Translate this page into:
The Influence of Demographic and Psychosocial Factors on the Intensity of pain Among Chronic Patients Receiving Home-based Nursing Care
Address for correspondence: Dr. Thomas Antony Thaniyath; E.mail: thaniyan1@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
To determine the influence of the demographic and the psychosocial factors on the intensity of pain manifestation among the chronic ill patients.
Materials and Methods:
A descriptive, cross-sectional study was carried out among 328 chronic patients under home-based nursing care in Southern State of Kerala, India, from July to August 2015. Each patient was interviewed during a scheduled home visit by a trained health professional. The translated version of the assessment tool questionnaire Medical Outcome Study-Short Form Health Survey was used for the data collection.
Results:
Sixty-four (19.5%) out of 328 patients reported pain as one of the primary symptoms of their disease. The percentage of the patients who were suffering from pain increases with the improvements in both the educational level and the monthly income (P = 0.002 and 0.019, respectively). The social interaction with the relatives and other community members was significantly related to pain manifestation (P = 0.013). A higher degree of social interaction was associated with lower pain intensity (P = 0.019).
Conclusion:
The results of this study showed that certain demographic and psychosocial factors carry a significant level of influence on the pain manifestation and its intensity among the chronic patients. Hence, improvements in education, economic status, and psychosocial support should be considered for the management of the chronic patients.
Keywords
Chronic patients
Demographic factors
Home-based health care
Pain
Social factors
INTRODUCTION
Chronic pain affects the personal daily activities and interferes with the physical and mental wellbeing. A positive psychology has an integral part in the management of chronic pain.[1] On the other hand, factors such as negative affect, anxiety, depression, and focusing attention on pain can exacerbate the pain perception.[2] Previous studies have shown that certain psychological factors such as illness behavior and mental distress are significant predictors of pain persistence following trauma or surgery.[3] The social support, extended to these patients, plays a buffering mechanism and sustains the emotional and physical stability in a crisis. At the same time, reduced or lack of social support (i.e. social isolation) affects negatively the coping up mechanism with illness and causes failure to adapt the chronic illness.[4] Social isolation is independently associated with lower levels of self-rated physical health.[5] Therefore, with optimal social interactions, individuals can lead a healthy life. It is worth noting that the economic burden of palliative care in the countries that lack reliable health insurance systems causes severe limitation in the availability of pain-relieving medications, especially the opioids.[6] This indicates the importance of the economic class of the patient and its influence on the management plan and the compliance to the medical treatment. However, the financial problem can be resolved with proper assessment and utilization of resources by the health professionals and, in some cases, by assistance from relatives, neighbors, or other members of the society.
Considering all these factors, we conducted this study to determine the influence of demographic as well as psychosocial factors on the intensity of pain manifestation in patients under home-based palliative nursing care in Kerala, India.
MATERIALS AND METHODS
Setting and sample
A qualitative survey analysis was carried out among a group of patients registered for home care service under the supervision of the Pain and Palliative Care Department at the General Hospital, Kochi, Kerala, India. Inclusion criteria were a home bound chronic disease patient and aged above 18-year-old. Exclusion criteria were unconscious, uncooperative, or noncognitive patient and a patient with known HIV, HBV infection, or other contagious illness. Based on statistical calculation to attain 95% confidence interval and 0.8 power of the study, the minimum sample size was estimated as 300 patients. Considering human and technical errors, we added 10% to the statistics mentioned above to get a final sample size of 330.
Data collection
A total of 330 patients were approached. Each patient was interviewed during a scheduled home visit by a health professional from July to August 2015. The health care professional is a staff member of the Pain and Palliative Department of the General Hospital, Kochi, Kerala, and he is specialized in palliative care. He was provided with a printed questionnaire for the collection of information on patients’ demographics and social variables (emotional support, tangible support, affection, and social interaction), the cause of disability, presence of pain, and estimation of the pain intensity. These variables were measured using the assessment tool: Medical Outcome Study (MOS)-Short Form Health Survey that is translated into the local language, Malayalam. The validity and reliability of MOS-Short Form Health Survey for its use in India recently were established by Arokiasamy et al. in 2013.[7]
Statistical analysis
The data were analyzed using the Statistical Package for Social Sciences version 20 (SPSS Inc., Chicago, IL, USA). The Chi-square test was used to test distribution of categorical variables. Statistical significance was accepted when P < 0.05.
Ethical considerations
The study protocol was evaluated and approved by the Institutional Ethical Committee of St. Gregorios Dental College and the Research Center, Kothamangalam, under Kerala University of Health and Allied Sciences, India. Consents were obtained from the patients before participation in the study.
RESULTS
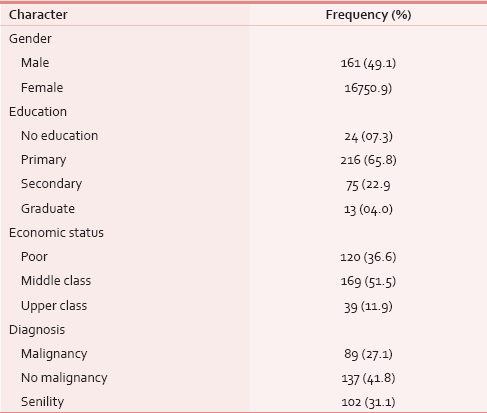
A total of 330 chronic ill patients were approached. The data of two patients were excluded from the study due to incomplete information in the survey form, and the data of 328 patients were included for analysis. Table 1 presents the demographic characters of the participants. Male to female ratio was almost 1:1 and the mean age (standard deviation) of the participants was 64.1 (17.4) years old. The major causes of disability were malignancy (27%), nonmalignant chronic medical problems (42%), and senility (31%).
The study showed a significant relation between pain and level of education, income, and causes of disability [Table 2]. The percentage of patients who were suffering from pain increased with the level of education from 8% in the illiterates to 19% in the partially educated and then 46% in the university graduates (P = 0.002). Similarly, the prevalence of pain as primary symptom increased with the rate of the monthly income from 12% in those with poor income to 23% and 28% among those who had moderate and high monthly income, respectively (P = 0.019). The patients who suffered from malignancy had a significantly higher frequency of pain than those who suffered from chronic nonmalignant medical conditions (14%) or those who had an age-related disability (8%) (P < 0.001).

Table 3 shows a significant effect of the social interaction with the occurrence of pain and insignificant relations between the frequency of pain sensation and the degree of emotional support, tangible support, or affection (P > 0.05). The percentage of patients who had pain was greater among those who received a high degree of social interaction compared to those who received moderate or low interaction (P = 0.013).

Sixty-four out of 328 patients (19.51%) showed pain as a primary symptom of their disease. Statistical analysis for the relation between pain intensity and psychosocial factors for this subgroup of patients showed that a higher degree of social interaction is associated with lower pain intensity (P = 0.019). Other factors such as emotions, tangible support, and affection showed a little relation with the pain intensity [Table 4].

DISCUSSION AND CONCLUSION
The association of the socioeconomic factors and the extent of the psychosocial support with disease manifestations was described in the work of Link and Phelan in 1995.[8] They argued that the social factors are “fundamental causes” of disease that affect multiple disease outcomes through multiple mechanisms, and therefore, they maintain an association with disease in different situations. In this study, we have investigated the relationship between the demographic and the psychosocial components with pain manifestation and its intensity as it is considered as the fifth vital sign.[9] Recently, it has been identified that the social isolation (loneliness) is an important risk factor for disease manifestation in the chronic ill patients.[10] This indicates the importance of the social interaction for general health and well-being. However, we found that patients who received a higher degree of social interaction had a higher frequency of pain complaints when compared to those who received lower interaction. A possible explanation could be the fact that the social visits and the active interaction with the relatives and the community offer a chance for the chronic ill patients to talk about their disease and to express the symptoms that may draw attention, like pain. Our finding that the higher level of social interaction was associated with reduced pain intensity supports this explanation. It is well known that the home-based patients have more interpersonal interactions with the family members and the society than the hospitalized patients.
In this qualitative analysis, we found a significant relation between the frequency of pain sensation and the levels of both education and income of the patients. The percentage of pain manifestation rises with the increasing level of educational attainment as well as the amount of the monthly income. This might be due to increased orientation about the health care seeking attitude in this group of patients. It is suggestible that a high degree of education (or economic status) improves the extent of health care attention. A previous work of the authors suggests that an improvement in these demographic factors was associated with a higher degree of healthy social interaction.[11]
The major limitation of this study was the recall bias and the lack of a locally developed tool for assessment of the social factors based on the local culture of the community. An additional limitation is the subjective estimation of the pain intensity. However, our results showed a significant effect of demographic factors, such as education, income status, and psychosocial support, on the incidence of pain and its intensity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Factors affecting the psychological functioning of Australian adults with chronic pain. Nurs Health Sci. 2012;14:508-13.
- [Google Scholar]
- Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain. 2006;123:146-54.
- [Google Scholar]
- Factors affecting self-efficacy and pain intensity in patients with chronic musculoskeletal pain seen in a specialist rheumatology pain clinic. Rheumatology (Oxford). 2008;47:1803-8.
- [Google Scholar]
- Social Isolation: The Association between Low Life Satisfaction and Social Connectivity. In: Presented at WOCN Society 41st Annual Conference. St. Louis, USA, 6-10 June, 2009.
- [Google Scholar]
- Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50:31-48.
- [Google Scholar]
- Palliative care in India: Successes and limitations. J Pain Palliat Care Pharmacother. 2003;17:121-8.
- [Google Scholar]
- Validity and reliability of MOS short form health survey (SF-36) for use in India. Indian J Community Med. 2013;38:22-6.
- [Google Scholar]
- Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No:80-94.
- [Google Scholar]
- The influence of demographic factors on social affections among chronic patients under home based nursing care. Asian Acad Res J Soc Sci Humanit. 2015;2:166-75.
- [Google Scholar]






