Translate this page into:
Role of Electro-Therapeutic Modalities in Breast Cancer-Related Lymphedema and Shoulder Dysfunction: A Systematic Review and Meta-Analysis
*Corresponding author: Asmita Shrestha, Department of Oncology Physiotherapy, KAHER Institute of Physiotherapy, Belagavi, Karnataka, India. asmitashresthapt@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pattanshetty R, Shrestha A, Pawar N. Role of Electro-Therapeutic Modalities in Breast Cancer-Related Lymphedema and Shoulder Dysfunction: A Systematic Review and Meta-Analysis. Indian J Palliat Care. doi: 10.25259/IJPC_324_2024
Abstract
Breast cancer-related lymphedema (BCRL) is one of the most significant complications among survivors, leading to physical as well as psycho-social issues such as pain, joint restriction, heaviness, body image issues, and overall affecting quality of life (QOL). Various electro-therapeutic modalities are being used for its treatment, which is proven to be safe and effective. This systematic review and meta-analysis aimed to explore the evidence of the effectiveness of electro-therapeutic modalities in BCRL and shoulder dysfunction. This systematic review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. Electronic search was conducted in PubMed, Scopus, physiotherapy evidence database (PEDro) and Cochrane databases for eligible studies. Quality assessment was conducted by the PEDro scale for Randomised Controlled Trials and Modified McMaster Critical Review Form for other studies. The primary outcomes were arm volume, circumference and shoulder range of motion (ROM). Secondary outcome measures were QOL by QOL scale and functional assessment of cancer therapy-breast (FACT-B), and shoulder pain and disability by disability of arm, shoulder and hand (DASH), Quick DASH (Q-DASH) and shoulder pain and disability index. A descriptive synthesis of the studies was done, followed by a meta-analysis carried by Stata version 16 software. Twenty-eight studies were included in the review, and six in the meta-analysis. In summary, we found that electro-therapeutic modalities significantly improve arm volume, arm circumference at wrist level and shoulder ROM of flexion, abduction and external rotation. However, there was no significant improvement in arm circumference below the elbow, the elbow or below the axilla. This systematic review and meta-analysis identified significant improvement in terms of arm volume, circumference, shoulder ROM, shoulder pain and disability and overall QOL in BCRL and shoulder dysfunction. This review recommends the utilisation of these modalities in a clinical setting.
Keywords
Breast cancer
Electro-therapeutic modalities
Lymphedema
INTRODUCTION
Cancer remains a leading cause of mortality worldwide. Global cancer observatory (GLOBOCAN) 2020 estimates that there were around 19.3 million new cases and 10 million deaths globally. Among these, breast cancer is the most prevalent, with nearly 2.26 million new diagnoses, representing 11.7% of all new cancer cases in 2020.[1] Despite this, survival rates have significantly improved, having doubled over the past 50 years. At present, the 5-year survival rate for breast cancer stands at 90%, yet the global burden of the disease continues to rise.[2]
The impressive survival rates are also accompanied by numerous late effects and long-term problems. It can involve both psycho-social challenges and physical effects of surgery or cancer treatments, such as fatigue, pain, lymphedema, physical limitations, peripheral neuropathy, osteoporosis, sleep disturbances, body image concerns, as well as financial, family and work-related issues.[3] These factors exhibit a considerable repercussion on the health-related quality of life (HRQoL) of survivors.[4]
Lymphedema is one of the most significant long-term complications in patients after the treatment of breast cancer.[5] Evidence suggests that more than one-fifth of breast cancer survivors will experience lymphedema.[6]
Lymphedema is a long-term, progressive condition marked by the excessive build-up of protein-rich fluid in the tissues, chronic inflammation and fibrosis, which results from damage or dysfunction in the lymphatic system. Breast cancer-related lymphedema (BCRL) leads to pain, joint restriction, discomfort, heaviness, as well as weakness in the affected extremity.[4]
Physiotherapists, as integral members of the multidisciplinary team, are vital in the care, management and rehabilitation of cancer patients, supporting them from diagnosis to end-of-life care. They are also responsible for the proper examination and management of side effects derived from cancer as well as from its treatment.[7] As an important part of the cancer continuum, various approaches of physical therapy can reduce the financial burden of disease, raise the likelihood of going back to work and ultimately improve the HRQoL among survivors.[8]
However, the rehabilitation of cancer patients is very challenging due to their medical complications and dynamic trajectory.[9] Various modalities such as ultrasound, cryotherapy, pneumatic compression, functional electrical stimulation (FES), extracorporeal shock wave therapy (ESWT), infra-red therapy (IRR), low-level light laser, transcutaneous electrical nerve stimulation (TENS) and scrambler therapy have proven to be safe and effective in those patients.[7-9]
Even though various modalities such as TENS, ESWT, IFT, FES, IRR, low-level laser therapy (LLLT) and scrambler therapy are proven to be sound and efficient in the treatment of breast cancer-treatment-related adverse effects, there is still a lack of knowledge among health care professionals regarding rehabilitation services, usage of electrotherapeutic modalities and their precautions.[10] This lack of awareness results in the underutilisation of these modalities in rehabilitation.[11] Hence, there is a need for an updated review regarding physiotherapeutic modalities used in cancer patients.[12]
Hence, this systematic review sought to examine the support for the effectiveness of electro-therapeutic modalities in treating BCRL and shoulder dysfunction and to provide a foundation for evidence-based practice in the field of oncology physiotherapy.
MATERIALS AND METHODS
This systematic review was conducted in alignment with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and ethical approval was granted by the Institutional Ethical Committee.[13] In line with PRISMA recommendations, the research question was defined as, ‘What is the role of electro-therapeutic modalities in the treatment of BCRL?’
Search strategy and eligibility criteria
A comprehensive digital search was performed for the studies published from January 2013 and December 2023. The search strategy was prepared in Population, Intervention, Comparison and Outcome format by the discussion among the authors and a professional librarian experienced in health science. It included four major databases: PubMed, Scopus, Physiotherapy evidence database (PEDro) () and Cochrane database. Various combinations of the following medical subject headings (MESH) phrases and keywords were used: ‘Lymphedema’, ‘electrotherapy’, ‘physiotherapy’, ‘laser’, ‘cold laser’, ‘low level light laser’, ‘Transcutaneous Electrical Nerve Stimulation (TENS)’, ‘Interferential Therapy (IFT)’, ‘Matrix Rhythm Therapy (MRT)’, ‘Scrambler/Calmer therapy’, ‘Pneumatic Compression Therapy’, ‘Therapeutic ultrasound’ and ‘Extra-corporeal shockwave therapy (ESWT)’. Boolean operators ‘AND’ and ‘OR’ were used to develop MESH terms and MESH strategies.
Articles were screened by both authors and selected using the eligibility criteria. Table 1 outlines the inclusion and exclusion criteria for the study. Eligible studies were quantitative and published between January 2013 and December 2023, including randomised controlled trials (RCTs), clinical trials (including quasi-experimental research), case series and case studies, with case reports also accepted. Participants were required to be adults (18+) with BCRL. The intervention involved electrotherapeutic methods such as TENS, ESWT, pneumatic compression therapy, IFT, low-level light laser, scrambler/calmer therapy, therapeutic ultrasound or MRT. Primary outcomes included volume, circumference and shoulder joint range of motion (ROM), while secondary outcomes focused on shoulder pain, disability and quality of life (QOL).
| Inclusion | Exclusion | |
|---|---|---|
| Design | Quantitative studies (January 2013–December 2023) Randomised controlled trials Clinical trials including quasi-experimental research Case series and Case studies Case reports |
Qualitative studies Study protocols Abstract only studies Grey literature Duplicate studies Languages other than English |
| Participants | People aged 18 years and above with breast cancer related lymphedema | Lymphedema not related to breast cancer surgery |
| Intervention | Electrotherapeutic modalities as
|
Any Japanese or Chinese intervention Acupuncture |
| Outcome measures | Primary: Volume, Circumference, Shoulder joint ROM Secondary: Shoulder pain and disability, QOL |
TENS: Transcutaneous electrical nerve stimulation, ESWT: Extracorporeal shockwave therapy, ROM: Range of motion, QOL: Quality of life
Excluded studies included qualitative research, study protocols, abstract-only publications, grey literature, duplicate studies and non-English language studies. Lymphedema unrelated to breast cancer surgery, Japanese or Chinese interventions and acupuncture were also excluded from the study. The complete texts were analysed, along with the reference list for any pertinent research that the digital search had overlooked. The reviewers worked independently, and in case of different outcomes, it was resolved through discussion.
Assessment of the characteristics of studies
Quality
Independent reviews and gradings of all included studies were conducted using the National Health and Medical Research Council’s hierarchy of evidence. For RCTs, the PEDro scale was applied, which includes 11 items, each worth 1 point if met, with higher scores indicating better methodological quality. For non-RCT studies, the Modified McMaster Critical Review Form for Quantitative Studies was applied, with scores given according to the research design and applicable elements, resulting in a maximum possible score of 14.
Participants
Studies were included if participants had lymphedema associated with breast cancer and were aged 18 and over.
Intervention
The review included various electro-therapeutic modalities used for treating BCRL, such as TENS, intermittent pneumatic compression therapy (IPCT), IFT, ESWT, low-level light laser, scrambler/calmer therapy, therapeutic ultrasound and MRT.
Outcome measures
The primary outcomes were arm volume, circumference and shoulder ROM of the affected arm. The secondary outcomes were QOL assessed by Lymphedema-QOL (LYM-QOL) scale and functional assessment of cancer therapy-breast (FACT-B), and shoulder pain and disability assessed by disability of arm, shoulder and hand (DASH), Quick DASH (Q-DASH) and shoulder pain and disability index (SPADI).
Data extraction and data analysis
Data extraction was carried out independently by two authors using Microsoft Excel. It included study characteristics such as authors, research design, data collecting year and publication, country of data collection, sample size, type of cancer, evaluated groups, electrotherapeutic modalities, co-intervention and evaluated outcomes, when they were evaluated, parameters of treatment, conclusion and adverse events. The outcomes, such as arm circumference, volume and shoulder ROM along with outcome measures such as DASH, SPADI and LYM-QOL questionnaire, were recorded. Following data extraction, the potential for conducting meta-analysis was determined by assessing statistical heterogeneity. The meta-analysis was done using the software Stata version 16. The studies that assessed arm circumference, volume and ROM included necessary data to perform meta-analysis; hence, only those studies were used for the quantitative evaluation. To homogenise the results, quantitative combination of subgroups was done like circumference at four different levels (wrist, forearm, elbow and arm) and ROM for three different movements (flexion, abduction and external rotation). The Cochran’s Chi-squared test (Q test) and I-squared test were used to evaluate statistical heterogeneity, and the continuous data were presented as mean ± standard deviation. To evaluate differences within and between studies, a random effects model (I2 value >50% and P < 0.01) was employed, and Cohen’s d effect size was employed as an estimate. The results were summarised using a forest plot, and any publishing or other bias was evaluated using a funnel plot.
RESULTS
Study selection process
The combined database searches resulted in 548 articles, and 382 duplicates were removed by using Zotero. After screening the titles and abstracts, 110 records were discarded, leaving 56 papers for detailed review. From these, 28 studies met the inclusion standards and were chosen for qualitative analysis, while six studies were included in the quantitative analysis. The selection process is depicted in Figure 1.
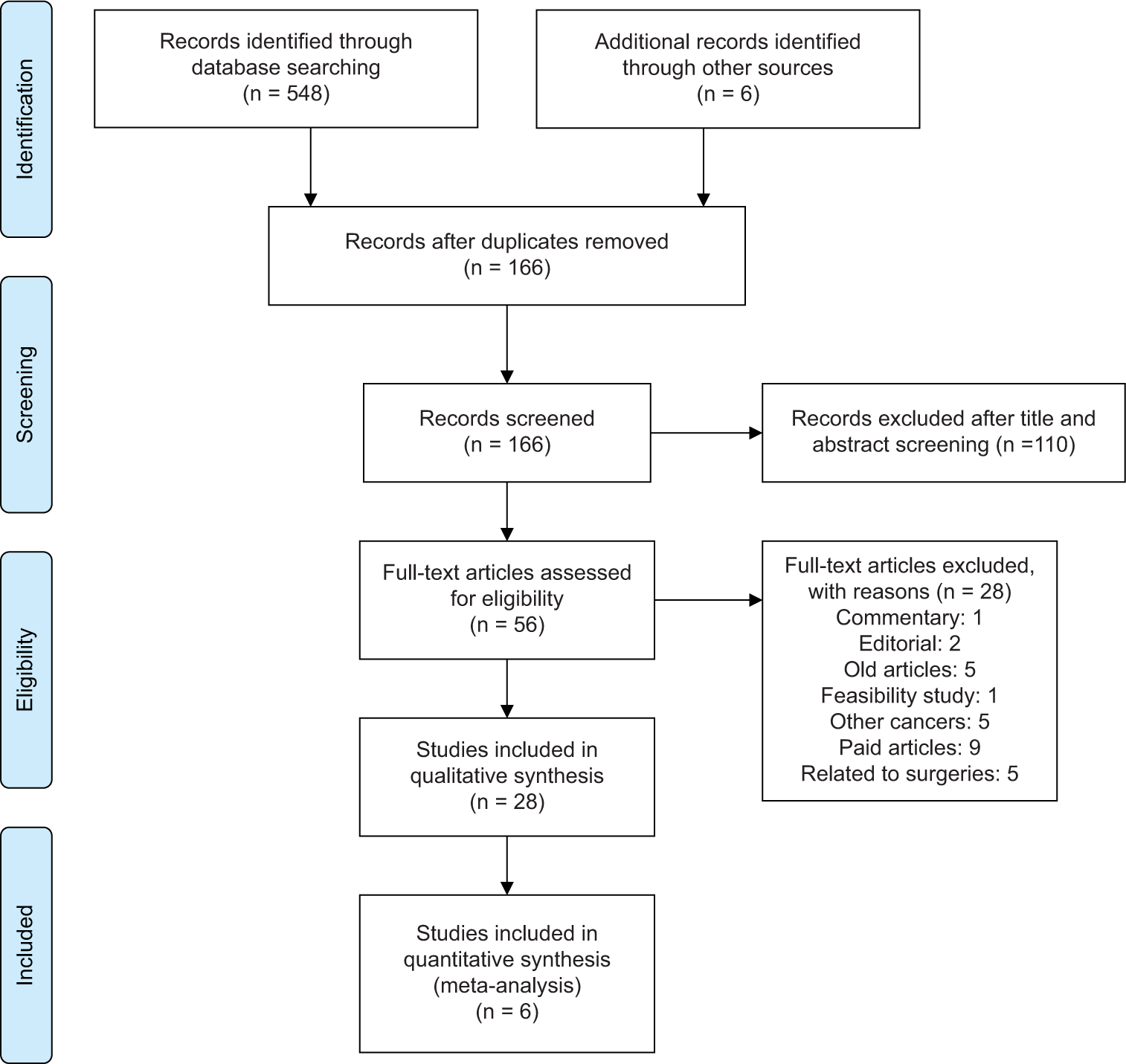
- Preferred reporting items for systematic reviews and meta-analyses flow chart showing literature search and selection process.
Study characteristics
All the studies published from January 2013 to December 2023 in the English language were included. Data extraction included 21 RCTs, four case-reports, two clinical trials and 1 pilot study conducted in 11 different countries, that is Turkey (six studies), India (four studies), United States (four studies), Egypt (four studies), Korea (three studies), Iran (two studies), Belgium (one study), Switzerland (one study), Spain (one study), Poland (one study) and Germany (one study). The sample size ranged from 1 to 76, and all participants had BCRL. The detailed characteristics are mentioned in Table 2.
| Studies | Year | Country | Study design | Participants | Intervention | Sample |
|---|---|---|---|---|---|---|
| Aykac Cebicci and Dizdar[17] | 2021 | India | RCT | BCRL | ESWT | 23 |
| Ridner et al.[29] | 2013 | USA | Randomised clinical trial | BCRL Stage I or II | LLLT | 46 |
| Abdelhalim and Samhan[14] | 2018 | Egypt | RCT | BCRL | ESWT and IPCT | 48 |
| Kilmartin et al.[33] | 2020 | USA | RCT | BCRL | LLLT | 22 |
| Diab et al.[37] | 2021 | Egypt | RCT | BCRL | IPCT | 30 |
| Rockson and Skoracki[15] | 2023 | USA | RCT | BCRL | APCD and NPCD | 14 |
| Gnanasekar[34] | 2020 | India | Case report | BCRL | MRT | 1 |
| Lee et al.[18] | 2020 | Korea | RCT | BCRL (Stage II) | ESWT | 30 |
| Uzkeser et al.[35] | 2015 | Turkey | RCT | BCRL | IPCT | 31 |
| Bhatikar[47] | 2018 | India | Case report | BCRL | MRT | 1 |
| Khalaf et al.[30] | 2013 | Switzerland | RCT | BCRL | HNLT | 30 |
| Pajero Otero et al.[36] | 2022 | Spain | RCT | BCRL | IPTC | 43 |
| Chmielewska et al.[39] | 2016 | Poland | RCT | BCRL | IPTC | 21 |
| Uzkeser et al.[19] | 2013 | Turkey | RCT | BCRL | PCT | 25 |
| Farhan et al.[20] | 2023 | Iran | Phase 2 clinical trial | BCRL | LLLT | 23 |
| Özçete and Eyigör[25] | 2020 | Turkey | Case report | BCRL | LLLT | 1 |
| Lee et al.[21] | 2022 | Korea | RCT | BCRL (Stage II) | ESWT | 28 |
| Joos et al.[32] | 2021 | Belgium | Pilot study | BCRL (Stage III) | ESWT | 10 |
| Pattanshetty et al.[38] | 2023 | India | Case report | BCRL | MRT | 1 |
| Storz et al.[31] | 2017 | Germany | RCT | BCRL | PBMT | 40 |
| Tastaban et al.[26] | 2020 | Turkey | RCT | BCRL | IPCT | 76 |
| Rockson et al.[27] | 2022 | USA | RCT | BCRL | APCD and NPCD | 50 |
| Hemmati et al.[16] | 2022 | Iran | RCT | BCRL | UST and FC | 39 |
| Tatar and Turhan[22] | 2022 | Turkey | RCT | BCRL | TENS | 30 |
| Selcuk Yilmaz and Ayhan[28] | 2023 | Turkey | RCT | BCRL (Stage II) | LLLT | 45 |
| Bae and Kim[23] | 2013 | Korea | Prospective clinical trial | BCRL (Stage III) | ESWT | 7 |
| El-Shazly et al.[6] | 2016 | Egypt | RCT | BCRL (Stage II or III) | ESWT | 60 |
| Mahran and Thabet[24] | 2015 | Egypt | RCT | BCRL (Stage II or III) | ESWT | 40 |
RCT: Randomised controlled trial, ESWT: Extracorporeal shock wave therapy, IPCT: Intermittent pneumatic compression therapy, TENS: Transcutaneous electrical nerve stimulation, MRT: Matrix rhythm therapy, PBMT: Photo-biomodulation therapy, BCRL: Breast cancer-related lymphedema, LLLT: Low level laser therapy, HNLT: Helium neon laser therapy, PCT: Pneumatic compression therapy, APCD: Advanced pneumatic compression device, NPCD: Non-pneumatic compression device, UST: Ultrasound therapy, FC: Faradic current
Quality
Quality assessment was performed by the PEDro scale for RCTs and the Modified McMaster Critical Review Form for other studies. The summary is mentioned in Tables 3 and 4.
| Studies | Eligibility | Random allocation | Concealed allocation | Baseline comparability | Blind subjects | Blind therapists |
|---|---|---|---|---|---|---|
| Aykac Cebicci and Dizdar[17] | Yes | Yes | No | Yes | No | No |
| Ridner et al.[29] | Yes | Yes | No | Yes | No | No |
| Abdelhalim and Samhan[14] | Yes | Yes | Yes | Yes | No | No |
| Kilmartin et al.[33] | Yes | Yes | Yes | Yes | Yes | Yes |
| Diab et al.[37] | Yes | Yes | Yes | Yes | No | Yes |
| Rockson and Skoracki[15] | Yes | Yes | Yes | No | No | No |
| Lee et al.[18] | Yes | Yes | No | Yes | No | No |
| Uzkeser et al.[35] | Yes | Yes | Yes | Yes | No | No |
| Khalaf et al.[30] | Yes | Yes | No | Yes | No | No |
| Pajero Otero et al.[36] | Yes | Yes | Yes | Yes | No | No |
| Chmielewska et al.[39] | Yes | Yes | No | Yes | No | No |
| Uzkeser et al.[19] | Yes | Yes | Yes | Yes | No | No |
| Farhan et al.[20] | Yes | No | No | Yes | No | No |
| Lee et al.[21] | Yes | Yes | No | Yes | No | No |
| Storz et al.[31] | Yes | Yes | Yes | Yes | Yes | No |
| Tastaban et al.[26] | Yes | Yes | Yes | Yes | No | No |
| Rockson et al.[27] | Yes | Yes | Yes | Yes | No | No |
| Hemmati et al.[16] | Yes | Yes | Yes | Yes | No | No |
| Tatar and Turhan[22] | Yes | Yes | Yes | Yes | No | No |
| Selcuk Yilmaz and Ayhan[28] | Yes | Yes | Yes | Yes | No | No |
| El-Shazly et al.[6] | Yes | Yes | No | Yes | No | No |
| Mahran and Thabet[24] | Yes | Yes | No | Yes | No | No |
| Studies | Blind assessors | Adequate follow-up | Intention to treat analysis | Between group comparison | Pointed estimated variability | Score |
| Aykac Cebicci and Dizdar[17] | No | Yes | Yes | Yes | Yes | 6 |
| Ridner et al.[29] | No | Yes | Yes | Yes | Yes | 6 |
| Abdelhalim and Samhan[14] | Yes | Yes | Yes | Yes | Yes | 8 |
| Kilmartin et al.[33] | Yes | Yes | Yes | Yes | Yes | 10 |
| Diab et al.[37] | No | Yes | Yes | Yes | Yes | 9 |
| Rockson and Skoracki[15] | No | Yes | Yes | Yes | Yes | 6 |
| Lee et al.[18] | No | Yes | Yes | Yes | Yes | 6 |
| Uzkeser et al.[35] | Yes | Yes | Yes | Yes | Yes | 8 |
| Khalaf et al.[30] | No | Yes | Yes | Yes | Yes | 6 |
| Pajero Otero et al.[36] | No | Yes | Yes | Yes | Yes | 7 |
| Chmielewska et al.[39] | No | Yes | Yes | Yes | Yes | 7 |
| Uzkeser et al.[19] | Yes | Yes | Yes | Yes | Yes | 8 |
| Farhan et al.[20] | No | Yes | Yes | Yes | Yes | 5 |
| Lee et al.[21] | No | Yes | Yes | Yes | Yes | 6 |
| Storz et al.[31] | Yes | Yes | Yes | Yes | Yes | 9 |
| Tastaban et al.[26] | No | Yes | Yes | Yes | Yes | 7 |
| Rockson et al.[27] | No | Yes | Yes | Yes | Yes | 7 |
| Hemmati et al.[16] | Yes | Yes | Yes | Yes | Yes | 8 |
| Tatar and Turhan[22] | No | Yes | Yes | Yes | Yes | 7 |
| Selcuk Yilmaz and Ayhan[28] | No | Yes | Yes | Yes | Yes | 7 |
| El-Shazly et al.[6] | No | Yes | Yes | Yes | Yes | 6 |
| Mahran and Thabet[24] | No | Yes | Yes | Yes | Yes | 6 |
| Studies | NHMRC Level | 1 | 2 | 3 | 4a | 4b | 5a | 5b | 6a | 6b | 6c | 7a | 7b | 7c | 7d | 8 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gnanasekar[34] | IV | Y | Y | Single case design | Y | NA | Y | Y | Y | NA | NA | N | N | N | NA | Y | 7/10 | 70% |
| Bhatikar[47] | IV | Y | Y | Single case design | Y | NA | Y | Y | Y | NA | NA | N | N | N | NA | Y | 7/10 | 70% |
| Özçete and Eyigör[25] | IV | Y | Y | Single case design | Y | NA | Y | Y | Y | NA | NA | N | N | N | NA | Y | 7/10 | 70% |
| Joos et al.[34] | III-3 | Y | Y | Before and after | Y | N | Y | Y | Y | NA | NA | Y | Y | Y | Y | Y | 11/12 | 91.6% |
| Pattanshetty et al.[38] | IV | Y | Y | Single case design | Y | NA | Y | Y | Y | NA | NA | N | N | N | NA | Y | 7/10 | 70% |
| Bae and Kim[23] | III-3 | Y | Y | Before and after | Y | N | Y | Y | Y | NA | NA | Y | Y | Y | N | Y | 9/12 | 75% |
Modified McMaster items to be scored: (1) Was the purpose of the study clearly stated? (2) Was relevant background literature reviewed? (3) Study design (4a) Was the sample described in detail? (4b) Was sample size justified? (5a) Were the outcome measures reliable? (5b) Were the outcome measures valid? (6a) Intervention was described in detail? (6b) Contamination was avoided? (6c) Co-intervention was avoided? (7a) Results were reported in terms of statistical significance? (7b) Were the analysis method/s appropriate? (7c) Clinical importance was reported? (7d) Drop-outs were reported? (8) Conclusions were appropriate given study methods and results? NHMRC: National Health and Medical Research Council, Y: Yes, N: No, NA: Not-applicable
Participants
A total of 815 participants were included, with sample sizes ranging from 1 to 76. All participants were aged 18 and above and had various stages of lymphedema (Stage I-III) caused by breast cancer related treatment.
Intervention
About 11 different types of electro-therapeutic modalities, that is ESWT, MRT, TENS, therapeutic ultrasound, faradic current, LLLT, photo-biomodulation therapy (PBMT), Helium neon laser therapy, IPCT, advanced pneumatic compression device (APCD) and non-pneumatic compression device (NPCD) were used. The effect of ESWT, LLLT, IPCT, MRT, therapeutic ultrasound, faradic current and TENS was investigated by 7, 7, 6, 3, 1, 1 and 1 studies, respectively. A RCT by Abdelhalim and Samhan[14] compared ESWT and IPCT, whereas one randomised crossover trial by Rockson and Skoracki[15] investigated the effect of APCD Versus NPCD. The impact of therapeutic ultrasound in comparison to faradic current was also assessed in a study by Hemmati et al.[16] The parameters of all interventions and its results are mentioned in Tables 5 and 6, respectively.
| Studies | Electrotherapeutic modalities | Evaluated Groups | Frequency | Duration | Co- intervention | Outcomes evaluation |
|---|---|---|---|---|---|---|
| Aykac Cebicci and Dizdar[17] | ESWT | CDT and ESWT | 12 sessions, 3 times a week, frequency of 4 Hz at 2 bar, 15 mm head, 2500 shocks | 4 weeks | CDT | Baseline, post-treatment and 1st month after treatment |
| Ridner et al.[29] | LLLT | MLD, LLLT and MLD+LLLT | 20 min, 20–30 s per point in each grid | - | MLD | Pre-treatment, daily, weekly and end of treatment |
| Abdelhalim and Samhan[14] | ESWT and IPCT | ESWT and IPCT | ESWT: 3 times/week, 12 sessions. 2500 shocks IPTC: 45 min, 5 times/week, 20 sessions, 60 mm Hg cuff pressure | 4 weeks | Home exercises | Baseline and post-treatment |
| Kilmartin et al.[33] | LLLT | Laser and Control | Twice a week, 1 min at 10 sites, 8–16 sessions, dose: 1.5 J/cm2(total: 15 J/cm2 per session) |
4 weeks | CDT | 1st visit, 8th session, post-treatment, at 3rd, 6th and 12th month |
| Diab et al.[37] | IPCT | IPTC+KT and Control | 3 times a week for 4 weeks, 60 mm Hg, 30 min | 4 weeks | CDT, KT | Pre and post-treatment |
| Rockson and Skoracki[15] | APCD and NPCD | APCD and NPCD | 1 h per day for 28 days- washout period of 4 weeks-another treatment of 28 days | 12 weeks | - | Day 0 and 28 of each period |
| T.V. Gnanasekar[34] | MRT | - | 10 sessions, alternate days, 60–75 min inclusive of CDT | 3 weeks | CDT | Pre and post treatment |
| Lee et al.[18] | ESWT | ESWT and Control | Twice a week, 6 sessions, 0.056–0.068 mJ/mm2, 2500 shocks | 3 weeks | CDT | Before treatment and 3 weeks after treatment |
| Uzkeser et al.[35] | IPCT | CDT and CDT+IPCT | 40 mmHg for 45 min, 5 times a week | 3 weeks | CDT | Baseline, after therapy (week 3) and 1 month after completion (week 7) |
| Bhatikar[47] | MRT | - | Low intensity | - | Joint mobilisation and Exercises | 1st, 2nd, 3rd, 4th, 5th and 6th month |
| Khalaf et al.[30] | HNLT | HNLT and Control | 5000 Hz, 15 min, 50 ns pulse duration, 5 mW power intensity, 632.8 nm wave length and 1.5 J/cm2, 17 points (1 min each), 3 times/week |
6 months | Decongestive lymphatic therapy | Before treatment and end of study after 6 months |
| Pajero Otero et al.[36] | IPTC | CPT+IPCT and KT | 30 min, 40 mm Hg, 5 days/week for 3 weeks with washout period of 6 months | 3 weeks | KT and MLD | Pre and post treatment |
| Chmielewska et al.[39] | IPTC | IPCT+Ex and IPCT | 20 sessions (5 times a week), 60 mm Hg cuff pressure for 45 min | 4 weeks | Exercises | Before and after treatment |
| Uzkeser et al.[19] | PCT | PCT and Control | 5 times a week, total 15 sessions | 3 weeks | MLD, Compression bandages and exercise | Baseline, after therapy and 1 month after completion |
| Farhan et al.[20] | Low level light laser | LLLT | 3 times a week, radiation dose of 2 J/cm2, output of 100 mWarr, wavelength of 658 nm | 4 weeks | - | Week 0, end of week 4, start of week 12 and end of week 16 |
| Özçete and Eyigör[25] | Low level light laser | - | 3 sessions/week (total 12), 15 min, 5000 Hz, 0.8J/cm2 at 3 points | 4 weeks | KT | Pre, post and 3 months after treatment |
| Lee et al.[21] | ESWT | ESWT and Control | Thrice a week, 9 sessions, 0.056–0.068 mJ/mm2, 4 Hz, 2500 shocks | 3 weeks | CDT | Baseline, 3 weeks after ESWT completion and 3 months post-ESWT completion |
| Joos et al.[32] | ESWT | ESWT | Twice a week, 0.10 mJ/mm2, 4Hz, membrane pressure level 6 or 7, penetration depth of 8 cm, large focus of 10–15 mm, total energy 5880 Mj | 4 weeks | MLD | Baseline, after every 2 sessions, 4 weeks and 3 months post treatment |
| Pattanshetty et al.[38] | MRT | - | 5 sessions | 10 days | Cupping and MLD | Pre and post treatment |
| Storz et al.[31] | PBMT | Laser and Placebo | 8 sessions (twice a week), 980 nm, 40 mW average power output, 10 min, point of 4.9 cm2–24 J, 384 J over whole axilla, energy density 4.89 J/cm2, power density 8.14 mW/cm2 |
4 weeks | - | Pre and post treatment, follow-up at 4, 8 and 12 weeks |
| Tastaban et al.[26] | IPCT | CDT and CDT+IPCT | 30 min, 30–40 mm of Hg pressure, 5 days/week | 4 weeks | CDT | Pre and post treatment |
| Rockson et al.[27] | APCD and NPCD | APCD and NPCD | Once daily for 60 min for 28 days with washout period of 4 weeks | 12 weeks | - | Pre-treatment and post-treatment (28 days) |
| Hemmati et al.[16] | UST and FC | CDT, CDT+UST and CDT+FC | 5 sessions per week (10 sessions), UST: 1 MHz, 2 W/cm2 pulsed and Faradic under pressure: 30 Hz, 300 µs, interval of 2 s and off time of 5s | 2 weeks | CDT | Before and at end of 10 sessions |
| Tatar and Turhan[22] | TENS | IDT and Control | 5 days a week, 20 min of heat and ex, TENS: 20 min of conventional TENS | 3 weeks | Exercises, Hot pack and TENS | Before and after 3 weeks of program |
| Selcuk Yilmaz and Ayhan[28] | LLLT | MLD, KT and LLLT | 5 days a week, power density of 30 mW/cm2 and a square centimeter density of 1.5 J/cm2 for 1 min, 20 min, 12 points on axillary region and 8 points in cubital or elbow area | 3 weeks | MLD and KT | Baseline, end of treatment, 4-and 12-weeks post treatment |
| Bae and Kim[23] | ESWT | ESWT and ESWT+MLD+IPCT | Twice a week, 0.056–0.068 mJ/mm2, 2000 shocks (1000 for most fibrotic and 1000 for less fibrotic) | 2 weeks | MLD and PCT | Before treatment and after 4 sessions of ESWT |
| El-Shazly et al.[6] | ESWT | ESWT and Control | 2 times/week, 2000 impulses for 10 min, 1000 on most fibrotic point and 1000 on lesser fibrotic point, 0.040–0.069 mJ/mm2 energ flux density and frequency 5 Hz | 6 weeks | Traditional PT | Pre-treatment and post-treatment |
| Mahran and Thabet[24] | ESWT | ESWT and Control | Twice a week, 2500 shocks, pressure of 2 bar and frequency 4 Hz | 8 weeks | Traditional PT | Before treatment, 4 weeks and 8 weeks after treatment |
ESWT: Extracorporeal shock wave therapy, MLD: Manual lymphatic drainage, KT: Kinesio-taping, IPCT: Intermittent pneumatic compression therapy, TENS: Transcutaneous electrical nerve stimulation, CDT: Complex decongestive therapy, PBMT: Photo-biomodulation therapy, CPT: Complex physical therapy, APCD: Advanced pneumatic compression device, NPCD: Non-pneumatic compression device, KT: Kinesiotherapy, LLLT: Low level laser therapy, PT: Physiotherapy
| Studies | Intervention | Circumference | Volume | Pain | LYM-QOL Arm | FACT-B |
|---|---|---|---|---|---|---|
| Aykac Cebicci and Dizdar[17] | ESWT | *↑ | *↑ | |||
| Ridner et al.[29] | LLLT | *↑ | *↑ | |||
| Abdelhalim and Samhan[14] | ESWT and IPCT | *↑ | ||||
| Kilmartin et al.[33] | LLLT | *↑ | ||||
| Diab et al.[37] | IPCT | *↑ | ||||
| Rockson and Skoracki[15] | APCD and NPCD | *↑ | *↑ (NPCD) and ↔ (APCD) | |||
| Gnanasekar[34] | MRT | ?↑ | ?↑ | ?↑ | ||
| Lee et al.[18] | ESWT | *↑ | *↑ | *↑ | ||
| Uzkeser et al.[35] | IPCT | *↑ | *↑ | *↑ | ||
| Bhatikar[47] | MRT | ?↑ | ?↑ | |||
| Khalaf et al.[30] | HNLT | *↑ | ||||
| Pajero Otero et al.[36] | IPTC | *↑ (RVC), ↑? (RVD) | ||||
| Chmielewska et al.[39] | IPTC | *↑ | ||||
| Uzkeser et al.[19] | PCT | *↑ | *↑ | |||
| Farhan et al.[20] | LLLT | *↑ | *↑ | *↑ | ||
| Özçete and Eyigör[25] | LLLT | ?↑ | ?↑ | |||
| Lee et al.[21] | ESWT | *↑ | *↑ | |||
| Joos et al.[32] | ESWT | *↑ | ?↑ | |||
| Pattanshetty et al.[38] | MRT | ?↑ | ?↑ | ?↑ | ||
| Storz et al.[31] | PBMT | ?↑ | ||||
| Tastaban et al.[26] | IPCT | ?↑ | ?↑ | |||
| Rockson et al.[27] | APCD and NPCD | *↑ | *↑ | |||
| Hemmati et al.[16] | UST and FC | *↑ | *↑ | *↑ | ||
| Tatar and Turhan[22] | TENS | *↑ | ↔ | *↑ | ||
| Selcuk Yilmaz and Ayhan[28] | LLLT | *↑ | *↑ | |||
| Bae and Kim[23] | ESWT | *↑ | *↑ | |||
| El-Shazly et al.[6] | ESWT | *↑ | ||||
| Mahran and Thabet[24] | ESWT | *↑ | *↑ | |||
| Studies | Intervention | ROM | DASH | Quick DASH | SPADI | Skin Thickness |
| Aykac Cebicci and Dizdar[17] | ESWT | *↑ | ||||
| Ridner et al.[29] | LLLT | |||||
| Abdelhalim and Samhan[14] | ESWT and IPCT | *↑ | *↑ | |||
| Kilmartin et al.[33] | LLLT | |||||
| Diab et al.[37] | IPCT | *↑ | ||||
| Rockson and Skoracki[15] | APCD and NPCD | |||||
| Gnanasekar[34] | MRT | ?↑ | ||||
| Lee et al.[18] | ESWT | *↑ | *↑ | |||
| Uzkeser et al.[35] | IPCT | *↑ | ||||
| Bhatikar[47] | MRT | |||||
| Khalaf et al.[30] | HNLT | *↑ | ||||
| Pajero Otero et al.[36] | IPTC | *↑ | *↑ | |||
| Chmielewska et al.[39] | IPTC | |||||
| Uzkeser et al.[19] | PCT | *↑ | ||||
| Farhan et al.[20] | LLLT | |||||
| Özçete and Eyigör[25] | LLLT | |||||
| Lee et al.[21] | ESWT | *↑ | *↑ | |||
| Joos et al.[32] | ESWT | |||||
| Pattanshetty et al.[38] | MRT | ?↑ | ?↑ | |||
| Storz et al.[31] | PBMT | ?↑ | ||||
| Tastaban et al.[26] | IPCT | ?↑ | ?↑ | |||
| Rockson et al.[27] | APCD and NPCD | |||||
| Hemmati et al.[16] | UST and FC | *↑ | ||||
| Tatar and Turhan[22] | TENS | ↔ (Flex, Ext, Abd) *↑ (Rot) | *↑ | |||
| Selcuk Yilmaz and Ayhan[28] | LLLT | *↑ | *↑ | |||
| Bae and Kim[23] | ESWT | *↑ | ||||
| El-Shazly et al.[6] | ESWT | *↑ | ||||
| Mahran and Thabet[24] | ESWT | *↑ |
LYM-QOL: Lymphedema quality of life, RVC: Relative volume change, RVD: Relative volume difference, ESWT: Extracorporeal shock wave therapy, ROM: Range of motion, DASH: Disabilities of the arm, shoulder and hand, Q-DASH: Quick DASH, SPADI: Shoulder pain and disability index, GS-D: Grip strength measured by dynamometer, IPCT: Intermittent pneumatic compression therapy, TENS: Transcutaneous electrical nerve stimulation, MRT: Matrix rhythm therapy, FACT-B: Functional assessment of cancer therapy-breast, PBMT: Photo-biomodulation therapy. *: Statistical significance, ?: Statistical significance not reported, ↑: Increased, ↑ : Decreased, ↔:No change
Outcome measures
Arm volume was the primary outcome measure in 22 studies, making it the most frequently used outcome. Volume displacement method by Archimedes’ principle was used by nine studies[16-24], and other methods included were the truncal cone formula,[25-28] classical disc method,[29-31] infrared perometry,[32,33] and limb volume program.[34] Two studies used volume difference[15,35] and one study[36] evaluated relative volume change (RVC) and relative volume difference.
Arm circumference was the second common outcome measure used in 18 studies. Sixteen studies evaluated the circumference of the affected arm, whereas two studies conducted by Abdelhalim and Samhan[14] and Uzkeser et al.[35] measured the variation in circumference between the affected and healthy arms.
Another outcome measure was shoulder ROM, assessed in nine studies by goniometer[6,24,28-30,34,36-38] and in one study[22] by isokinetic dynamometer. Pain was evaluated in eight studies by Visual Analogue Scale (VAS), one study by Verbal Rating Scale[34] and another study by numeric pain rating scale.[16] Shoulder pain and disability were assessed by DASH,[16,22,36] Q-DASH[17,18,21,26,28] and SPADI.[38] QOL was evaluated by LYM-QOL[15,27,28] and FACT-B.[29,38] Fewer articles stated other outcomes such as skin thickness, grip strength, depression and sensory impairments. They are summarised in Table 7.
| Studies | Circumference | Volume | Skin thickness | Pain | DASH | Q-DASH | SPADI | ROM | LYM-QOL | GS-D | FACT-B |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aykac Cebicci and Dizdar[17] | + | + | + | ||||||||
| Ridner et al.[29] | + | + | + | ||||||||
| Abdelhalim and Samhan[14] | + | + | + | ||||||||
| Kilmartin et al.[33] | + | ||||||||||
| Diab et al.[37] | + | + | |||||||||
| Rockson and Skoracki[15] | + | + | |||||||||
| Gnanasekar[34] | + | + | + | + | |||||||
| Lee et al.[18] | + | + | + | + | + | ||||||
| Uzkeser et al.[35] | + | + | + | + | |||||||
| Bhatikar[47] | + | + | |||||||||
| Khalaf et al.[30] | + | + | |||||||||
| Pajero Otero et al.[36] | + | + | + | ||||||||
| Chmielewska et al.[39] | + | ||||||||||
| Uzkeser et al.[19] | + | + | + | ||||||||
| Farhan et al.[20] | + | + | + | ||||||||
| Özçete and Eyigör[25] | + | + | |||||||||
| Lee et al.[21] | + | + | + | + | |||||||
| Joos et al.[32] | + | + | |||||||||
| Pattanshetty et al.[38] | + | + | + | + | + | ||||||
| Storz et al.[31] | + | + | |||||||||
| Tastaban et al.[26] | + | + | + | + | |||||||
| Rockson et al.[27] | + | + | |||||||||
| Hemmati et al.[16] | + | + | + | + | |||||||
| Tatar and Turhan[22] | + | + | + | + | + | ||||||
| Selcuk Yilmaz and Ayhan[28] | + | + | + | + | |||||||
| Bae and Kim[23] | + | + | + | ||||||||
| El-Shazly et al.[6] | + | + | |||||||||
| Mahran and Thabet[24] | + | + | + |
DASH: Disabilities of the arm, shoulder and hand, Q-DASH: Quick DASH, SPADI: Shoulder pain and disability index, ROM: Range of motion, LYM-QOL: Lymphedema quality of life questionnaire, GS-D: Grip strength measured by dynamometer, FACT-B: Functional assessment of cancer therapy-breast, ‘+’: Outcome measures assessed
Heterogeneity of results
To address potential heterogeneity in the meta-analysis, several steps were taken to ensure the results were valid and reliable. First, after data extraction, statistical heterogeneity was assessed to determine whether performing a meta-analysis was appropriate. The software Stata version 16 was used for this analysis. Only the studies that provided the necessary data for arm circumference, volume and ROM were included in the quantitative evaluation, ensuring a consistent basis for comparison across studies. To further manage heterogeneity, the results were homogenised by conducting subgroup analyses. These subgroups included arm circumference measured at four different levels (wrist, forearm, elbow and arm) and ROM assessed for three specific movements (flexion, abduction and external rotation). This approach allowed for a more detailed and precise comparison of the outcomes, minimising the potential for variability due to different measurement techniques. For statistical analysis, continuous data were expressed as mean ± standard deviation. To assess statistical heterogeneity, Cochran’s Chi-squared test (Q test) and I-squared test were used. A random effects model was applied when the I-squared value was >50% and the P-value was <0.01, indicating substantial heterogeneity. In addition, Cohen’s d effect size was used as an estimator to assess the variations within and between studies. To summarise the findings, a forest plot was created, which visually represented the pooled results from the meta-analysis. Finally, a funnel plot was analysed to check for publication bias and other potential biases, ensuring the robustness and transparency of the findings. These steps collectively addressed potential heterogeneity and ensured a comprehensive and reliable analysis of the data.
Primary outcome: Arm volume
All the studies that assessed arm volume showed improvements except one RCT by Tatar and Turhan, 2022[22] where TENS was given as a conventional treatment and compared to intensive complex decongestive therapy (CDT). No significant difference was observed in the control group (P = 0.655), while a significant improvement was noted in the intervention group (P = 0.001).
For meta-analysis, five trials with 218 participants (109 in each control and intervention group) were included in the meta-analysis. The volume was measured by Archimedes’ principle and the classical disc method. The negative Cohen’s d value indicates that all studies, except Tatar and Turhan, 2022[22] observed a substantial decrease in volume after intervention. However, the combined effect size is not statistically significant at the conventional threshold of 0.05, as the P-value for the test of theta is 0.0993. There is significant heterogeneity among the studies as I2 is high (91.49%) and as per the test of homogeneity, the P-value is 0.0000, as shown in Figures 2 and 3.
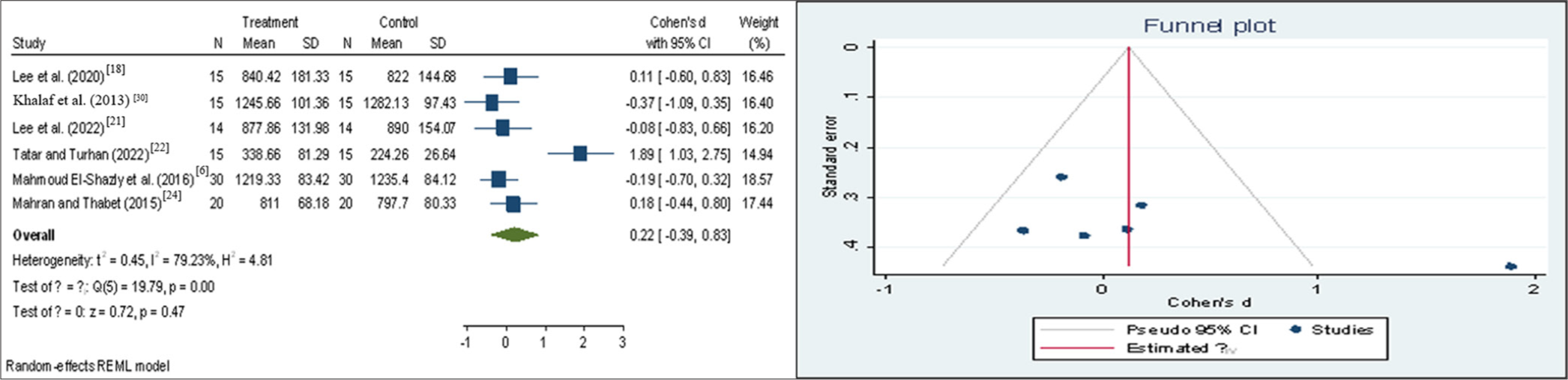
- Forest plot and funnel plot representing volume (pre-test). CI: Confidence interval, SD: Standard deviation

- Forest plot and funnel plot representing volume (post-test). CI: Confidence interval, SD: Standard deviation
Primary outcome: Arm circumference
There was a significant improvement in arm circumference in most of the studies. Five studies with 139 participants (70 intervention group and 69 control group) were included for the meta-analysis and were done on four different levels: Wrist, below elbow, elbow and above elbow.
At wrist level
All studies observed significant improvement in arm circumference at wrist level as suggested by a negative Cohen’s d value. The combined effect is statistically significant as P-value is <0.05 (z = −3.17, Prob > z = 0.0015) and there is no evidence of significant heterogeneity (Low I2 [22.06%] and Q = chi2 [4] =4.99, Prob > Q = 0.2878). Considering individual studies, Lee et al. (2022)[21] lies on the line of null effect, suggesting no difference between the two groups. Diab et al. (2021),[37] Chmielewska et al. (2016)[39] and Tatar and Turhan (2022)[22] have shown large effect size of −0.85, −0.82 and −1.11, respectively. Lee et al. (2020)[18] has shown medium effect size of −0.46 showing a relatively smaller difference between the groups. The funnel plot suggests absence of publication bias, as shown in Figures 4 and 5.

- Forest plot and funnel plot representing circumference-wrist (pre-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood.

- Forest plot and funnel plot representing circumference-wrist (post-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood.
Below elbow
The combined effect size was not considerable (z = −1.10, Prob > z = 0.2693), and there was evidence of significant heterogeneity (Low I2 (69.66%) and Q = chi2 [4] = 12.56, Prob > Q = 0.0136) among the studies, as shown in Figures 6 and 7. However, on individual analysis, Diab et al. (2021),[37] Lee et al. (2022)[21] and Tatar and Turhan (2022)[22] have demonstrated large effect sizes of −0.87, −0.84 and −0.81, respectively, suggesting significant improvement. Lee et al. (2020)[18] and Chmielewska et al. (2016)[39] lie on the other half of forest plot, suggesting no significant reduction in arm circumference.

- Forest plot and funnel plot representing circumference-below elbow (pre-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood.
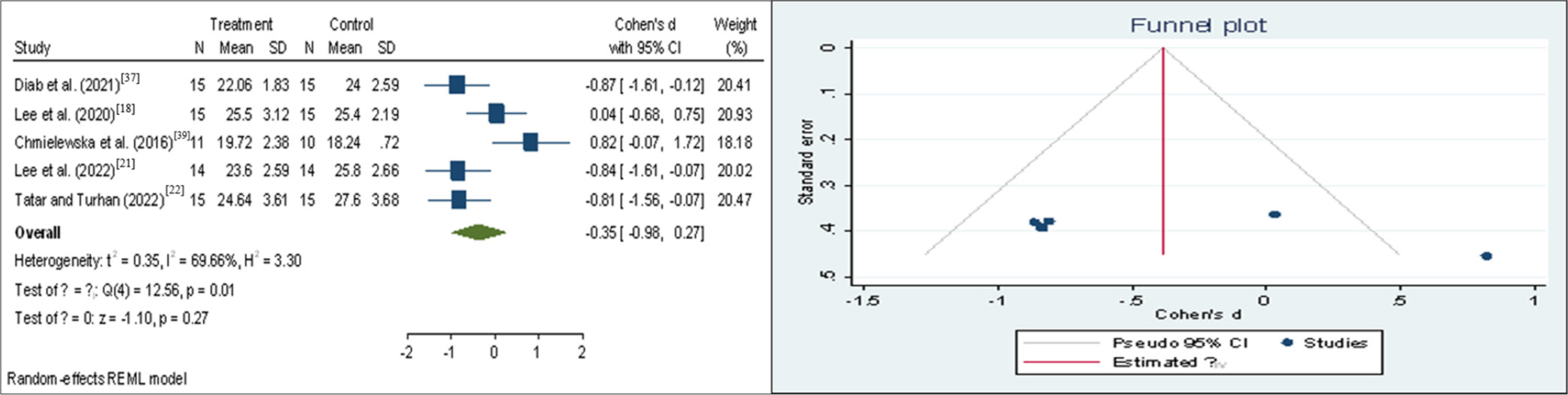
- Forest plot and funnel plot representing circumference-below elbow (post-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
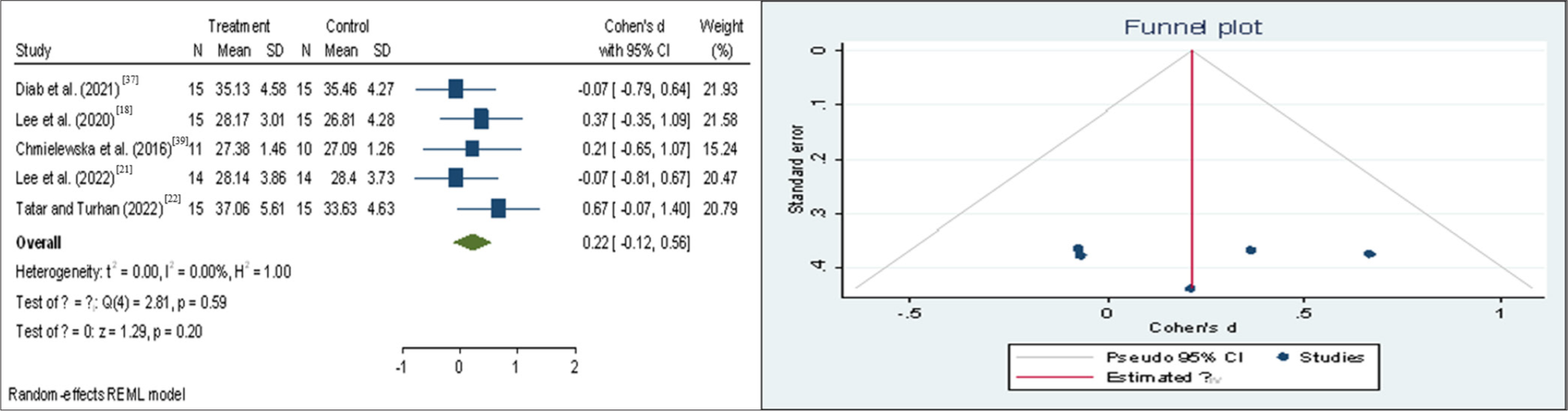
At elbow
The combined effect size was not statistically significant (z = −0.20, Prob > z = 0.8431) and there was no strong evidence of significant heterogeneity (Low I2 (56.23%) and Q = chi2 [4] = 9.14, Prob > Q = 0.0578) among the studies, as shown in Figures 8 and 9. Only one study, that is Diab et al. (2021)[37] has shown a significant reduction in arm circumference. Other studies lie very close to the line of null effect, demonstrating no significant or very less improvement.

- Forest plot and funnel plot representing circumference-elbow (pre-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood

- Forest plot and funnel plot representing circumference-elbow (post-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
Below axilla
The combined effect size was not statistically significant (z = −0.20, Prob > z = 0.8414) and there was evidence of significant heterogeneity (Low I2 [59.00%] and Q = chi2 [4] = 9.70, Prob > Q = 0.05) among the studies, as shown in Figures 10 and 11. Diab et al. (2021)[37] have shown large effect size of -0.99 whereas Lee et al. (2022)[21] have shown small effect size of −0.23. Other studies lie on the other half of forest plot suggesting no significant improvement in the intervention group.
- Forest plot and funnel plot representing circumference-below axilla (pre-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
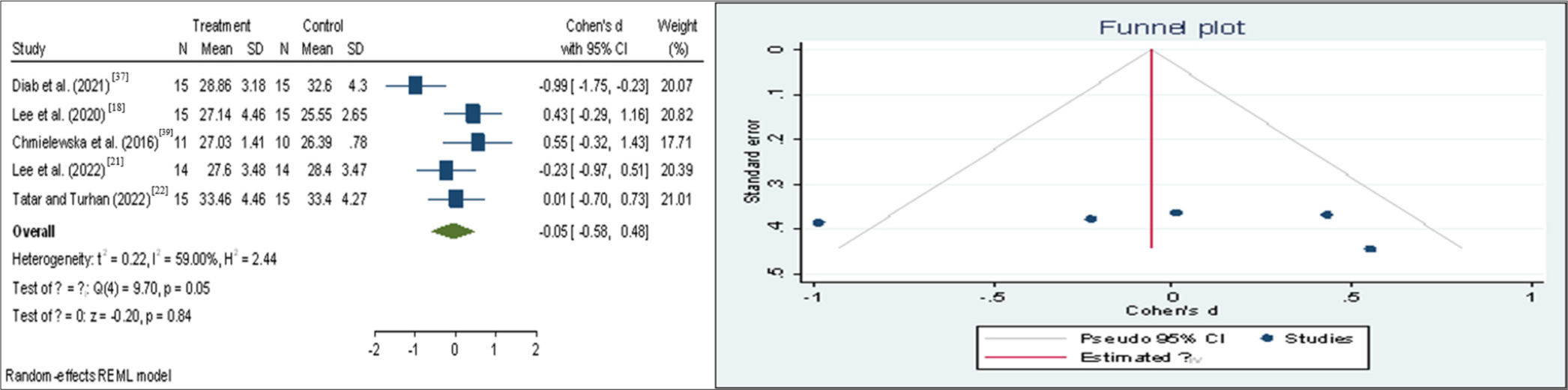
- Forest plot and funnel plot representing circumference-below axilla (post-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
Primary outcome: Shoulder ROM
Four studies with 160 participants (80 in both intervention and control group) were analysed. There was significant improvement in all the studies and all three movements, that is external rotation, flexion and abduction were analysed.
Flexion
The combined effect size was statistically significant (z = 0.05, Prob > z = 0.0000) and there was some evidence of significant heterogeneity (I2 = 28.82% and Q = chi2 [3] = 4.06, Prob > Q = 0.2555) among the studies, as shown in Figures 12 and 13. All studies have shown significant improvement in flexion ROM with a large effect size (0.64–1.59).

- Forest plot and funnel plot representing range of motion-Flexion (Pre-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood

- Forest plot and funnel plot representing range of motion-flexion (post-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
Abduction
Similarly, for abduction movement, the combined effect size was statistically significant (z = 6.61, Prob > z = 0.0000) and there was some evidence of significant heterogeneity (I2 = 0.00% and Q = chi2 [3] = 0.88, Prob > Q = 0.8301) among the studies, as shown in Figures 14 and 15. All studies have shown significant improvement with large effect size ranging from 0.96 to 1.45.

- Forest plot and funnel plot representing range of motion-abduction (Pre-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood

- Forest plot and funnel plot representing range of motion-abduction (post-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
External rotation
The same findings were observed for external rotation movement. The combined effect size was statistically significant (z = 7.61, Prob>z = 0.0000) and there was some evidence of significant heterogeneity (I2 = 0.00% and Q = chi2 [3] = 2.15, Prob > Q = 0.54) among the studies, as shown in Figures 16 and 17. All the studies have shown large effect sizes ranging from 095 to 1.60, suggesting significant improvement in abduction range.

- Forest plot and funnel plot representing range of motion-external rotation (pre-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
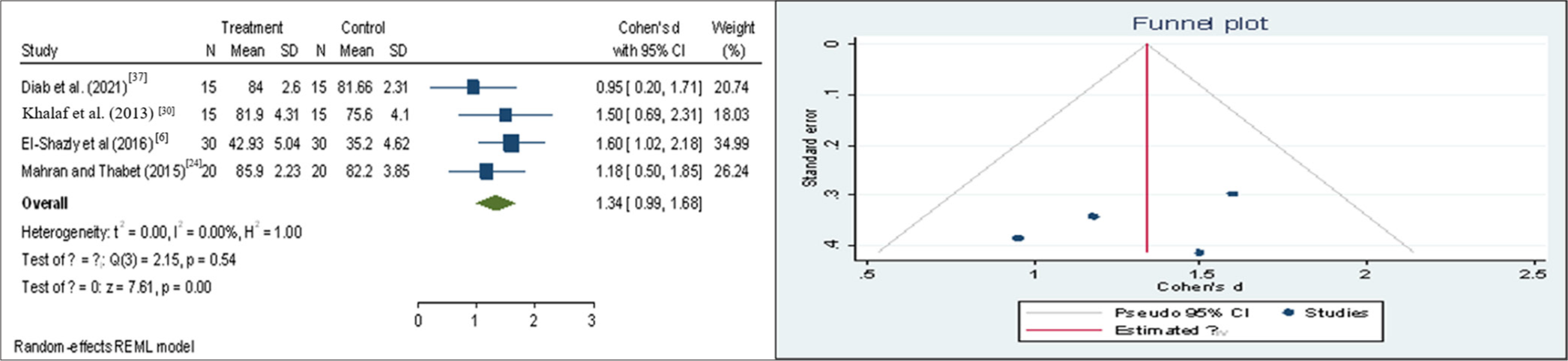
- Forest plot and funnel plot representing range of motion-external rotation (post-test). CI: Confidence interval, SD: Standard deviation, REML: Restricted maximal likelihood
Secondary outcome: QOL
Regarding QOL, three studies used LYM-QOL and two studies used FACT-B. There was significant improvement in all the studies. However, there were insufficient data to conduct a meta-analysis.
Secondary outcomes: Shoulder pain and disability
DASH, Q-DASH and SPADI were used to assess shoulder pain and disability by ten studies and they demonstrated significant improvement in the scores.
Adverse events
None of the studies identified any significant adverse consequences. Two studies conducted by Pajero Otero et al.[36] and Selcuk Yilmaz and Ayhan[28] reported itching, paraesthesia, reddening, skin peeling and allergy, as both included Kinesio-taping (KT) as a co-intervention. Another study done by Farhan et al.[20] reported nausea and feeling of weakness among two participants.
DISCUSSION
Breast cancer is considered a major problem due to its high incidence and impact on QOL.[4] BCRL and shoulder dysfunction is a life-long complication affecting physical, mental and emotional function among the survivors. CDT is regarded as the treatment for BCRL.[33] Along with CDT, other conventional physiotherapy treatments such as manual lymphatic drainage (MLD), circulatory exercises, elevation and compression bandaging are advised. There are numerous electro-therapeutic modalities that are proven to be reliable and beneficial in the treatment of BCRL.[7-9] The aim of this study was to offer a comprehensive review of these electro-therapeutic modalities and evaluate the evidence supporting their effectiveness.
The qualitative analysis revealed that the included studies provide good quality evidence on role of electro-therapeutic modalities on BCRL and shoulder dysfunction. About 11 different types of electro-therapeutic modalities, that is ESWT, LLLT, IPCT, MRT, helium neon laser therapy, PBMT and TENS were being used.
ESWT was the most often utilised modality. It is a noninvasive, safe, cost-effective and emerging treatment, widely applied in orthopaedic conditions such as elbow epicondylitis, plantar fasciitis and calcifying tendinitis of the shoulder.[40] ESWT has shown to increase stem cell activity, promote endothelial neo angiogenesis, prevent soft-tissue fibrosis and ultimately help in tissue regeneration.[41] A study done in animals has proved that ESWT alleviates lymphedema by enhancing the release of vascular endothelial growth factor (VEGF) and encouraging lymph angiogenesis.[42] Pilot studies performed by Bae and Kim, 2013[23] and Joos et al., 2021[32] found significant improvement in arm circumference, volume and skin elasticity. Study done by Mahran and Thabet, 2015[24] on postmenopausal patients stated that ESWT speed up reduction of BCRL as well as improve shoulder ROM. Similar findings was found by Lee et al. (2022)[21] and Lee et al. (2020).[18] Aykac Cebicci and Dizdar (2021) administered ESWT over 12 sessions, 3 times a week, using a 15 mm head to deliver 2500 shocks at a frequency of 4 Hz and a pressure of 2 bar. Within group assessment revealed significant improvement in the outcomes whereas when compared with another group receiving CDT, there was no statistically significant difference suggesting ESWT which can be an alternative treatment to CDT.[17] Abdelhalim and Samhan (2018) compared shockwave versus pneumatic compression and found that ESWT had greater improvement in terms of circumference and skin thickness than IPCT.[14]
Photobiomodulation therapy (PBMT), also known as low-level light laser therapy, was the second most frequently used electro-therapeutic modality. The North American Association for Laser Therapy defines PBMT as the ‘therapeutic use of light absorbed by endogenous chromophores, initiating non-thermal, non-cytotoxic biological reactions through photochemical or photophysical processes, resulting in physiological changes’. It aids in pain and inflammation relief, immunomodulation and supports wound healing and tissue regeneration.[43] In case of BCRL, laser stimulates macrophage cells and lymph angiogenesis leading to stimulation of immune system and lymphatic drainage. A case-report presented on a 57-year-old female patient with BCRL and arteriovenous (AV) fistula for haemodialysis underwent 12 sessions of LLLT along with KT and remedial exercises as CDT was contraindicated due to AV fistula. There was significant decrease in arm volume (691 mL–454 mL) and was concluded that LLLT and KT can be used as an alternative for CDT.[25] Multiple placebo-controlled studies found significant improvement by active laser in terms of pain (50%), QOL and mean grip strength,[31] limb volume and shoulder mobility[30] as well as symptom distress of sadness (73 to 11%) and self-perception (36 to 0%).[33] However, a RCT by Selcuk and Ayhan, 2023 compared the effect of low-level light laser (LLLT), KT and MLD and it was found that the percentage of decreased arm volume or treatment success was better in KT group.[28] Similarly, another RCT by Ridner et al. examined the impact of MLD, LLLT and combined MLD plus LLLT in terms of limb volume, extracellular fluid, QOL, psychological and physical symptoms. Clinically and statistically substantial improvements were shown by all therapy groups; however, no notable differences were seen between them.[44]
MRT is an advancement in physiotherapy that works on the principle of cellular oscillations with a frequency of 8–12 Hz.[45] It activates and rebalances the normal physiological vibrations of skeletal muscles and nervous system.[46] This rhythm produces anti-oedematous effects by maximising lymphatic venous perfusion of extracellular space. MRT, being a novel treatment, only three case-reports were found during qualitative analysis. Pattanshetty et al. reported a case of 54-year-old female with BCRL, treated by multimodal approach with MaRhyThe©, sliding cupping and routine physiotherapy.[38] MaRhyThe© was administered over complete upper limb, pectorals, trapezius, rhomboids and paraspinal muscles followed by cupping for 15–20 min and was beneficial in reducing lymphedema, pain and improving shoulder ROM. Similarly, Gnanasekar, 2020 presented a case of 50-year-old female treated with MRT, along with CDT.[34] The treatment was given for 60–75 min across ten sessions over a 3-week period, resulting in significant improvements in ROM, pain, limb volume and QOL. Another case report by Bhatikar, 2018 examined a novel protocol with MRT, compression garments, free hand exercises, resisted exercises with TheraBand/FlexBar and mobilisation on a 62-year-old female with BCRL and shoulder stiffness.[47] MRT was administered in limb elevation, with low intensity in lymphatic drainage position followed by effleurage. It showed significant improvement in terms of lymphedema, pain, ROM as well as muscle strength.
Intermittent pneumatic compression (IPC) is a non-invasive technique widely used in the management of lymphedema. It features a multi-chambered design with sequential inflation, gradient pressure and adjustable time settings. The applied pressure aids in moving the oedema proximally toward the limb’s root and the adjacent trunk. Diab et al.[37] investigated the combined effects of IPC and KT on patients with BCRL, administering IPC for 30 min, 3 times a week over 4 weeks, at a pressure of 60 mmHg. The study found a significant reduction in lymphedema size and a notable improvement in shoulder ROM in the treatment group compared to the control group. In addition, a randomised crossover clinical trial involving 43 women compared the effectiveness of complex physical therapy (CPT) and IPC with that of KT.[36] RVC and shoulder ROM was better on IPC group whereas DASH score and pain was better on KT group. Similar evidence was found by Chmielewska et al.[39] supporting the use of pneumatic compression to reduce BCRL. In contrast, a RCT done by Tastaban et al.[26] found that IPC added no benefits when combined with CDT and appeared to be useful only to reduce sensation of heaviness and tightness. Similar results were observed by Uzkeser and Karatay,[19] who found no significant difference between the IPC group and the control group regarding upper limb ROM, VAS and the Constant–Murley scale.
Fewer studies had used TENS, therapeutic ultrasound and faradic current for the treatment if BCRL. Hemmati et al.[16] conducted a randomised clinical trial on 39 patients with BCRL and was randomly allocated to three groups: Control group (CDT), ultrasound group (Ultrasound and CDT) and faradic group (Faradic current and CDT). There was greater reduction in lymphedema volume, pain and functional disability when electrotherapy modalities were combined with CDT. However, no significant improvement was noted in limb circumference. Another RCT by Tatar and Turhan[22] aimed to assess the effect of CDT on upper extremity function, with TENS administered to both the control and intervention groups. Conventional TENS was applied for 20 min to the shoulder joint and surrounding painful areas. Both groups showed significant enhancements in shoulder ROM as well as upper limb functionality, but changes in circumference and volumetric measurements were only observed in the CDT group.
Strength of study
This review is, to our knowledge, the first to evaluate the effectiveness of electro-therapeutic modalities in managing BCRL and shoulder dysfunction. This review included 815 participants across 28 studies which add significantly to the existing evidence and many included studies were of low risk of bias and provided good quality evidence. Studies other than RCTs such as case reports and prospective clinical trials were also included considering novel electro-therapeutic modalities such as MRT and ESWT. Additional strengths of this review include compliance with PRISMA guidelines, the incorporation of a risk of bias assessment and the execution of a meta-analysis that demonstrated low statistical heterogeneity.
Limitations
The inclusion of studies published only in English may have overlooked evidence from grey literature and studies in other languages. In addition, the variation in the selected studies may have resulted in a lack of homogeneity in the quality assessment.
Recommendations
The review suggests conducting more clinical trials with larger sample sizes in specific areas, such as novel electrotherapeutic modalities, to enable more effective meta-analysis. The author also suggests including other outcome measures specific to lymphedema and its symptoms.
CONCLUSION
This systematic review identified positive effects of various electro-therapeutic modalities in BCRL and shoulder dysfunction. They had significant improvement in terms of arm circumference, volume, shoulder ROM, pain and disability and overall QOL. This has been confirmed by the meta-analysis performed among six of the selected studies. Hence, the authors strongly advocate for the thoughtful and informed implementation of electro-therapeutic modalities in clinical practice, ensuring they are applied with the utmost care and attention to patient needs.
Ethical approval:
The research/study was approved by the Institutional Review Board at Institute of Physiotherapy, KLE Academy of Higher Education and Research, number 617, dated 1st December 2023.
Declaration of patient consent:
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-49.
- [CrossRef] [PubMed] [Google Scholar]
- Breast Cancer in India: Present Scenario and the Challenges Ahead. World J Clin Oncol. 2022;13:209-18.
- [CrossRef] [PubMed] [Google Scholar]
- Late Effects, Long-term Problems and Unmet Needs of Cancer Survivors. Int J Cancer. 2022;151:1280-90.
- [CrossRef] [PubMed] [Google Scholar]
- Long-Term Quality of Life Profile in Oncology: A Comparison between Cancer Survivors and the General Population. Support Care Cancer. 2018;26:651-6.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of unilateral arm lymphoedema after breast cancer: A systematic review and meta-analysis. Lancet Oncol. 2013;14:500-15.
- [CrossRef] [PubMed] [Google Scholar]
- Response of Post-Mastectomy Lymphedema to Extracorporeal Shockwave Therapy. J Surg. 2016;4:14.
- [CrossRef] [Google Scholar]
- Head and Neck Cancer Survivorship Care Guideline: American Society of Clinical Oncology Clinical Practice Guideline Endorsement of the American Cancer Society Guideline. J Clin Oncol. 2017;35:1606-21.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and Nature of Survivorship Needs in Patients with Head and Neck Cancer. Head Neck. 2016;38:1097-103.
- [CrossRef] [PubMed] [Google Scholar]
- Safety, Precautions, and Modalities in Cancer Rehabilitation: An Updated Review. Curr Phys Med Rehabil Rep. 2021;9:142-53.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic Review of the Problems and Issues of Accessing Specialist Palliative Care by Patients, Carers and Health and Social Care Professionals. Palliat Med. 2004;18:525-42.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to Cancer Rehabilitation: Healthcare Professionals' Perspective in Saudi Arabia. Phys Med Rehab Kuror. 2019;58:317-22.
- [CrossRef] [Google Scholar]
- Current Practice and Barriers in Cancer Rehabilitation: Perspectives of Korean Physiatrists. Cancer Res Treat. 2015;47:370-8.
- [CrossRef] [PubMed] [Google Scholar]
- The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of Extracorporeal Shock Waves Therapy Versus Intermittent Pneumatic Compression Therapy in Breast Cancer-related Lymphedema. Int J Cancer Res. 2018;14:77-85.
- [CrossRef] [Google Scholar]
- Effectiveness of a Nonpneumatic Active Compression Device in Older Adults with Breast Cancer-Related Lymphedema: A Subanalysis of a Randomized Crossover Trial. Lymphat Res Biol. 2023;21:581-4.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of the Combined Use of Complex Decongestive Therapy with Electrotherapy Modalities for the Treatment of Breast Cancer-related Lymphedema: A Randomized Clinical Trial. BMC Musculoskelet Disord. 2022;23:837.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of the effectiveness of complex decongestive therapy and extracorporeal shock wave therapy in the treatment of lymphedema secondary to breast cancer. Indian J Surg. 2021;83:749-53.
- [CrossRef] [Google Scholar]
- Effects of Extracorporeal Shockwave Therapy on Improvements in Lymphedema, Quality of Life, and Fibrous Tissue in Breast Cancer-Related Lymphedema. Ann Rehabil Med. 2020;44:386-92.
- [CrossRef] [PubMed] [Google Scholar]
- Intermittent pneumatic compression pump in upper extremity impairments of breast cancer-related lymphedema. Turk J Med Sci. 2013;43:99-103.
- [CrossRef] [Google Scholar]
- Investigation of the Effect of Low-Level Laser Therapy on arm Lymphedema in Breast Cancer Patients: A Noninvasive Treatment for an Intractable Morbidity. Health Sci Rep. 2023;6:e1261.
- [CrossRef] [PubMed] [Google Scholar]
- Long-Term Effects of Extracorporeal Shock Wave Therapy on Breast Cancer-Related Lymphedema. J Clin Med. 2022;11:6747.
- [CrossRef] [PubMed] [Google Scholar]
- The Effects of Complex Decongestive Therapy on Pain and Functionality in Individuals with Breast Cancer who Developed Adhesive Capsulitis due to Lymphedema: An Evaluation by an Isokinetic Computerized System. Korean J Pain. 2022;35:280-90.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Outcomes of Extracorporeal Shock Wave Therapy in Patients with Secondary Lymphedema: A Pilot Study. Ann Rehabil Med. 2013;37:229-34.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal Shockwave Therapy for Post-Menopausal Patients with Breast Cancer-Related Lymphedema. Int J Cancer Res. 2015;49:1618-1625.
- [Google Scholar]
- Kinesio Taping and Low-level Laser Therapy in Breast Cancer-Related Lymphedema in an Arm with Arteriovenous Fistula for Hemodialysis. Turk J Phys Med Rehabil. 2020;66:214-8.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Intermittent Pneumatic Compression in the Treatment of Breast Cancer-related Lymphoedema: A Randomized Controlled Trial. Clin Rehabil. 2020;34:220-8.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and Effectiveness of a Novel Nonpneumatic Active Compression Device for Treating Breast Cancer-Related Lymphedema: A Multicenter Randomized, Crossover Trial (NILE) J Vasc Surg Venous Lymphat Disord. 2022;10:1359-66.e1.
- [CrossRef] [PubMed] [Google Scholar]
- The Randomized Controlled Study of Low-Level Laser Therapy, Kinesio-Taping and Manual Lymphatic Drainage in Patients With Stage II Breast Cancer-Related Lymphedema. Eur J Breast Health. 2023;19:34-44.
- [CrossRef] [PubMed] [Google Scholar]
- A Pilot Randomized Trial Evaluating Low-level Laser Therapy as an Alternative Treatment to Manual Lymphatic Drainage for Breast Cancer-Related Lymphedema. Oncol Nurs Forum. 2013;40:383-93.
- [CrossRef] [PubMed] [Google Scholar]
- Helium Neon Laser Therapy for Post Mastectomy Lymphedema and Shoulder Mobility. Egypt J Med Hum Genet. 2013;14:195-9.
- [CrossRef] [Google Scholar]
- Photobiomodulation Therapy in Breast Cancer-Related Lymphedema: A Randomized Placebo-controlled Trial. Photodermatol Photoimmunol Photomed. 2017;33:32-40.
- [CrossRef] [PubMed] [Google Scholar]
- Low-Energy Extracorporeal Shockwave Therapy as a Therapeutic Option for Patients with a Secondary Late-Stage Fibro-Lymphedema After Breast Cancer Therapy: A Pilot Study. Lymphat Res Biol. 2021;19:175-80.
- [CrossRef] [PubMed] [Google Scholar]
- Complementary Low-Level Laser Therapy for Breast Cancer-related Lymphedema: A Pilot, Double-Blind, Randomized, Placebo-Controlled Study. Lasers Med Sci. 2020;35:95-105.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of Matrix Rhythm Therapy for Frozen Shoulder in Breast Cancer Related Lymphedema Patient: A case report. Int J Physiother Res. 2020;8:3354-8.
- [CrossRef] [Google Scholar]
- Efficacy of Manual Lymphatic Drainage and Intermittent Pneumatic Compression Pump Use in the Treatment of Lymphedema after Mastectomy: A Randomized Controlled Trial. Breast Cancer. 2015;22:300-7.
- [CrossRef] [PubMed] [Google Scholar]
- Intensive Complex Physical Therapy Combined with Intermittent pneumatic Compression Versus Kinesio Taping for Treating Breast Cancer-Related Lymphedema of the Upper Limb: A Randomised Cross-Over Clinical Trial. Eur J Cancer Care (Engl). 2022;31:e13625.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Intermittent Pneumatic Compression in Combination with Kinesiotape on Post Mastectomy Lymphedema. Egypt J Hosp Med. 2021;85:2794-9.
- [CrossRef] [Google Scholar]
- Matrix Rhythm Therapy (MaRhyThe) and Cupping: A Novel Multimodal Approach for Breast Cancer-Related Lymphedema. BLDE Univ J Health Sci. 2023;8:171.
- [CrossRef] [Google Scholar]
- Intermittent Pneumatic Compression in Patients with Postmastectomy Lymphedema. Family Med Primary Care Rev. 2016;18:419-24.
- [CrossRef] [Google Scholar]
- Extracorporeal Shock Waves, a New Non-Surgical Method to Treat Severe Burns. Burns. 2010;36:844-9.
- [CrossRef] [PubMed] [Google Scholar]
- Lymphatic Vessels in Regenerative Medicine and Tissue Engineering. Tissue Eng Part B Rev. 2016;22:395-407.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal Shock Wave Therapy Induces Therapeutic Lymphangiogenesis in a Rat Model of Secondary Lymphoedema. Eur J Vasc Endovasc Surg. 2011;42:254-60.
- [CrossRef] [PubMed] [Google Scholar]
- NAALT - North American Association for Photobiomodulation Therapy. Available from: https://www.naalt.org [Last accessed on 2024 Apr 24]
- [Google Scholar]
- Advanced Pneumatic Compression for Treatment of Lymphedema of the Head and Neck: A Randomized Wait-List Controlled Trial. Support Care Cancer. 2021;29:795-803.
- [CrossRef] [PubMed] [Google Scholar]
- The Application of Matrix Rhythm Therapy as a New Clinical Modality in Burn Physiotherapy Programmes. Burns. 2014;40:909-14.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Matrix Rhythm Therapy (MaRhyThe) in Plantar Fasciitis-an Experimental Study. Indian J Phys Ther Res. 2019;1:105-9.
- [CrossRef] [Google Scholar]
- Evaluation of Long-Term Effect of Clinical Physiotherapy Treatment Protocol for Post Cancer Mastectomy Induced Lymphadenopathy and Restricted Joint Range: A Novel Protocol Case Study. Integr Oncol. 2018;7:219.
- [CrossRef] [Google Scholar]







