Translate this page into:
Role of Yoga in Cancer Patients: Expectations, Benefits, and Risks: A Review
Address for correspondence: Dr. Raghavendra Mohan Rao, Healthcare Global Enterprises Ltd., No. 8, P Kalinga Rao Road, Sampangiramnagar, Bengaluru - 560 027, Karnataka, India. E-mail: raghav.hcgrf@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The diagnosis and treatment of cancer poses severe psychologic distress that impacts functional quality of life. While cancer directed treatments are directed purely against tumor killing, interventions that reduce treatment related distress and improve quality of life are the need of the hour. Yoga is one such mind body intervention that is gaining popularity among cancer patients.
Method:
Several research studies in the last two decades unravel the benefits of yoga in terms of improved mood states, symptom reduction, stress reduction and improved quality of life apart from improving host factors that are known to affect survival in cancer patients. However, several metaanalysis and reviews show equivocal benefits for yoga. In this review, we will study the Yoga interventions in cancer patients with respect to expectations, benefits and risks and analyse the principles behind tailoring yoga interventions in cancer patients.
Results:
The studies on Yoga show heterogeneity with varied types of Yoga Interventions, duration, exposure, practices and indications. It also elucidates the situational context for reaping benefits and cautions against its use in several others. However, there are several reviews and bibliometric analysis of effects of yoga; most of them have not enlarged the scope of their review to cover the basic principles behind use of these practices in cancer patients.
Conclusion:
This review offers insight into the principles and practice of yoga in cancer patients.
Keywords
Cancer
clinical utility
meditation
risks
yoga
INTRODUCTION
Both diagnosis and treatment of cancer pose physical and psychological threats to the patient. Cancer patients normally receive multimodal treatments over a long period with accompanying cumulative morbidity.[12] Treatment regimens for cancer can pose serious side effects for these patients such as change in appearance, infertility, altered sexual functioning, hair loss, fatigue, nausea and vomiting, pain, infections, and low blood counts, which grossly affect the patients overall functional quality of life (QOL).[345] Fear and anxiety associated with invasive treatment procedures, sexual dysfunction secondary to surgery and radiation, and problems associated with extended hospital care and aggressive medical treatment are among the most common causes for the treatment-related side effects observed in cancer patients. The advances in cancer detection and treatment have improved survival rates for most of the cancers with majority of them surviving with cancer for a longer time than ever before. However, surviving with cancer means a constant reminder about the disease, anxiety about recurrence and progression, and impending death.[6] This coupled with treatment-related side effects can lead to intrusive thoughts and feelings of anxiety, hopelessness and helplessness and can cause severe psychologic distress.[789] There sets in a vicious cycle of anxiety/stress, vasomotor, and pain symptoms that further reduce the patient's ability to tolerate pain and symptoms. This process is catalyzed by situational stressors and daily worries which the cancers patients have to contend reducing their threshold for these symptoms.[10] This leads to increased dependency on medications that come with their accompanying side effects. This treatment-related distress can manifest as anxiety or depressive disorders in some of these cancer patients leading to a state of heightened helplessness/hopelessness, lack of will to survive, loss of control over ones lives, change in attitude toward cancer and survival,[611121314] decrease in threshold for pain and discomfort,[151617] and low self-esteem.[18] Studies have also shown that such a state of mind can lead to sleep disturbances, aberrant cortisol rhythms, poor antitumor immune response, decrease in overall and disease-free survival with early relapse/recurrence, and heightened distress.[19202122] Both treatment-related side effects and associated distress act as a potent short-term and long-term stressors constantly influencing patients to make lifestyle changes to cope and adjust with these problems and seek supportive care.
Oncologists and health professionals working with these patients recognize the need to intervene to break this vicious symptom-distress-symptom cycle. Growing evidence suggests that psychosocial and psychoeducational interventions are beneficial adjunctive treatments for patients with cancer.[232425] These interventions increase perceived control, decrease the potential stigma associated with cancer and having a “psychiatric problem,” and provide a supportive environment where patients can allay their fears and concerns.[2627] Psychosocial interventions decrease depression and anxiety and increase self-esteem and help patients adopt active-approach coping strategies.[282930] In addition, QOL, immune status, and in some cases these programs have enhanced survival times.[233132]
Stress management techniques that have proven helpful include progressive muscle relaxation,[3334] diaphragmatic breathing,[3334] guided imagery,[3334] and social support.[3536] Participating in intervention programs before treatment have enabled patients to tolerate therapy with fewer reported side effects.[3738] Stress-reduction methods are many and varied, and yoga is especially attractive as it combines many of these techniques with simple stretching exercises, breathing, and relaxation techniques that could be useful for patients with cancer.
A growing literature shows the potential benefits of practicing yoga. Yoga is an ancient discipline and its physical and mental health benefits have been described in early texts.[3940] Although it has been used in India for centuries,[3334] it has recently started to gain global recognition.
Yoga is an ancient Indian science and is one among the six great Indian philosophies that have evolved over thousands of years. In the spiritual dimension, yoga is a path toward attainment of superconscious states beyond sensory perception and knowledge. It deals with the physical, mental, moral, and spiritual well-being of an individual.[41] References to yoga are made throughout the Vedas, (ancient Indian scriptures that are among the oldest texts in existence).[3940] The earliest systematic description of this practice and various philosophies was codified into 196 aphorisms in the classic treatise the “Yoga Sutras” of Patanjali, dating back to 900 B.C.,[394042] which helped to define the modern practice of yoga.[43] In his aphorisms, yoga has been defined as “citta vrtti nirodhah” a practice of “controlling of the mind” by a systematic 8-fold path called Astanga Yoga. This pragmatic description enumerates eight stages of yoga, which if practiced systematically allows one to attain a state of sublimation of all mental modifications in the mind and superconsciousness (Samadhi). These systematic yoga techniques include Yama's (moral doctrines), Niyamas (disciplines), Asanas (postures), Pranayama (regulated nostril breathing/breath control), Pratyahara (introspection/in drawing mind away from perceptible external sensory stimuli), Dharana (concentration), Dhyana (meditation), and finally to attain a state of Samadhi (absorption).[41] Attainment of such a contemplative absorptive state has been elucidated to confer a blissful state of mind and body. Similar references to these practices can be found in Buddhist scriptures who equate these yogic practices to mindful exercises. This is also popularly known as mindfulness-based stress reduction (MBSR) program.
World over, the term yoga usually refers to the third and fourth limbs, “Asana” and “Pranayama,” although traditionally the limbs are viewed as interrelated. It is important to note that each of these approaches represents a distinct intervention, in the same way that psychodynamic, cognitive-behavioral, and interpersonal therapies each involve different approaches to psychotherapy.[44]
The first four limbs – Yama, Niyama, Asana, and Pranayama – are considered external cleansing practices that help prepare the mind for internal practices Pratyahara (sense control), Dharana (concentration), and Dhyana (meditation). However, other traditional schools of yoga such as hatha yoga envisage cleansing practices called Kriyas. These cleansing practices are a precursor to asanas and pranayama, ensure proper circulation, digestion, and correct metabolic imbalances that affect flow of prana to all parts of the body.[4546] The asanas improve flexibility and strength and keep these channels open, whereas pranayama facilitates movement of prana across these channels. The asanas and pranayama together help keep the mind calm and prepare the mind to overcome sensory stimulus, reduce the thoughts by helping one to focus and concentrate, and finally relax in meditative states that ensure relaxation response and feeling of well-being. Although there are several other benefits and practices of yoga associated with spiritual upliftment and liberation, we discuss only those that have been used to promote health in cancer patients.
However, ancient Indian yoga scriptures have alluded that each of these eight limbs (steps) affect different aspects of health. Psychosomatic phenomena of disease as proposed in Western psychology is in consonance with Panchakosa theory of existential states according to Upanishads. Accordingly, a holistic concept of health has been proposed in the Upanishads which states that every human being has five existential states.[40] The gross physical body or Annamaya kosa with organs and systems, the subtle functional body or Pranamaya kosa responsible for all physiological functions, the mind with thoughts and emotions as the Manomaya kosa, the intellect or the reasoning as Vignanamaya kosa, and finally the inherent blissful states of awareness called the Anandamaya kosa. The psychosomatic phenomena of disease is explained as a change in perception and ignorance in Vignanamaya Kosa leading to mental turmoil or stress in Manomaya kosa which percolates as physiological changes in the Pranamaya kosa to finally culminate in organic changes in the physical body or Annamayakosa. Using different yoga practices to act at all five levels, we can correct the imbalances at each of these kosas and restore the homeostasis. For example, we use asanas and kriyas at Annamaya kosa level, pranayama at Pranamaya kosa, relaxation and meditation at Manomaya kosa level, counseling at Vignanamaya kosa, and finally by increasing ones internal awareness of these levels with these practices and relaxing we attain deeper states of bliss which is responsible for restoring the homeostasis by bringing relaxation response.
There are several studies that have used various forms and schools of yoga that tend to lay emphasis on either one or more of the above practices popular among them being Iyengar Yoga, Integrated Approach of Yoga Therapy, Sudarshan Kriya Yoga, Vinyasa Yoga, Tibetian Yoga, Integrated Yoga, and Hatha Yoga, etc. Unlike the Eastern traditions, Meditation is considered different from Yoga in the West; popular among them being MBSR and transcendental meditation, etc.
These yoga traditions have been increasingly used in cancer patients to reduce stress, mood states, and symptom distress and improve QOL. We elucidate the psychologic benefits and symptom reduction effects of various yoga interventions and their mechanism of action.
MOOD STATES AND PSYCHOLOGIC DISTRESS
Several studies have shown yoga to reduce self-reported depression, anxiety state, and trait in cancer patients undergoing cancer-directed treatment as well as in survivors.[47484950] Various review articles validate the effects of yoga to have a moderate effect in modulating mood states such as anxiety, depression, and psychologic distress.[485152] Anxiety reduction effects of yoga are primarily due to pranayama and relaxation techniques,[53] whereas antidepressant effects have been attributed to hyperventilation breathing techniques such as Bhastrika, Kapalabhati, and Ujjayi pranayama.[5455] Apart from these asanas or postures are known to reduce psychologic distress and contribute to anxiolytic and antidepressant effects. In a majority of the studies, the duration of the yoga program varies between 4 weeks to 12 weeks with a minimum of two supervised classes per week and home practice on remaining days. A recent Cochrane review has shown yoga to have moderate-quality evidence for reducing depression, anxiety and fatigue, when compared with psychosocial/educational interventions.[56] In another review, yoga showed moderate-to-large effect for psychosocial outcomes.[51] In contradiction, another review showed no significant benefits for anxiety, depression, distress, and sleep.[48]
Meditative movement therapies such as Yoga, tai Chi, and Qi Gong showed to favor health-related QOL in cancer patients.[57]
SYMPTOM MANAGEMENT
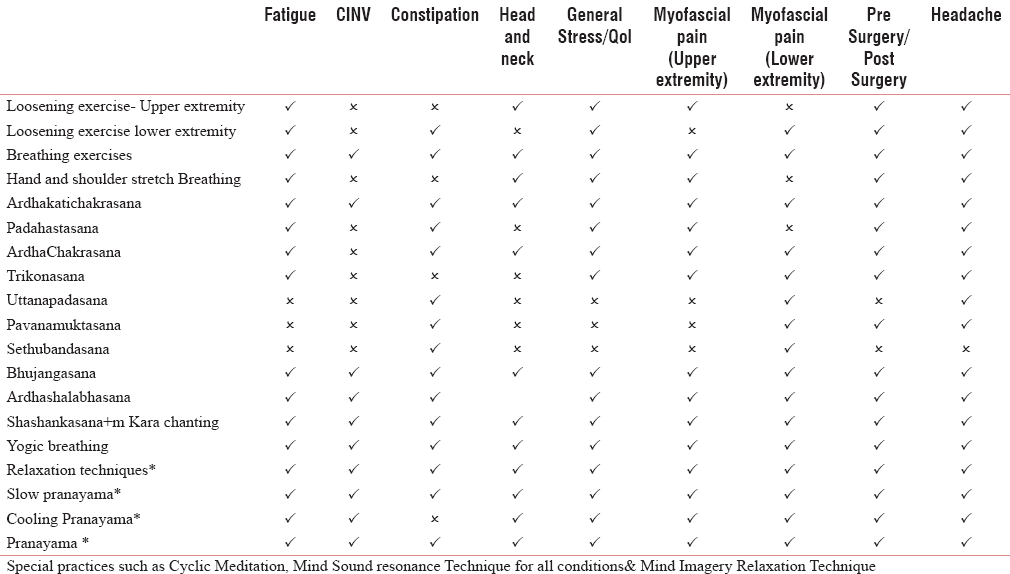
Yoga has been used in the management of a variety of symptoms such as fatigue, sleep disturbances, loss of appetite, chemotherapy-induced nausea and vomiting (CINV), and pain in cancer patients.[5658] The effects of yoga intervention have been moderate to large in these studies. Cooling Pranayama such as Sheetali, Sheetakari, and Sadanta have been useful in managing CINV along with Pavanamuktasana (supine knee-chest) and Uttana padasana (straight leg raise).[58] Loosening exercises, gentle stretches, Yogasanas (stretching postures), Sudarshan kriya, and relaxation techniques have been shown to be effective in managing fatigue, pain, and sleep problems.[59] Techniques that use postures intersped with relaxation techniques (cyclic meditation/movement meditation) have been found to be useful in reducing stress and improving sleep.[60] Mind sound resonance technique that involves chanting and meditating on sound “a,” “u,” and “m,” and mantras have been shown to reduce fear, anxiety, and instill restful state of mind.[61] Other schools of yoga that have used props to facilitate stretching followed by relaxation have also found to reduce fatigue and pain in cancer patients.[62] The asanas chosen for managing symptoms depend on the direction of flow of prana according to Pancha Prana theory. For example, for managing CINV, the problem lies in the correcting Samana vayu whose seat is in the stomach and gut, sluggishness of this vayu causes abdominal discomfort and increase in Udana vayu (upward force) causing vomiting. The use of antiemetic therapy causes gastroparesis and obstructs Udana vayu and Apana vayu (downward force) causing nausea. By doing postures that work on abdomen, we facilitate the downward flow of the otherwise sluggish Apana vayu that reduces nausea and improves appetite. Similarly, fatigue is caused due to sluggish Samana vayu and obstructed flow of vyana that causes myalgia and fatigue on exertion. Various modules of yoga can be tailored to meet the needs of cancer patients. Some of these modules for various symptoms are given in Table 1.
MECHANISM OF ACTION OF YOGA INTERVENTION
Apart from the physical benefits of yoga as described above, reduction in stress hormones, HPA axis regulation, relaxation response, and improved parasympathetic function are known to reduce stress and modulate response to stressors and instill a greater control over situations.[6364] This is particularly useful in cancer patients who perceive cancer as a threat and constantly ruminate on its fears. For example, depression causes abnormal diurnal cortisol elevations that can affect sleep and cause insomnia and immune suppression.[1921] By changing perceptions and reactivity to situations and reducing intrusive thoughts a reduction in depressive symptoms have been seen. This in turn translates to reduction in cortisol peaks that is known to reduce fatigue, improve sleep, and consequent immune response. Yoga is known to modulate this psychoneuroendocrine and psychoneuroimmune axis thereby restoring homeostasis and reducing the allostatic load.[6365] These effects have been observed in numerous studies of yoga that have shown reductions in cortisol, inflammatory cytokines,[6667] and improved natural killer cell counts.[636869] These changes have been shown to modulate distressful symptoms and improve QOL of these patients.
CONTRAINDICATIONS OF YOGA INTERVENTIONS
Although yoga is useful in improving fitness and health in both healthy and disease populations, caution is advised while dealing with cancer patients due to their disease condition and increased propensity for injury. None of the earlier studies with yoga in cancer patients reported side effects following yoga intervention. However, bone metastases in long bones present an increased risk of fracture with some asanas, especially in the elderly population. Second, hyperventilation practices have been shown to cause pneumothorax earlier,[70] the chances of this is high in patients with lung cancer or lung metastases undergoing radiotherapy. Patients having pleural effusion, ascites, abdominal surgeries, etc., need a more cautious approach with yoga interventions, slow deep breathing, pranayama, and relaxation techniques being useful in these conditions. The performance status and general condition of the patient are of paramount importance while selecting yoga interventions.
Yoga is a promising mind-body intervention for integration in an oncology setting. However, most of the studies with yoga and meditation intervention have been done on breast cancer patients. We need to evaluate the effects of these interventions in other solid malignancies, head and neck, lung and cervical cancer patients that form a major burden of cancer in the country. We also need to evaluate the effects of this intervention under different treatment scenarios. Yoga is a feasible intervention used to reduce symptom burden and improve QOL in cancer patients. However, studies are needed to evaluate its cost-effectiveness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997;337:949-55.
- [Google Scholar]
- Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337:956-62.
- [Google Scholar]
- Symptom clusters in advanced cancer patients: An empirical comparison of statistical methods and the impact on quality of life. J Pain Symptom Manage. 2016;51:88-98.
- [Google Scholar]
- Symptom clusters of ovarian cancer patients undergoing chemotherapy, and their emotional status and quality of life. Eur J Oncol Nurs. 2016;21:215-22.
- [Google Scholar]
- Effects of symptom clusters and depression on the quality of life in patients with advanced lung cancer. Eur J Cancer Care (Engl) 2016 April 26
- [Google Scholar]
- Influence of psychological response on breast cancer survival: 10-year follow-up of a population-based cohort. Eur J Cancer. 2005;41:1710-4.
- [Google Scholar]
- Patient perceptions of the side-effects of chemotherapy: The influence of 5HT3 antagonists. Br J Cancer. 1997;76:1055-61.
- [Google Scholar]
- Quality-of-life-adjusted evaluation of adjuvant therapies for operable breast cancer. The International Breast Cancer Study Group. Ann Intern Med. 1991;114:621-8.
- [Google Scholar]
- Adjuvant psychological therapy for patients with cancer: A prospective randomised trial. BMJ. 1992;304:675-80.
- [Google Scholar]
- Sleep problems in breast cancer survivors 1-10 years posttreatment. Palliat Support Care. 2017;16:1-10.
- [Google Scholar]
- Global quality of life and its potential predictors in breast cancer patients: An exploratory study. Support Care Cancer. 2007;15:21-30.
- [Google Scholar]
- Influence of psychological coping on survival and recurrence in people with cancer: Systematic review. BMJ. 2002;325:1066.
- [Google Scholar]
- Psychiatric disorders following first breast cancer recurrence: Prevalence, associated factors and relationship to quality of life. Jpn J Clin Oncol. 2005;35:302-9.
- [Google Scholar]
- Gender-dependent effect on nociceptive response induced by chronic variable stress. Physiol Behav. 2014;135:44-8.
- [Google Scholar]
- Acute psychosocial stress reduces pain modulation capabilities in healthy men. Pain. 2014;155:2418-25.
- [Google Scholar]
- Short-term pre- and post-operative stress prolongs incision-induced pain hypersensitivity without changing basal pain perception. Mol Pain. 2015;11:73.
- [Google Scholar]
- Evaluation of self-esteem in cancer patients undergoing chemotherapy treatment. Rev Lat Am Enfermagem. 2015;23:1082-9.
- [Google Scholar]
- Repression and high anxiety are associated with aberrant diurnal cortisol rhythms in women with metastatic breast cancer. Health Psychol. 2004;23:645-50.
- [Google Scholar]
- Predictors of patterns of pain, fatigue, and insomnia during the first year after a cancer diagnosis in the elderly. Cancer Nurs. 2008;31:334-44.
- [Google Scholar]
- Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92:994-1000.
- [Google Scholar]
- Flattened cortisol rhythms in metastatic breast cancer patients. Psychoneuroendocrinology. 2004;29:1082-92.
- [Google Scholar]
- Malignant melanoma. Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Arch Gen Psychiatry. 1993;50:681-9.
- [Google Scholar]
- Effects of psychosocial interventions with adult cancer patients: A meta-analysis of randomized experiments. Health Psychol. 1995;14:101-8.
- [Google Scholar]
- Etiology and treatment of the psychological side effects associated with cancer chemotherapy: A critical review and discussion. Psychol Bull. 1988;104:307-25.
- [Google Scholar]
- Managing stress and managing illness: Survival and quality of life in chronic disease. J Clin Psychol Med Settings. 1995;2:309-33.
- [Google Scholar]
- A structured psychiatric intervention for cancer patients. II. Changes over time in immunological measures. Arch Gen Psychiatry. 1990;47:729-35.
- [Google Scholar]
- Long-term effects of educational and peer discussion group interventions on adjustment to breast cancer. Health Psychol. 2001;20:387-92.
- [Google Scholar]
- Education and peer discussion group interventions and adjustment to breast cancer. Arch Gen Psychiatry. 1999;56:340-7.
- [Google Scholar]
- The effect of compliance with treatment on survival among patients with hematologic malignancies. J Clin Oncol. 1990;8:356-64.
- [Google Scholar]
- Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2:888-91.
- [Google Scholar]
- Progressive muscle relaxation and guided imagery in cancer patients. Gen Hosp Psychiatry. 1994;16:340-7.
- [Google Scholar]
- Relaxation and imagery for anxiety and depression control in community patients with advanced cancer. Cancer Nurs. 2002;25:432-5.
- [Google Scholar]
- Coping, life attitudes, and immune responses to imagery and group support after breast cancer treatment. Altern Ther Health Med. 1997;3:62-70.
- [Google Scholar]
- Social support and salivary cortisol in women with metastatic breast cancer. Psychosom Med. 2000;62:337-45.
- [Google Scholar]
- Relaxation to reduce nausea, vomiting, and anxiety induced by chemotherapy in Japanese patients. Cancer Nurs. 1997;20:342-9.
- [Google Scholar]
- Preoperative rehearsal of active coping imagery influences subjective and hormonal responses to abdominal surgery. Psychosom Med. 1995;57:177-82.
- [Google Scholar]
- The Science of Yoga. Chennai: Adyar Library and research center; 1996.
- Yoga the Science of Holistic Living. Chennai: Vivekananda Kendra Prakashan Trust; 2005.
- The Science of Yoga: The Yoga-Sutras of Patanjali in Sanskrit. Adyar Library and Research center; 1999.
- Patañjali, undefined. Patanjali Yoga Sutras. Vedanta society of southern California 1953
- 2002. Hatha Yoga Pradipika. Available from: https://www.yogabookingportal.com/Yogabooks/HathaYogaPradipika-SanskritTextWithEnglishTranslatlionAndNotes.pdf
- Characteristics of randomized controlled trials of yoga: A bibliometric analysis. BMC Complement Altern Med. 2014;14:328.
- [Google Scholar]
- Effects of yoga on psychologic function and quality of life in women with breast cancer: A meta-analysis of randomized controlled trials. J Altern Complement Med. 2012;18:994-1002.
- [Google Scholar]
- Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1:CD010802.
- [Google Scholar]
- The evolution of psychological distress trajectories in women diagnosed with advanced breast cancer: A longitudinal study. Psychooncology. 2013;22:2831-9.
- [Google Scholar]
- Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 2012;12:559.
- [Google Scholar]
- Yoga for breast cancer patients and survivors: A systematic review and meta-analysis. BMC Cancer. 2012;12:412.
- [Google Scholar]
- Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: A randomized controlled trial. Complement Ther Med. 2009;17:1-8.
- [Google Scholar]
- Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255-9.
- [Google Scholar]
- Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006;94:249-53.
- [Google Scholar]
- Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1:CD010802.
- [Google Scholar]
- ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: Executive Summary. JACC. 2011;57:1002-44.
- [Google Scholar]
- Effects of an integrated yoga programme on chemotherapy-induced nausea and emesis in breast cancer patients. Eur J Cancer Care (Engl). 2007;16:462-74.
- [Google Scholar]
- Randomized controlled trial in advance stage breast cancer patients for the effectiveness on stress marker and pain through Sudarshan Kriya and Pranayam. Indian J Palliat Care. 2013;19:180-5.
- [Google Scholar]
- Autonomic changes during “OM” meditation. Indian J Physiol Pharmacol. 1995;39:418-20.
- [Google Scholar]
- Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23:135-42.
- [Google Scholar]
- Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: A randomized controlled trial. Integr Cancer Ther. 2009;8:37-46.
- [Google Scholar]
- Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448-74.
- [Google Scholar]
- Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12:278-85.
- [Google Scholar]
- Qigong/Tai Chi Easy for fatigue in breast cancer survivors: Rationale and design of a randomized clinical trial. Contemp Clin Trials. 2016;50:222-8.
- [Google Scholar]
- Influence of yoga on mood states, distress, quality of life and immune outcomes in early stage breast cancer patients undergoing surgery. Int J Yoga. 2008;1:11-20.
- [Google Scholar]
- Effects of yoga on natural killer cell counts in early breast cancer patients undergoing conventional treatment. Comment to: Recreational music-making modulates natural killer cell activity, cytokines, and mood states in corporate employees Masatada Wachi, Masahiro Koyama, Masanori Utsuyama, Barry B. Bittman, Masanobu Kitagawa, Katsuiku Hirokawa Med Sci Monit. 2007;13(2):CR57-70. Med Sci Monit 2008;14:LE3-4
- [Google Scholar]
- Effects of yoga on symptom management in breast cancer patients: A randomized controlled trial. Int J Yoga. 2009;2:73-9.
- [Google Scholar]
- Kapalabhati pranayama: Breath of fire or cause of pneumothorax? A case report. Chest. 2004;125:1951-2.
- [Google Scholar]






