Translate this page into:
Quality of Life of patients with chronic kidney disease in Iran: Systematic Review and Meta-analysis
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Renal diseases are among the major health problems around the world that cause major changes in patients’ lifestyle and affect their quality of lives. The aim of this study was to evaluate the quality of life of patients with chronic kidney disease (CKD) in Iran through a meta-analysis.
Materials and Methods:
This study was conducted using authentic Persian and English keywords in the national and international databases including IranMedex, SID, Magiran, IranDoc, Medlib, Science Direct, Pubmed, Scopus, Cochrane, Embase, Web of Science, and Medline. The data were analyzed using meta-analysis (random effects model). Heterogeneity of studies was assessed using I2 index. In this study, SF-36: 36-Item Short Form health-related quality of life (HRQOL), kidney disease quality of life-SF (KDQOL-SF), KDQOL and KDQOL-SFTM questionnaires were used. Data were analyzed using STATA Version 11 software.
Results:
A total of 17200 individuals participated in 45 reviewed studies, and the mean score of CKD patients’ quality of life was estimated by SF-36 (60.31), HRQOL (60.51), and KDQOL-SF (50.37) questionnaires. In addition, meta-regression showed that the mean score of CKD patients’ quality of life did not significantly decrease during the past years.
Conclusion:
The mean score of quality of life of patients with CKD was lower in different dimensions in comparison with that of normal people. Therefore, interventional measures should be taken to improve the quality of life of these patients in all dimensions.
Keywords
Iran
kidney patients
meta-analysis
quality of life
renal patients
INTRODUCTION
Quality of life is an important criterion that illustrates the effectiveness of health care, health level, and well-being. It is a multidimensional concept that includes ability, function, health, well-being, and psychological state, which is defined by the World Health Organization as values, goals, standards, and individual interests.[1234] There is a relationship between diseases and quality of life. Quality of life can have a direct impact on physical performance, emotional, and physical problems, fatigue, mental health, social performance, physical pain, and general health.[5678910] Therefore, knowledge about chronic diseases, especially chronic kidney diseases (CKD) is very important in the evolution of patients’ health problems.[11121314]
CKD is one of the major public health problems worldwide.[151617] The incidence of chronic renal failure in the world is 242 cases per a million people, and 8% is added to this population each year.[1819] The population of patients with renal failure in Iran is 320,000.[2021] One of the ways to improve the condition of patients with chronic renal failure is hemodialysis.[1822] In addition to hemodialysis, peritoneal dialysis and kidney transplantation are the common alternative treatments.[23] The patients undergoing dialysis have to spend several hours of their lives in dialysis sessions (2–3 sessions each week), and these constraints affect the living conditions of these patients.[1824] In general, patients with CKD are affected by a wide range of physical, psychological, economic, and social problems[112526272829] which ultimately influence their quality of lives.[30]
Considering the contradictory results of previous studies and the importance of "quality of life" and its effects on the personal and social life in patients with CKD, the present study was carried out through meta-analysis to provide a general assessment of the quality of life of CKD patients in Iran.
MATERIALS AND METHODS
Search strategy
In this study, the quality of life in patients with CKD in Iran was examined using a systematic review and meta-analysis. To access the relevant Persian and English articles, national and international databases including IranMedex, SID, Magiran, IranDoc, Medlib, ScienceDirect, Pubmed, Scopus, Cochrane, Embase, Web of Science, and Medline were searched using related Persian keywords and their English equivalent ("Iran," "CKD Patients," "CKD," "Quality of Life") along with the logical combinations of these keywords. The Google Scholar search engine was also used to find relevant articles. References of related articles were searched to come up with an exhaustive search.[112526272829] The search was done on databases from 2005 to May 2017.
Inclusion and exclusion criteria
The inclusion criteria referred to the quality of life in patients with CKD in Persian and English from 2000 to 2017. The exclusion criteria included nonrandom sampling, insufficient data, and statistical population other than in patients with CKD.
In the first stage, 231 articles on the quality of life in patients with CKD were found. After reviewing the titles, 113 articles were excluded due to the problem of duplication. The abstracts of all remaining articles were reviewed, and 39 irrelevant articles were omitted. The full texts of the remaining articles were reviewed, and 34 articles were excluded in conformity with the exclusion criteria. In the end, 45 articles entered the qualitative assessment process [Chart 1].
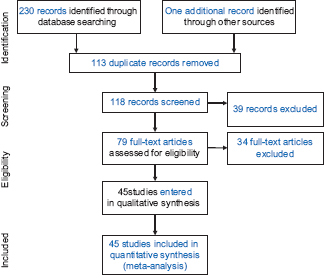
- Flowchart of steps involved in entering the studies into the systematic review and meta-analysis process
Qualitative assessment of studies
To assess the quality of studies, the preferred reporting items for systematic review and meta-analysis,[31] which is a checklist specifically designed for meta-analyses and systematic reviews, were used.
Data extraction
Two researchers independently extracted the data from the sources to minimize the errors in data reporting, and thereby increase the accuracy of the gleaned data. The researchers designed a checklist for extracting data from the sources (the items of researcher-made checklist were the name of the first author, the purpose of the study, the number of samples, the year and place of research, the type of kidney disease, the type of quality of life questionnaire, the average age of the individuals, and mean and standard deviation (SD) of different dimensions of the quality of life in in patients with CKD). Questionnaires used in the studies included the following:
SF-36 standard questionnaire
This is a short 36-item form consisting of two parts; the first part comprises demographic information, and the second part contains 11 questions that examine different aspects of health pertaining to quality of life. In fact, the second part of theSF-36 questionnaire is the same as health-related quality of life (HRQOL). These aspects include social function, limitations in the role due to physical problems, pain, mental health, limitations in the role due to emotional problems, and overall understanding of general health. Questions were rated by Likert Scale and ranged from 0 to 100, where higher points indicate a more favorable situation.[32333435]
The kidney disease quality of life-short form (KDQOL-SF) questionnaire, which is a multidimensional questionnaire that includes SF-36 questions and questions on CKD. The questionnaire assesses 12 factors of health and quality of life, including physical function, general health, the effects of CKD on life, imposed conditions, pain, sleep, social function, social support, energy, emotional roles, sexual function, and patient's satisfaction. Questions were rated from 0 to 100, where higher points indicate more favorable conditions.[3637]
Kidney disease quality of life-short form ™ questionnaire
This questionnaire is a specific tool for assessing the quality of life in hemodialysis patients and includes two general and specific scales on the quality of life. The general quality of life scale consists of two subscales of physical conditions and emotional conditions. The physical subscale contains four areas of general health (with 6 items), physical function (10 items), playing physical role (including 4 items), and physical pain (including 3 items). The subscale comprised emotional conditions comprising three areas of playing emotional role (3 items), social function (including 2 items), and mental health (including 8 items). The specific dimension of the research tool consisted of nine areas including CKD-related constraints (11 items), health-related mental problems (6 items), health-related physical function (12 items), general health (3 items), health-related family satisfaction (4 items), sleep status (score from 0 to 100), health-related occupational status (3 items), sexual issues (2 items), and satisfaction with care and ward staff (3 items). Each area has 100 points. This questionnaire is a multidimensional, valid, and reliable tool that addresses all aspects of the SF-36 questionnaire.[38]
Statistical analysis
The reviewed studies were combined based on the number of samples, mean, and SD. The standard error of the mean was calculated using SD/sqrt (n) equation according to the normal distribution. To evaluate the heterogeneity of the studies, Q test and I2 index were used. Due to the heterogeneity in the studies, the random-effects model was used to combine the results of the studies. The significance level of the test was considered P < 0.05. Data were analyzed using Stata is a general-purpose statistical software package created in 1985 by StataCorp. Most of its users work in research, especially in the fields of economics, sociology, political science, biomedicine and epidemiology
RESULTS
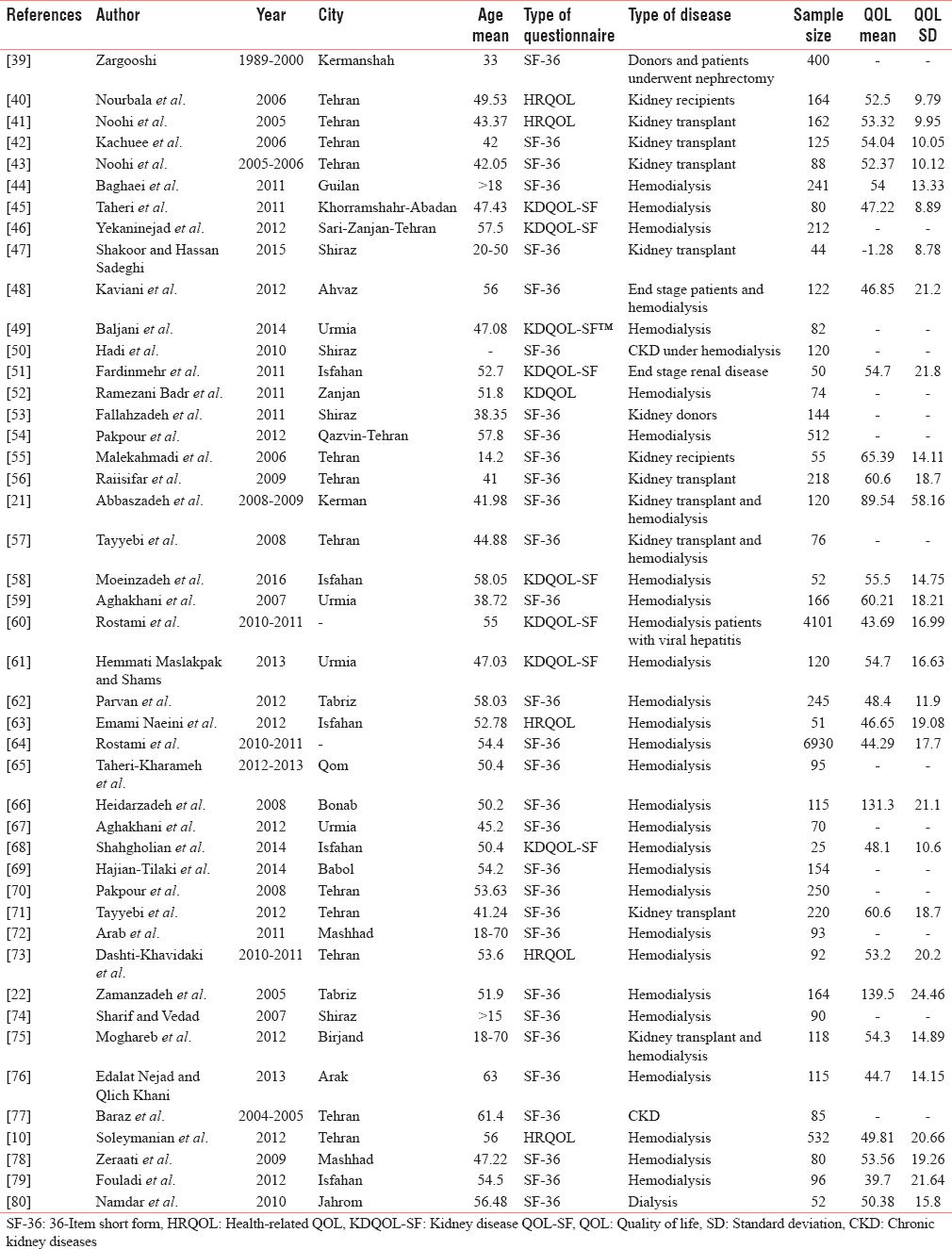
In 45 studies with a sample size of 17,200 people, the mean score of "quality of life" in CKD patients based on SF-36 questionnaire was 60.31% (95% confidence interval [CI]: 69.00%–51.62%), it was 51.60% (95% CI: 53.45%–49.75%) according to HRQOL questionnaire and 50.37% (95% CI: 54.77%–45.96%) based on KDQOL-SF questionnaire. Considering the heterogeneity of the studies in focus, the CI for each study based on the random effects model is presented in Figure 1 and Tables 1, 2.
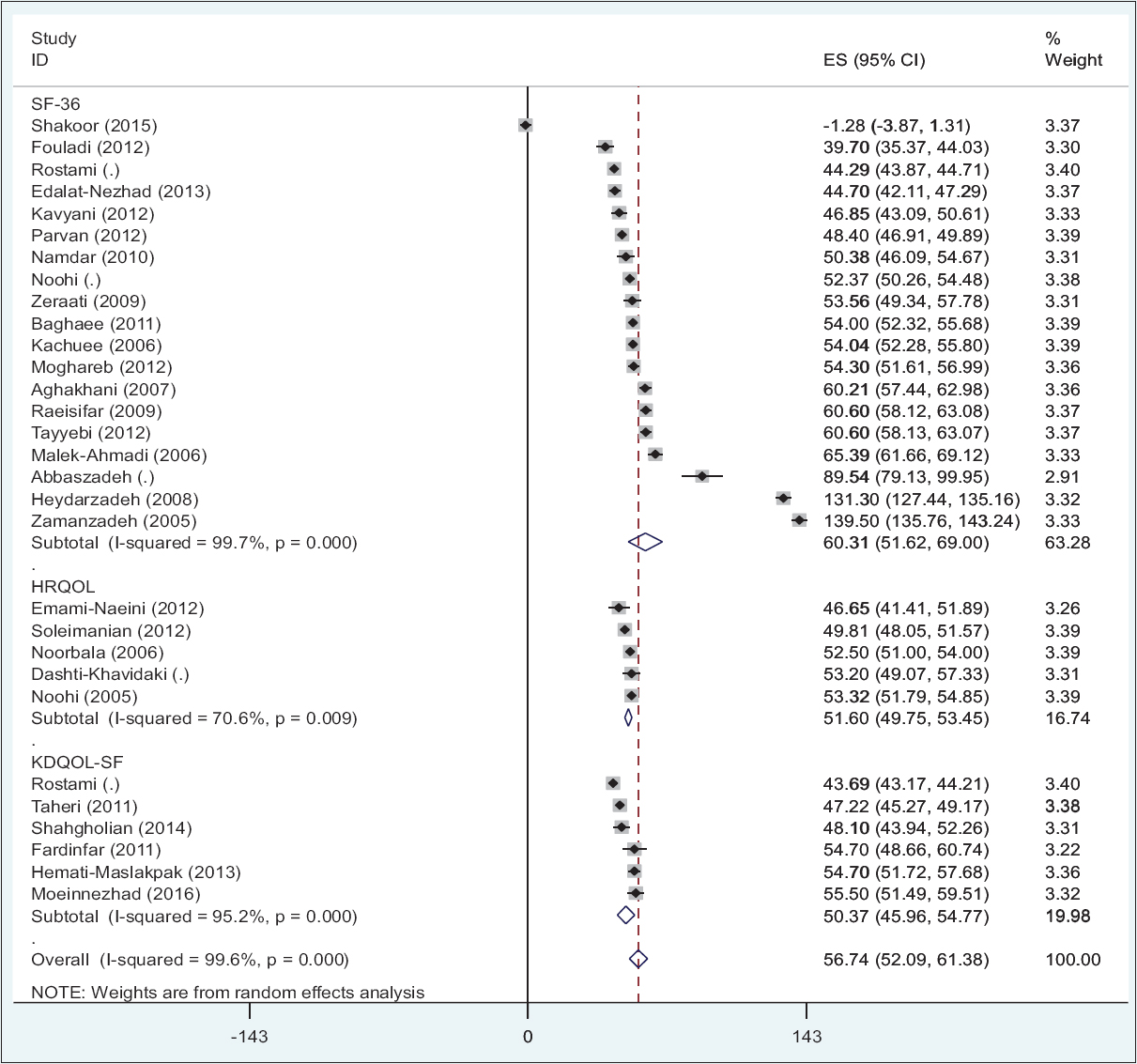
- Average quality of life in patients with chronic kidney disease in Iran (95% confidence interval) based on questionnaire according to random effects model. The middle point of each segment shows the quality of life score in chronic kidney disease patients in each study

DISCUSSION
In 45 studies with a sample size of 17,200 people, the mean score of the quality of life in patients with CKD based on SF-36, HRQOL, and KDQOL-SF questionnaires was 60.31, 51.60, and 50.37%, respectively. However, the mean score of the "quality of life" based on KDQOL-SF™ and KDQOL questionnaires was not calculated since each of them was only used in a single study
According to meta-regression diagram, there is no significant relationship between the quality of life in patients with CKD and the number of research samples, that is, with an increase in the number of research samples, the mean score of the quality of life in patients with CKD decreased, but this reduction is not statistically significant (P = 0.502). In the above diagram, the size of the circle shows the magnitude of the sample size [Figure 2]. In Figure 3, meta-regression model showed that there is no significant relationship between the quality of life in patients with CKD and the year of study. In other words, during the studied years, the quality of life in patients with CKD in Iran has decreased, but this decline is not statistically significant (P = 0.07).
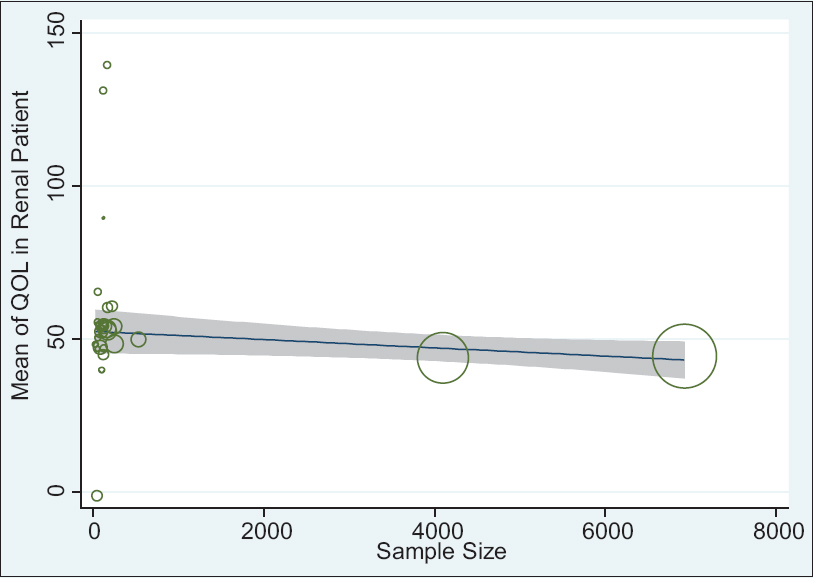
- The relationship between quality of life in chronic kidney disease patients and number of research samples using meta-regression
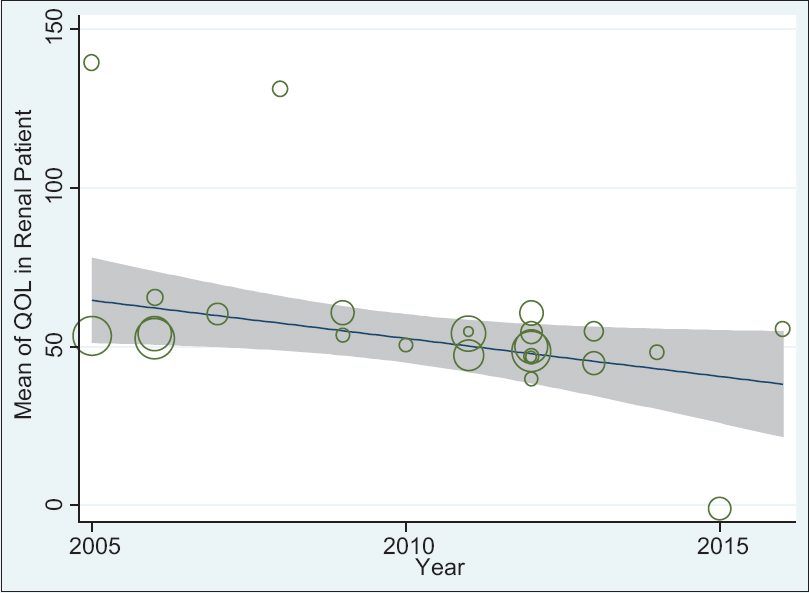
- The relationship between quality of life in patients with chronic kidney disease and years of research using meta-regression
Different studies show that quality of life in patients undergoing dialysis in Iran is lower than that of other chronic diseases.[81] In a study by Vázquez et al. in 2004, there were clear differences between men and women with CKD compared to the normal population in terms of quality of life (physical function, limited role due to mental problems, social function, and general health), while women had a worse situation.[82] In another study, among hemodialysis patients in Saudi Arabia in 2011, AL-Jumaih et al. showed that the majority of patients had limited physical role, emotional role, job status, and cognitive function and had poor quality of life.[83] In a study by Nonoyama et al. in Toronto, Canada, it was found that the majority of hemodialysis patients had average quality of life.[84] In a study by Chow and Wong, dialysis patients had the lowest quality of life scores in terms of physical health, social function, and dimensions of CKD including job status and burden of the disease.[85] In studies conducted by Cleary and Drennan and Vasilieva, the mean score for physical and mental health was low and patients had poor quality of life.[8687]
The mean score of diabetic patients’ quality of life in Iran estimated by SF-36 was 59.94 (CI 95%: 36.78–83.10).[88] The mean score of heart patients’ quality of life in Iran was 42.09 (CI 95%: 19.90–64.29).[89] Among 17 accomplished studies in Iran with the sample size of 1476 from 2003 to 2015, the average quality of life score for patients with cancer in Iran was 42 (CI 95%: 34.05–49.96).[90]
In other studies conducted in Iran, people over 50 had significantly lower scores in physical, psychological, and renal domains compared with younger people.[91] In the study of Baraz et al., the highest scores of quality of life before intervention were related to physical function (60.3%) and social function (60%). The lowest scores were those of emotional role (41.9%) and health perception (43.5%).[92] A study by Namadi and Movahhedpour demonstrated that 52.1% of hemodialysis patients had a moderate quality of life.[93] In a study by Raiisifar et al., the quality of life in patients who underwent kidney transplantation in Tehran in 2009 was assessed; they found that the mean and SD of quality of life was 60.6%.[56] Considering the different accessible data for the quality of life in patients with CKD, we used the meta-analysis method to obtain an accurate estimate of the quality of life in these patients.
Limitations of the study
Due to the different types of questionnaires used in the reviewed articles, the difference in scoring the questions of the respective questionnaires, and the difference in the number of questions in questionnaires, we could not combine the results of different questionnaires and report accurate statistics on the quality of life in patients with CKD in general and for various dimensions. Because of the variety of questionnaires, we did not manage to estimate the average score of the quality of life in patients with CKD in terms of type of disease, age, and place of research.
CONCLUSION
The mean score for quality of life of patients with CKD was estimated by SF-36 (60.31), HRQOL (60.51), and KDQOL-SF (50.37) questionnaires. In addition, meta-regression showed that the mean score of these patients’ quality of life has not significantly decreased during the past few years. The mean score of quality of life for patients with CKD was lower in different dimensions in comparison with that of normal people. The mean score of quality of life of patients with CKD in Iran was more than those of patients with heart diseases, diabetic patients, and patients with cancer.[9495] Therefore, interventional measures should be taken to improve the quality of life of these patients in all dimensions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Health-related quality of life in nephrology research and clinical practice. Semin Dial. 2005;18:82-90.
- [Google Scholar]
- The relationship between disease features and quality of life in patients with cancer – I. Cancer Nurs. 2001;24:490-5.
- [Google Scholar]
- The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc Sci Med. 1995;41:1403-9.
- [Google Scholar]
- The of education on quality of life in menopausal women referring to Shiraz Motahhari clinic in 2004. J Birjand Univ Med Sci. 2009;16:39-45.
- [Google Scholar]
- A comparison of the effects of pilates and McKenzie training on pain and general health in men with chronic low back pain: A Randomized trial. Indian J Palliat Care. 2017;23:36-40.
- [Google Scholar]
- The effect of family training and support on the quality of life and cost of hospital readmissions in congestive heart failure patients in Iran. Appl Nurs Res. 2016;31:165-9.
- [Google Scholar]
- Effect of progressive muscle relaxation on the fatigue and quality of life among Iranian aging persons. Acta Med Iran. 2016;54:430-6.
- [Google Scholar]
- The effect of education on quality of life in patients under interferon therapy. Hepat Mon. 2010;10:218-22.
- [Google Scholar]
- Health related quality of life in family caregivers of patients suffering from mental disorders. J Clin Diagn Res. 2016;10:VC05-9.
- [Google Scholar]
- Clinical outcomes and quality of life in hemodialysis diabetic patients versus non diabetics. J Nephropathol. 2017;6:81-9.
- [Google Scholar]
- Aggravation of chronic kidney disease by inflammatory factors; a narrative review on current concepts. J Renal Endocrinol. 2016;2:e05.
- [Google Scholar]
- Effect of booklet and combined method on parents’ awareness of children with beta-thalassemia major disorder. J Pak Med Assoc. 2008;58:485-7.
- [Google Scholar]
- Ischemic nephropathy; new concepts on its pathophysiology. Angiol Persica Acta. 2016;1:e03.
- [Google Scholar]
- Clinical practice guidelines for chronic kidney disease in adults: Part I. Definition, disease stages, evaluation, treatment, and risk factors. Am Fam Physician. 2004;70:869-76.
- [Google Scholar]
- The care preferences of patients under hemodialysis. J Renal Inj Prev. 2017;6:210-215.
- [Google Scholar]
- Forecast of the number of patients with end-stage renal disease in the United States to the year 2010. J Am Soc Nephrol. 2001;12:2753-8.
- [Google Scholar]
- Prevalence of CKD in the United States: A sensitivity analysis using the National Health and Nutrition Examination Survey (NHANES) 1999-2004. Am J Kidney Dis. 2009;53:218-28.
- [Google Scholar]
- Comparative assessment of quality of life in hemodialysis and kidney transplant patients. J Shahid Sadoughi Univ Med Sci. 2010;18:461-8.
- [Google Scholar]
- Relationship between quality of life and social support in hemodialysis patients in Imam Khomeini and sina educational hospitals of Tabriz university of medical science. Med J Tabriz Univ Med Sci. 2007;29:49-54.
- [Google Scholar]
- Evaluation of hemodialysis A dequacy on patients undergoing hemodialysis in Razi hospital in Rasht. J Guilan Univ Med Sci. 2007;17:44-9.
- [Google Scholar]
- Coping strategies and health-related quality of life among spouses of continuous ambulatory peritoneal dialysis, haemodialysis, and transplant patients. J Adv Nurs. 2000;31:1398-408.
- [Google Scholar]
- Administration of herbal drugs in geriatric individuals;trends on its helps and hazards. Geriatr Persia. 2017;1:e01.
- [Google Scholar]
- The epidemic of pediatric chronic kidney disease: The danger of skepticism. J Nephropathol. 2012;1:61-4.
- [Google Scholar]
- Psychological impact of chronic kidney disease among children and adolescents: Not rare and not benign. J Nephropathol. 2013;2:1.
- [Google Scholar]
- Chronic kidney disease in children: A report from a tertiary care center over 11 years. J Nephropathol. 2012;1:177-82.
- [Google Scholar]
- Socioeconomic links to health-related quality of life, anxiety, and depression in kidney transplant recipients. Iran J Kidney Dis. 2009;3:40-4.
- [Google Scholar]
- Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
- [Google Scholar]
- Quality of life in hemodialysis, peritoneal dialysis, and transplantation patients. Transplant Proc. 2007;39:3047-53.
- [Google Scholar]
- Assessment of health-related quality of life in renal transplant and hemodialysis patients using the SF-36 health survey. Urology. 2000;56:201-6.
- [Google Scholar]
- Depression and quality of life in living related renal transplantation. Transplant Proc. 2007;39:1791-3.
- [Google Scholar]
- Effects of applying continuous care model on quality of life in hemodialysis patients. Razi J Med Sci. 2006;13:123-34.
- [Google Scholar]
- Validation of the KDQOL-SF: A dialysis-targeted health measure. Qual Life Res. 2002;11:437-47.
- [Google Scholar]
- Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res. 1994;3:329-38.
- [Google Scholar]
- Pain affects health-related quality of life in kidney transplant recipients. Transplant Proc. 2007;39:1126-9.
- [Google Scholar]
- Anxiety and depression are correlated with higher morbidity after kidney transplantation. Transplant Proc. 2007;39:1074-8.
- [Google Scholar]
- Sleep quality and its correlates in renal transplant patients. Transplant Proc. 2007;39:1095-7.
- [Google Scholar]
- Are all domains of quality of life poor among elderly kidney recipients? Transplant Proc. 2007;39:1079-81.
- [Google Scholar]
- Redictive personal factors of quality of life in hemodialysis patient. J Holist Nurs Midwifery. 2015;24:9-19.
- [Google Scholar]
- Validity and reliability of the kidney disease quality of life-short form (KDQOL-SF™ 1.3) in Iranian patients. J North Khorasan Univ Med Sci. 2012;4:261-73.
- [Google Scholar]
- The effects of 10 weeks concurrent aerobic and strength exercise on quality of life and resilience of kidney transplant patients. Int J Appl Exerc Physiol. 2015;4:1-8.
- [Google Scholar]
- Life quality and health status correlation in hemodialysis patients with end-stage renal disease from Ahvaz university of medical sciences affiliated hospitals, 2012. Jundishapur J Chronic Dis Care. 2013;2:39-47.
- [Google Scholar]
- The effect of self management programs on the quality of life in patients under going hemodialysis. J Urmia Nurs Midwifery Fac. 2014;12:815-24.
- [Google Scholar]
- Health-related quality of life in chronic renal failure patients receiving hemodialysis. Payesh. 2010;9:349-54.
- [Google Scholar]
- The validity and reliability of the persian version of kidney disease quality of life questionnaire-short form (KDQOL-SF) in Iranian patients. J Isfahan Med Sch. 2012;29:1-10.
- [Google Scholar]
- Quality of life and related factors in hemodialysisPatients referred to teaching hospitals in Zanjan. J Neyshabur Univ Med Sci. 2016;4:57-64.
- [Google Scholar]
- Comparison of health status and quality of life of related versus paid unrelated living kidney donors. Am J Transplant. 2013;13:3210-4.
- [Google Scholar]
- A case-control study on oral health-related quality of life in kidney disease patients undergoing haemodialysis. Clin Oral Investig. 2015;19:1235-43.
- [Google Scholar]
- Importance of socioeconomic, clinical, and psychological factors on health-related quality of life in adolescents after kidney transplant. Exp Clin Transplant. 2011;9:50-5.
- [Google Scholar]
- An investigation of quality of life in kidney transplant patients. Iran J Crit Care Nurs. 2011;4:149-52.
- [Google Scholar]
- Comparison of quality of life in hemodialysis and renal transplantation patients. Iran J Crit Care Nurs. 2010;3:7-8.
- [Google Scholar]
- Effects of omega-3 fatty acid supplementation on serum biomarkers, inflammatory agents, and quality of life of patients on hemodialysis. Iran J Kidney Dis. 2016;10:381-7.
- [Google Scholar]
- Quality of life during hemodialysis and study dialysis treatment in patients referred to teaching hospitals in Urmia-Iran in 2007. Caspian J Intern Med. 2011;2:183-8.
- [Google Scholar]
- Health related quality of life in Iranian hemodialysis patients with viral hepatitis: Changing epidemiology. Hepat Mon. 2013;13:e9611.
- [Google Scholar]
- A comparison of face to face and video-based self care education on quality of life of hemodialysis patients. Int J Community Based Nurs Midwifery. 2015;3:234-43.
- [Google Scholar]
- Assessment of quality of life in patients undergoing continuous hemodialysis in four hospitals of East Azarbayjan, in 2012. Razi J Med Sci. 2014;21:19-28.
- [Google Scholar]
- Effects of oral L-carnitine supplementation on lipid profile, anemia, and quality of life in chronic renal disease patients under hemodialysis: A Randomized, double-blinded, placebo-controlled trial. J Nutr Metab. 2012;2012:510483.
- [Google Scholar]
- Health-related quality of life in hemodialysis patients: An Iranian multi-center study. Nephrourol Mon. 2013;5:901-12.
- [Google Scholar]
- Negative religious coping, positive religious coping, and quality of life among hemodialysis patients. Nephrourol Mon. 2016;8:e38009.
- [Google Scholar]
- Relationship between quality of life and self-care ability in patients receiving hemodialysis. Iran J Nurs Midwifery Res. 2010;15:71-6.
- [Google Scholar]
- The impact of education on nutrition on the quality of life in patients on hemodialysis: A comparative study from teaching hospitals. Saudi J Kidney Dis Transpl. 2012;23:26-30.
- [Google Scholar]
- The effect of tai chi exercise on quality of life in hemodialysis patients. Iran J Nurs Midwifery Res. 2014;19:152-8.
- [Google Scholar]
- A comparison of health-related quality of life in patients with renal failure under hemodialysis and healthy participants. Saudi J Kidney Dis Transpl. 2017;28:133-40.
- [Google Scholar]
- Health-related quality of life in a sample of Iranian patients on hemodialysis. Iran J Kidney Dis. 2010;4:50-9.
- [Google Scholar]
- Measuring health related quality of life (hrqol) in renal transplant patients: Psychometric properties and cross-cultural adaptation of kidney transplant questionnaire (ktq-25) in persian. Nephrourol Mon. 2012;4:617-21.
- [Google Scholar]
- A sham-controlled trial of acupressure on the quality of sleep and life in haemodialysis patients. Acupunct Med. 2016;34:2-6.
- [Google Scholar]
- The use of pharmaceutical care to improve health-related quality of life in hemodialysis patients in iran. Int J Clin Pharm. 2013;35:260-7.
- [Google Scholar]
- The relationship between mental health and quality of life of hemodialysis patients referred to hospitals affiliated to Shiraz university of medical sciences. IJN. 2007;20:61-9.
- [Google Scholar]
- Quality of life in hemodialysis and kidney transplantation patients in Birjand, 2012. Mod Care J. 2014;11:127-35.
- [Google Scholar]
- Quality of life and sleep in hemodialysis patients. Saudi J Kidney Dis Transpl. 2013;24:514-8.
- [Google Scholar]
- Correlation of quality of sleep or quality of life and some of blood factors in hemodialysis patients. J Shahrekord Univ Med Sci. 2008;9:67-74.
- [Google Scholar]
- Comparison of quality of life between hemodialysis and peritoneal dialysis patients in Imam Reza and Ghaem hospital dialysis centers in Mashhad. Med J Mashhad Univ Med Sci. 2010;53:169-76.
- [Google Scholar]
- Investigation of relationship betweenpositive psychological variables (spirituality and hope) psychopathology (depression, stress, anxiety) and quality of life inhemodialysis patients Isfahan – 2012. J Res Behav Sci. 2014;11:567-77.
- [Google Scholar]
- Health related quality of life in dialysis patients. J Jahrom Univ Med Sci. 2013;10:19-27.
- [Google Scholar]
- Effect of physical exercises on quality of life in hemodialysis patients. Med J Tabriz Univ Med Sci. 2008;30:51-5.
- [Google Scholar]
- Differences in health-related quality of life between male and female hemodialysis patients. Nefrologia. 2004;24:167-78.
- [Google Scholar]
- A study of quality of life and its determinants among hemodialysis patients using the KDQOL-SF instrument in one center in Saudi Arabia. Arab J Nephrol Transplant. 2011;4:125-30.
- [Google Scholar]
- Exercise program to inhance physical performance and quality of life of older hemodialysis patients: A feasibility study. Int Urol Nephrol. 2010;42:1125-30.
- [Google Scholar]
- Health-related quality of life in patients undergoing peritoneal dialysis: Effects of a nurse-led case management programme. J Adv Nurs. 2010;66:1780-92.
- [Google Scholar]
- Quality of life of patients on haemodialysis for end-stage renal disease. J Adv Nurs. 2005;51:577-86.
- [Google Scholar]
- Quality of life in chronic hemodialysis patients in Russia. Hemodial Int. 2006;10:274-8.
- [Google Scholar]
- Quality of life in diabetes patients in Iran: A systematic review and meta-analysis method. Int J Pharm Technol. 2016;8:21608-18.
- [Google Scholar]
- Quality of life in heart patients in Iran: A systematic review and meta-analysis method. Pharma Chem. 2016;8:27-34.
- [Google Scholar]
- The quality of life in cancer patients in Iran: A systematic review by using meta-analysis. Koomesh. 2016;18:1-12.
- [Google Scholar]
- Contributing factors in health-related quality of life assessment of ESRD patients: A single center study. Nephrourol Mon. 2009;1:129-36.
- [Google Scholar]
- The effect of self care educational program on decreasing the problems and improving the quality of life of dialysis patients. Hayat. 2005;11:51-62.
- [Google Scholar]
- Quality of life in patients after renal transplantation in comparison with intermittent hemodialysis. J Ardabil Univ Med Sci. 2009;9:171-9.
- [Google Scholar]
- The outcomes of stress exposure in hemodialysis patients. J Renal Inj Prev. 2017;6:275-81.
- [Google Scholar]
- Comparison of two interventions of increased blood f low rate and high-f lux filters on hemodialysis adequacy and complications; a quasi-experimental study. J Renal Inj Prev. 2017;6:247-52.
- [Google Scholar]






