve the cortical stroma with a maximal tumour dimension of less than 5x5 mm2.[7] This criteria will help us to differentiate it from primary serous carcinoma of ovary.
Clinically, women diagnosed with PPSC are treated using the same surgical and chemotherapeutic approach as epithelial ovarian cancer because of the similarities in biological behavior. The management of PPSC consists of combining optimal surgical debulking with an intravenous Taxol and Platin doublet chemotherapy of six cycles may offer the patient the most effective treatment. As our patient's condition was advance TNM stage-IV at presentation and co-existent cardiovascular morbidity considered as inoperable, planned for palliative chemotherapy, started intravenous paclitaxel 175 mg/m2 over 3 h followed by intravenous carboplatin AUC 5 over 2 h given on day 1. Same regime was repeated every 21 days for three cycles. Patient was then evaluated for improvement of symptoms clinically, radiologically, serum CA-125 level, and tolerance of chemotherapy.
In a view of patient having aforementioned symptoms, early incorporation of palliative care into active management was decided and applied accordingly. There was symptomatic improvement of abdominal pain and distension, constipation, vomiting, and respiratory distress due to palliative care. Palliative care strategy should be individualized to each patient with intent to provide symptomatic improvement. Patient responding well to palliative treatment in follow up after 6 months. Prognosis of PPSC remained poor, overall median survival was 23.1 months. 5 year survival rate ranged from 0-26.5%.[89]
In conclusion, PPSC is a rare tumour and should be included in differential diagnosis in any postmenopausal woman having peritoneal thickening, omental nodules, and ascites with or without ovarian involvement clinically and radiologically. Nowadays, detection of this rare entity has increased due to refinement and awareness of criteria and usage of image-guided FNAC technique for diagnosis of the tumour. USG-guided FNAC of peritoneal thickening or effusion cytology is distinctive enough to suggest correct diagnosis of this unusual tumour preoperatively. In our case, though we were not able to deliver optimum treatment to the patient, we could achieve best possible good quality of life and survival with chemotherapy and palliative care of mentioned symptoms.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Primary peritoneal serous carcinoma: A clinicopathological and immunohistochemical study of six cases. Int J Clin Exp Pathol. 2012;5:762-9.
- [Google Scholar]
- Mesothelioma of the pelvic peritoneum resembling papillary cystadenocarcinoma of the ovary; case report. Am J Obstet Gynecol. 1959;77:197-200.
- [Google Scholar]
- Rapidly Increasing Incidence of Papillary Serous Carcinoma of the Peritoneum in the United States: Fact or Artifact? Int J Cancer. 2009;124:2231-5.
- [Google Scholar]
- Evidence for a multifocal origin of papillary serous carcinoma of the peritoneum. Cancer Res. 1995;55:490-2.
- [Google Scholar]
- Molecular evidence for multifocal papillary serous carcinoma of the peritoneum in patients with germline BRCA1 mutations. J Natl Cancer Inst. 1998;80:841-5.
- [Google Scholar]
- Incidence of ovarian, peritoneal and fallopian tube carcinomas in the United States, 1995-2004. Cancer Epidemiol Biomarkers Prev. 2009;18:132-9.
- [Google Scholar]
- Extraovarian peritoneal serous papillary carcinoma: A case-control retrospective comparison to papillary adenocarcinoma of the ovary. Gynecol Oncol. 1993;50:347-51.
- [Google Scholar]
- Serous surface papillary carcinoma of the peritoneum: Clinical, radiologic and pathologic findings in 11 patients. AJR Am J Roentgenol. 2004;183:923-8.
- [Google Scholar]
- Clinical characteristics of primary peritoneal carcinoma. Cancer Res Treat. 2007;39:65-8.
- [Google Scholar]






