Translate this page into:
The Effect of Acupressure on Fatigue in Cancer Patients: A Meta-analysis Study
*Corresponding author: Melike Demir Doğan, Department of Nursing, Gümüşhane University Faculty of Health Sciences, Gümüşhane, Turkey. melekdm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Demir Doğan M. The Effect of Acupressure on Fatigue in Cancer Patients: A Meta-analysis Study. Indian J Palliat Care. 2024;30:10-5. doi: 10.25259/IJPC_95_2023
Abstract
Objectives:
This meta-analysis study was conducted to determine how acupressure affects fatigue in cancer patients.
Materials and Methods:
Randomised controlled clinical trials were conducted using the keywords ‘acupressure and fatigue’ on Google Scholar, PubMed, and ISI Web of Sciences databases. Cochran’s Q test statistics and I2 test statistics were used to test the presence of heterogeneity. The random-effect meta-analysis model was used according to the results of the test for heterogeneity. Hedge’s g test statistics were used to determine the joint effect between acupressure and control groups in the meta-analysis study.
Results:
In this meta-analysis study, 409 patients from the acupressure group and 403 patients from the control group were included. When calculating the average standardised difference value of the acupressure versus the control group, it was determined that acupressure decreased the fatigue score in a statistically significant way.
Conclusion:
Acupressure is an effective approach to alleviate cancer-related fatigue.
Keywords
Acupressure
Fatigue
Meta-analysis
INTRODUCTION
Cancer is one of the major diseases that threaten human health and affects the lives of patients biologically, psychologically, socially, and economically. According to the latest data from the World Health Organization, it has been determined that 19.2 million people have been diagnosed with new cancer.[1]
Cancer-related fatigue is the most commonly reported symptom of cancer and cancer treatment.[2,3] While up to 90% of patients suffer from fatigue symptoms during the treatment stage,[4] this rate is estimated to occur in 27–82% of patients after treatment.[5] Fatigue symptom is seen in 97% of advanced cancer patients.[6]
Although the aetiology of cancer-related fatigue is exactly unknown,[3] there is evidence that it is associated with many biological processes, including immune response, inflammation, metabolic, neuroendocrine, and dysfunction within the central nervous system as well as elevations in specific neurotransmitters and metabolites.[7-9]
The management of cancer-related fatigue includes pharmacotherapy, haemoglobin elevation, exercise, energy conservation, activity management, psycho-educational interventions, diet and nutrition management, sleep therapy, management of disturbing symptoms, and complementary and alternative medicine.[10] Amongst these methods, exercise (aerobic and resistance training), cognitive behavioural therapies, and psychoeducational therapies are currently the only standard evidence-based recommendations for the treatment of cancer-related fatigue.[11]
Various complementary and alternative therapies are generally used to manage the side effects and symptoms of cancer treatments, including fatigue.[12] Acupressure is a complementary therapy based on traditional Chinese medicine’s theory of energy pathways and on the premise that restoring proper energy flow through these pathways can contribute to health and well-being as well as the reduction of physical symptoms.[13,14] Acupressure includes applying pressure to specific points of the body using the hands, fingers, thumbs, elbows, feet or various devices.[15,16] Acupressure is non-invasive and typically painless and side effects associated with the insertion of fine needles can be prevented.[16]
It is emphasised that acupuncture point stimulation may have a promising role in the management of cancer-related fatigue.[17] In studies, acupressure has been used in various patient populations to treat a variety of symptoms and the study results have indicated that acupressure can help reduce stress, pain, and anxiety.[18-21]
The studies have supported the promising role of acupressure in the management of fatigue in cancer patients.[22-24] In light of this information, this meta-analysis study was conducted to determine how acupressure affects the management of fatigue in cancer patients.
MATERIALS AND METHODS
Data searches and study selection
Randomised controlled clinical trials were conducted using the keywords ‘acupressure and fatigue’ on Google Scholar, PubMed, and ISI Web of Sciences databases. This meta-analysis involved only studies comparing the experimental group and the control group. Selection criteria were randomised trials including adults suffering from fatigue and conducted with at least one group treated with acupressure. Studies that were written in English and whose full text can be accessed were included in this meta-analysis study.
As a result of screening with keywords in the PubMed database, nine randomised controlled trials were reached. As a result of the screening made from the Web of Sciences database, 116 randomised controlled studies were reached. As a result of screening from the Google Scholar database, 14000 results were found. After selecting studies in oncology patients and removing identical studies, 18 studies remained. The full text of two of these studies could not be reached. One of them was removed because their language was not written in English. As a result, 15 studies were included in the meta-analysis [Figure 1].

- Flow diagram of study inclusion and exclusions. RCT: Randomized controlled trial.
Data analysis
Cochran’s Q test statistics and I2 test statistics were used to test heterogeneity so that it was determined whether the effect size was significantly different from the studies in the meta-analysis or not. The random-effect meta-analysis model was used according to the results of the test for heterogeneity. Hedge’s g-test statistics were used to show the joint effect between acupressure therapy and control groups in the meta-analysis.
RESULTS
Characteristics of studies
Table 1 shows the characteristics of the studies included in the meta-analysis. In a randomised controlled study, the participants were evaluated into three groups. Acupressure was applied on the acupoints of Zusanli (ST-36), Hegu (LI-4), and Sanyinjiao (SP-6) in the acupressure group (n = 30). Sham pressure was used in the placebo group (n = 30) and no intervention was applied in the control group (n = 30). The fatigue levels of the participants in three groups were calculated in three phases: Before, during, and after chemotherapy. As a result of the study, it was reported that the fatigue level of the acupressure group was statistically significantly lower than the levels of the other groups.[22]
| Study | Intervention | Control | Outcome |
|---|---|---|---|
| Khanghah et al., 2019a | Acupressure n=30 Zusanli (ST-36), Hegu (LI-4) and Sanyinjiao (SP-6). Each point bilaterally for 2 min during and after chemotherapy. |
Sham acupressure n=30 |
The fatigue level of the acupressure group was statistically significantly lower. A visual analogue scale was used. |
| Khanghah et al., 2019b | Acupressure n=30 Zusanli (ST-36), Hegu (LI-4) and Sanyinjiao (SP-6). Each point bilaterally for 2 min during and after chemotherapy |
Usual care n=30 | The fatigue level of the acupressure group was statistically significantly lower. A Visual analogue scale was used. |
| Zick et al., 2011a | Relaxation acupressure n=12 Yin tang, anmian (bilaterally), heart 7 (bilaterally), liver 3 (bilaterally), and spleen 6 (bilaterally) twice a day |
Low-dose stimulating acupressure n=11 Stomach 36 (bilaterally), spleen 6 (bilaterally), kidney 3 (bilaterally), large intestine 4 (bilaterally), conception vessel 6, and governing vessel 20. 3 times a week |
Fatigue level was significantly lower in the relaxation acupressure group. A brief Fatigue Inventory was used. |
| Zick et al., 2011b | Relaxation acupressure n=12 Yin tang, anmian (bilaterally), heart 7 (bilaterally), liver 3 (bilaterally), and spleen 6 (bilaterally) Twice a day |
High-dose stimulating Acupressure n=12 Stomach 36 (bilaterally), spleen 6 (bilaterally), kidney 3 (bilaterally), large intestine 4 (bilaterally), conception vessel 6, and governing vessel 20. twice a day |
Fatigue level was significantly lower in the relaxation acupressure group. A brief fatigue inventory was used. |
| Zick et al., 2016a | Stimulating acupressure n=94 Du 20, conception vessel 6, large intestine 4, stomach 36, spleen 6, and kidney 3. Once per day Each point is in a circular motion for 3 min. |
Usual care n=96 | At week 10, the change in fatigue score from baseline was greater in stimulating acupressure compared to usual care. A brief Fatigue Inventory was used. |
| Zick et al., 2016b | Relaxing acupressure n=98 Yin tang, anmian, heart 7, spleen 6, and liver 3. Once per day Each point is in a circular motion for 3 min. |
Usual care n=96 | At week 10, the change in fatigue score from baseline was greater in relaxing acupressure compared to usual care. A brief fatigue inventory was used. |
| Molassiotis et al., 2007a | Acupressure group n=16 LI-4 (Hegu), SP-6 (Sanyinjiao), ST-36 (Zusanli) Each point for 1 minute, daily for 2 weeks. |
Acupuncture group n=15 LI-4, SP-6 and ST-36 |
Fatigue level improved significantly in the acupressure group. Multidimensional fatigue inventory was used. |
| Molassiotis et al., 2007b | Acupressure group n=16 LI-4 (Hegu), SP-6 (Sanyinjiao), ST-36 (Zusanli) Each point for 1 minute, daily for 2 weeks. |
Sham acupressure n=16 | Fatigue level improved significantly in the acupressure group. Multidimensional Fatigue Inventory was used. |
| Tang et al., 2014a | Acupressure n=24 Hegu (LI-4), Zusanli (ST-36) and Sanyinjiao (SP-6) |
Sham acupressure n=16 |
No statistically significant difference was found Tang fatigue rating scale was used. |
| Tang et al., 2014b | Acupressure with essential oils n=17 Hegu (LI-4), Zusanli (ST-36) and Sanyingjiao (SP-6) |
Sham acupressure n=16 |
No statistically significant difference was found Tang fatigue rating scale was used. |
| Yeh et al., 2016 | Auricular acupressure n=16 HT-7 (Shenmen), MA-TF1 (sympathetic), AT-3 (occiput) 3 min per time, 3 times per day, once a week for 4 weeks |
Sham acupressure n=15 | Fatigue level improved significantly in the acupressure group. M.D. Anderson symptom inventory was used. |
| Yorke et al., 2015 | Acupressure n=50 L-7 (Lieque), L-9 (Taiyuan), LI-4 (Hegu), CV-21 (Qianding), GV-22 (Xinhui), ST-36 (Zusanli) Each point for 1 minute at least twice a day for 4 weeks |
Usual care n=51 | At week 12, fatigue level improved significantly in the acupressure group. Functional assessment of cancer therapy fatigue was used. |
| Özdemir and Taşçı, 2023 | Acupressure n=15 Hands and legs (LI-4, SP-6, ST-36) 3 min twice daily, for 4 weeks |
Usual care n=16 | Fatigue level improved significantly in the acupressure group. A Piper fatigue scale was used. |
| Cheung et al., 2022 | Acupressure n=15 Two 2 h training sessions in self-administered acupressure in 1 week (4 h) Three 1 h weekly follow-up visits for reinforcing practice over 3 weeks (3 h) 15 minutes of self-administered acupressure twice a day after completing the two training sessions |
Health education n=15 Usual care and it was contacted in the 3rd week to attend a health talk unrelated to symptom management |
No statistically significant difference was found. Self-administered acupressure intervention was used. |
| Zhang et al., 2017 | Acupressure n=21 LI-4 (Hegu), ST-36 (Zusanli), SP-6 (Sanyinjiao) Each acupoint for 10 min (30 min/d), 3 d weekly for 12 weeks |
Sham acupressure n=22 | Fatigue level improved significantly in the acupressure group. Multidimensional fatigue inventory was used. |
a: The first group compared within the same study with more than one group (Placebo+experiment+control etc.), b: Second group compared in the same study with more than one group (Placebo+experiment+control etc.)
Similarly, in another study, patients were evaluated in three groups including relaxation acupressure (n = 12), low-dose stimulating acupressure (n = 11), and high-dose stimulating acupressure (n = 12). Those in the high-dose stimulating acupressure group and the relaxation acupressure group applied acupressure to themselves twice a day. The low-dose stimulating acupressure group applied acupressure to themselves 3 times a week. As a result of the study, it was reported that the fatigue level of the relaxation acupressure group was statistically significantly lower than the levels of the other groups.[23]
In another study evaluating the effectiveness of relaxation acupressure application, patients were evaluated in three groups relaxation acupressure group (n = 98), stimulating acupressure group (n = 94), and control group (n = 96). It was reported that the fatigue levels of the relaxation acupressure group and the stimulating acupressure group were significantly lower when compared to the control group.[24] In another randomised controlled study, patients were evaluated into three groups acupressure (n = 16), acupuncture (n = 15), and sham acupressure (n = 16). Fatigue levels improved significantly in the acupressure group.[25] Similarly, in another study of three groups, it was reported that there was no significant difference in terms of fatigue level.[26]
In four of the other randomised controlled studies on two groups, it was reported that the level of fatigue in the acupressure group statistically significantly improved.[27-30] In the other randomised controlled study, no significant difference was reported.[31]
Effects of acupressure on fatigue
In the meta-analysis examining the effect of acupressure on fatigue in cancer patients, 15 randomised controlled trials were included. Of 409 patients from the acupressure group and 403 patients from the control group were evaluated. When the effect of acupressure on fatigue was assessed, it was observed that the groups had a heterogeneous distribution (Q = 68.686, P < 0.001; I2 = 79.665%). The random-effect model was used in the meta-analysis and Figure 2 shows the comparison of acupressure and control groups as a result of the analysis (95% confidence interval, −0.7,92–−0.156; P = 0.003).
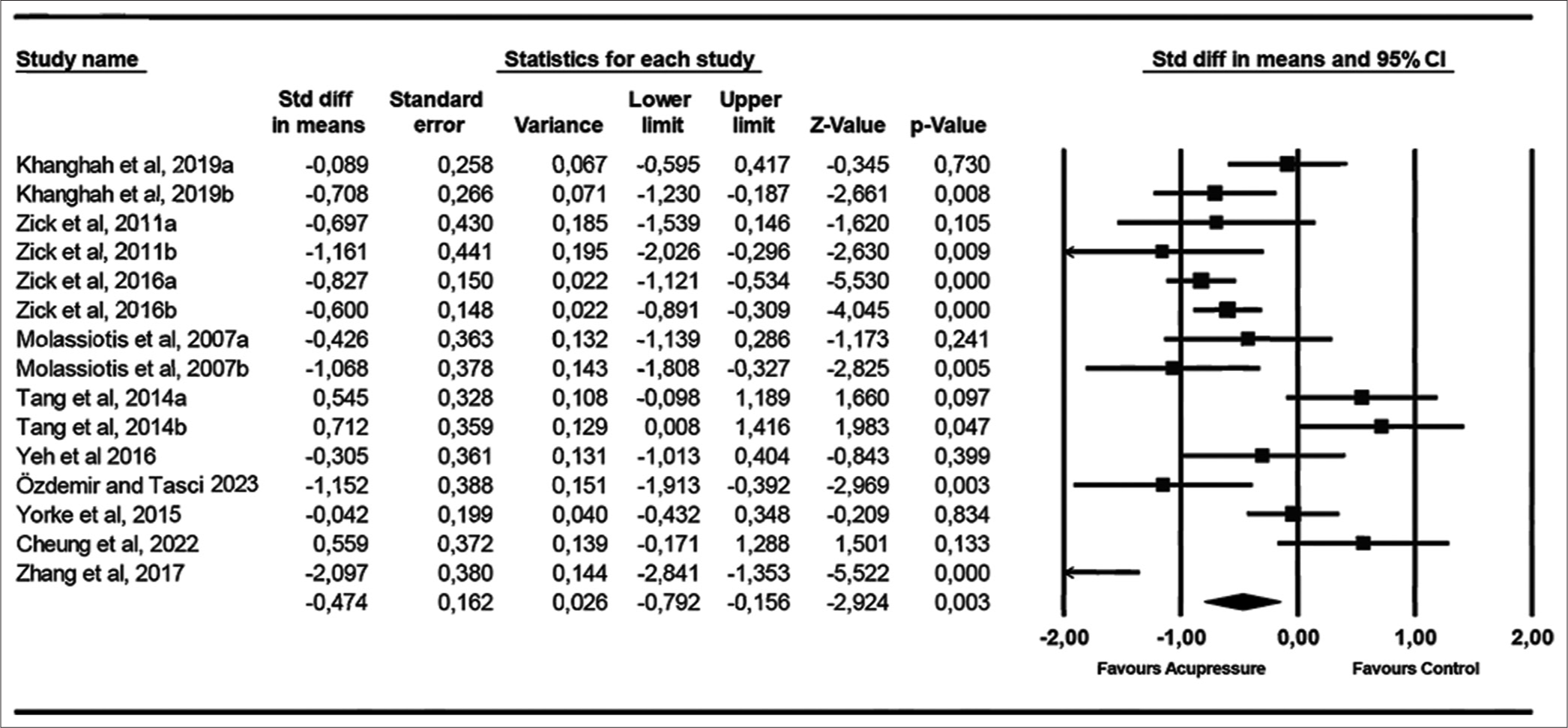
- Forrest plot showing changes acupressure between fatigues. CI: Confidence interval. a: The first group compared within the same study with more than one group (Placebo+experiment+control etc.), b: Second group compared in the same study with more than one group (Placebo+experiment+control etc.).
DISCUSSION
Acupressure is a complementary therapy based on traditional Chinese medicine’s theory of energy pathways and on the premise that restoring proper energy flow through these pathways can contribute to health and well-being as well as the reduction of physical symptoms.[13,14]
Results of the studies have indicated that acupressure can help reduce stress, pain, and anxiety.[18-21] There are studies showing that acupressure is not effective in managing fatigue in cancer patients.[26,31] On the contrary, there are studies reporting that acupressure is effective in managing fatigue in cancer patients.[22-24,27-30]
As a result of a meta-analysis, it was reported that acupuncture and related treatments were effective in reducing pain and fatigue and enhancing quality of life in cancer patients.[32] In a systematic review, it was found that acupuncture and acupressure tended to be effective in relieving fatigue in cancer patients.[33] In a meta-analysis study, it was reported that acupressure was an effective approach to alleviating cancer-related fatigue.[34]
CONCLUSION
Similar to the result of this meta-analysis, it was determined that it was an effective approach to reducing fatigue in cancer patients. To minimise the risk of bias, we included only randomised controlled trials in the meta-analysis study. It is recommended to repeat the meta-analysis with a larger sample size in the future as the number of studies increases. In future studies, repeating meta-analysis with studies using the same acupressure points may be useful for understanding the mechanism of action.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cancer Fact Sheet. 2021. Geneva: World Health Organization; Available from: https://www.who.int/news-room/fact-sheets/detail/cancer [Last accessed on 2021 Aug 06]
- [Google Scholar]
- Cancer-Related Fatigue, Version 2. J Natl Compr Canc Netw. 2015;13:1012-39.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer-Related Fatigue-Mechanisms, Risk Factors, and Treatments. Nat Rev Clin Oncol. 2014;11:597-609.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer-related fatigue: A Review of Nursing Interventions. Br J Community Nurs. 2010;15:214-9.
- [CrossRef] [PubMed] [Google Scholar]
- Symptom Burden and Quality of Life in Survivorship: A Review of the Literature. Cancer Nurs. 2015;38:E29-54.
- [CrossRef] [PubMed] [Google Scholar]
- Correlates of Fatigue Phenomenon in Palliative Care Patients with Advanced Cancers in Taiwan. J Palliat Med. 2012;15:737-43.
- [CrossRef] [PubMed] [Google Scholar]
- The Biology of Cancer-related Fatigue: A Review of the Literature. Support Care Cancer. 2015;23:2461-78.
- [CrossRef] [Google Scholar]
- Altered Resting Brain Connectivity in Persistent Cancer Related Fatigue. Neuroimage Clin. 2015;8:305-13.
- [CrossRef] [PubMed] [Google Scholar]
- Preliminary Differences in Peripheral Immune Markers and Brain Metabolites between Fatigued and Non-fatigued Breast Cancer Survivors: A Pilot Study. Brain Imaging Behav. 2014;8:506-16.
- [CrossRef] [PubMed] [Google Scholar]
- Putting Evidence into Practice: Evidence-based Interventions for Fatigue during and Following Cancer and Its Treatment. Clin J Oncol Nurs. 2007;11:99-113.
- [CrossRef] [PubMed] [Google Scholar]
- Putting Evidence into Practice: An Update of Evidence-based Interventions for Cancer-related Fatigue during and Following Treatment. Clin J Oncol Nurs. 2014;18(Suppl):38-58.
- [CrossRef] [PubMed] [Google Scholar]
- Fatigue in Long-term Breast Carcinoma Survivors: A Longitudinal Investigation. Cancer. 2006;106:751-8.
- [CrossRef] [PubMed] [Google Scholar]
- Classic and Modern Meridian Studies: A Review of Low Hydraulic Resistance Channels along Meridians and Their Relevance for Therapeutic Effects in Traditional Chinese Medicine. Evid Based Complement Alternat Med. 2015;2015:410979.
- [CrossRef] [PubMed] [Google Scholar]
- A New Theory on the Evaluation of Traditional Chinese Acupuncture Mechanisms from the Lates Medical Scientific Point of View. Acupunct Electrother Res. 2015;40:189-204.
- [CrossRef] [PubMed] [Google Scholar]
- Acupressure, Reflexology, and Auricular Acupressure for Insomnia: A Systematic Review of Randomized Controlled Trials. Sleep Med. 2012;13:971-84.
- [CrossRef] [PubMed] [Google Scholar]
- The Efficacy of Acupressure for Symptom Management: A Systematic Review. J Pain Symptom Manage. 2011;42:589-603.
- [CrossRef] [PubMed] [Google Scholar]
- Depression and Insomnia in Cancer: Prevalence, Risk Factors, and Effects on Cancer Outcomes. Curr Psychiatry Rep. 2013;15:404.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Acupressure on Anxiety: A Systematic Review and Meta-analysis. Acupunct Med. 2015;33:353-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Effects of Acupressure on Depression, Anxiety and Stress in Patients with Hemodialysis: A Randomized Controlled Trial. Int J Nurs Stud. 2015;52:509-18.
- [CrossRef] [PubMed] [Google Scholar]
- The Use of Acupressure to Decrease Anxiety in Hospitalized Orthopedic Trauma Patients Requiring Surgical Intervention [Capstone] Baltimore, MD: University of Maryland; 2013.
- [Google Scholar]
- Effect of Selfacupressure for Symptom Management: A Systematic Review. Complement Ther Med. 2015;23:68-78.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Acupressure on Fatigue in Patients with Cancer Who Underwent Chemotherapy. J Acupunct Meridian Stud. 2019;12:103-10.
- [CrossRef] [PubMed] [Google Scholar]
- Relaxation Acupressure Reduces Persistent Cancer-related Fatigue. Evid Based Complement Alternat Med. 2011;2011:142913.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of 2 Types of Self-administered Acupressure for Persistent Cancer-related Fatigue in Breast Cancer Survivors. JAMA Oncol. 2016;2:1470-6.
- [CrossRef] [PubMed] [Google Scholar]
- The management of Cancer-related Fatigue after Chemotherapy with Acupuncture and Acupressure: A Randomised Controlled Trial. Complement Ther Med. 2007;15:228-37.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Acupressure on Fatigue of Lung cancer Patients Undergoing Chemotherapy: An Experimental Pilot Study. Complement Ther Med. 2014;22:581-91.
- [CrossRef] [PubMed] [Google Scholar]
- Pilot Randomized Controlled Trial of Auricular Point Acupressure to Manage Symptom Clusters of Pain, Fatigue, and Disturbed Sleep in Breast Cancer Patients. Cancer Nurs. 2016;39:402-10.
- [CrossRef] [PubMed] [Google Scholar]
- Management of the Respiratory Distress Symptom Cluster in Lung Cancer: A Randomised Controlled Feasibility Trial. Support Care Cancer. 2015;23:3373-84.
- [CrossRef] [PubMed] [Google Scholar]
- Acupressure for Cancer-Related Fatigue in Elderly Cancer Patients: A Randomized Controlled Study. Altern Ther Health Med. 2023;29:57-65.
- [Google Scholar]
- Effect of Therapeutic Care for Treating Fatigue in Patients with Breast Cancer Receiving Chemotherapy. Medicine (Baltimore). 2017;96:e7750.
- [CrossRef] [PubMed] [Google Scholar]
- Patient-Centred, Self-Administered Acupressure for Chinese Advanced Cancer Patients Experiencing Fatigue and Co-occurring Symptoms: A Pilot Randomised Controlled Trial. Eur J Cancer Care (Engl). 2022;31:e13314.
- [CrossRef] [PubMed] [Google Scholar]
- Acupuncture and Related Therapies for Symptom Management in Palliative Cancer Care: Systematic Review and Meta-analysis. Medicine (Baltimore). 2016;95:e2901.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Acupuncture and Acupressure on Cancer-related Fatigue: A Systematic Review. Oncol Nurs Forum. 2014;41:581-92.
- [CrossRef] [PubMed] [Google Scholar]
- The Effect of Acupressure on Relieving Cancer-related Fatigue: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Cancer Nurs. 2021;44:E578-88.
- [CrossRef] [PubMed] [Google Scholar]






