Translate this page into:
The Mapping of Influencing Factors in the Decision-Making of End-of-Life Care Patients: A Systematic Scoping Review
*Corresponding author: Mauricio de Almeida Pereira da Silva, Bioethics Graduate Program, Pontifícia Universidade Católica do Paraná, Curitiba, Paraná, Brazil. msilvamintensiva@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Silva MA, Corradi-Perini C. The mapping of influencing factors in the decision-making of end-of-life care patients: A systematic scoping review. Indian J Palliat Care 2023;29:234-42.
Abstract
Decisions in end-of-life care are influenced by several factors, many of which are not identified by the decision maker. These influencing factors modify important decisions in this scenario, such as in decisions to adapt to therapeutic support. This presented scoping review aims to map the factors that influence end-of-life care decisions for adult and older adult patients, by a scoping review. The review was carried out in 19 databases, with the keyword ‘clinical decision-making’ AND ‘terminal care’ OR ‘end-of-life care’ and its analogues, including publications from 2017 to 2022. The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews. The search resulted in 3474 publications, where the presence of influencing factors in end-of-life decision-making for adults and the elderly was applied as a selection criterion. Fifty-four (54) of them were selected, which means 1.5% of all the results. Among the selected publications, 89 influencing factors were found, distributed in 54 (60.6%) factors related to the health team, 18 (20.2%) to patients, 10 (11.2%) related to family or surrogates and 7 (7.8%) factors related to the decision environment. In conclusion, we note that the decision-making in end-of-life care is complex, mainly because there is an interaction of different characters (health team, patient, family, or surrogates) with a plurality of influencing factors, associated with an environment of uncertainty and that result in a critical outcome, with a great repercussion for the end of life, making it imperative the recognition of these factors for more competent and safe decision-making.
Keywords
Palliative care
End-of-life care
Terminal care
Clinical decision-making
Withholding treatment
INTRODUCTION
End-of-life decisions are complex. They involve an interaction between the health team, patients, family members, or surrogates in a dynamic emotional environment, characterised by uncertainties.[1]
A decision is considered appropriate when we make it autonomously. For this to happen, three components must be present in this decision-making process: The intention, the understanding, and the absence of control over the decision. The intention is related to the planning which is expressed in the form of representation of the series of events proposed for the execution of the action.[2] The understanding involves learning a substantial amount of propositions and statements that describe the nature of the action, its foreseeable consequences, and possible outcomes.[3] Finally, the absence of internal and external controls may coerce the final decision. These controls influence unrestrained resistance and self-management capacities of the individual’s own desires.[2]
Different factors influence these components of an autonomous decision. Scientific evidence shows that health professionals are influenced during the decision-making process[4] in different areas of health care.[5] End-of-life care decisions have a more challenging characteristic because they are made in a critical environment, with multifaceted uncertainties and technical and ethical repercussions of great importance.[6] In this sense, the scoping review aims at mapping the influencing factors of end-of-life care decisions of adult and older adult patients.
METHODOLOGY
The methodology of this scoping review was developed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist for scoping reviews.[7] The population, concept and context strategy[8] was used for the elaboration of the research question, where the population is the decision-maker in matters related to health; the concept is the influencing factor of the decision-making, and; the context is end-of-life adult and elderly patient. Thus, the guiding question was raised, ‘What are the factors that influence the clinical decision-making of adult and elderly patients at the end of life?’
The search was carried out from January to April 2022; therefore, the following indexed keywords were searched: ‘Clinical decision-making’ associated with ‘terminal care’ OR ‘end-of-life care,’ in the Portuguese, English and Spanish languages in the following databases: Directory of Open Access Journals, ROAD: Directory of Open Access Scholarly Resources, Medline Complete, Wiley-Blackwell Full Collection 2013, BioMedCentral Open Access, Academic Search Premier, HighWire Press, HighWire Press (Free Journals), Sage Premier Journal Collection, CINAHL, SAGE Premier 2007, Freedom Collection Journals [SCFCJ], Single Journals, BMJ Journals, Freely Accessible Journals, Journals@Ovid Nursing Excellence and Quality Extended Journal Collection, MAG Online Library Internurse, Project MUSE - Premium Collection, Library, Information Science and Technology Abstracts, Oxford Journals Current Collection, restricted to peer review and to the period from 1 January, 2017, to 1 April, 2022, covering the past 5 years.
It was used, as an eligibility criterion, the presence of influencing factors citations in decision-making about adult and elderly patients in an end-of-life decision environment. The variables extracted from the articles were the objectives, type of research, population studied, data collection location (country) and also, information about the influencing factors mentioned and the parts involved evaluated (health team, patient, family members or surrogates, and the decision environment). The content-analysis method[9] was used to extract the influencing factors.
RESULTS
It was found 3.474 publications, which after the process of duplication elimination resulted in 1.355 articles. Out of these remaining articles, 1.199 publications in the title evaluation phase, 89 publications in the summary phase, and 13 fully completed publications were excluded from the study. Only articles that referred to influencing factors in the decision-making of end-of-life care of adult and elderly patients were included, totaling 54 publications (1.5%) used in the composition of the scoping review [Figure 1].
![PRISMA[7] flow diagram. PRISMA: Preferred Reporting Items for Systematic reviews and Meta-Analyses.](/content/137/2023/29/3/img/IJPC-29-234-g001.png)
- PRISMA[7] flow diagram. PRISMA: Preferred Reporting Items for Systematic reviews and Meta-Analyses.
Among the 54 publications included, 61% show qualitative methodologies, 31% quantitative, and 8% with mixed methodologies. With an average article checklist quality rating of 91%. Consisting of averages of 91% and 90% in qualitative and quantitative publications, respectively, according to QualSyst qualifications.[10,11] The included studies have a global distribution, including North America, Europe, and eastern countries such as Japan, Taiwan, Australia, Singapore, China, and Pakistan.
The publication sample shows 57% of the influencing factors related to health teams, 24% to patient factors, 2% to influencing family or surrogates, and 15% to a mixed population, totaling 302 influencing factors identified in this scoping review, as follows in [Tables 1 and 2].[12-65]
| Author | Year | Methodology | Qualsyst[10,11] | Perspective | Influencing factors |
|---|---|---|---|---|---|
| Abdullah et al.[12] | 2020 | Mixed | - | Patient; Family | 8 |
| Bandini et al.[13] | 2017 | Quantitative | 100% | Patient | 1 |
| Batteux et al.[14] | 2020 | Mixed | - | Patient | 5 |
| Bopp et al.[15] | 2018 | Quantitative | 100% | Health team | 8 |
| Cristina et al.[16] | 2017 | Quantitative | 71% | Health team | 5 |
| Dahmen et al.[17] | 2017 | Quantitative | 89% | Health team | 2 |
| Daly et al.[18] | 2018 | Quantitative | 71% | Mixed | 2 |
| Derry et al.[19] | 2019 | Qualitative | 75% | Patient | 1 |
| Dionne-Odom et al.[20] | 2019 | Qualitative | 100% | Patient | 7 |
| Duivenbode et al.[21] | 2019 | Quantitative | 100% | Health team | 6 |
| Dzeng et al.[22] | 2018 | Qualitative | 95% | Mixed | 9 |
| Escher et al.[23] | 2021 | Qualitative | 95% | Health team | 11 |
| Fischhoff et al.[24] | 2019 | Qualitative | 65% | Patient | 3 |
| Frush et al.[25] | 2018 | Qualitative | 93% | Health team | 3 |
| Geddis-Regan et al.[26] | 2021 | Qualitative | 100% | Health team | 3 |
| Gerber et al.[27] | 2021 | Qualitative | 100% | Patient | 1 |
| Glatzer et al.[28] | 2020 | Qualitative | 70% | Health team | 33 |
| Graham[29] | 2020 | Qualitative | 80% | Health team | 3 |
| Higginbotham et al.[30] | 2021 | Qualitative | 100% | Mixed | 4 |
| Jacquier et al.[31] | 2021 | Qualitative | 100% | Health team | 8 |
| Janssens et al.[32] | 2018 | Qualitative | 60% | Health team | 4 |
| Kim et al.[33] | 2017 | Quantitative | 82% | Health team | 3 |
| Author | Year | Methodology | Qualsyst[10,11] | Perspective | Influencing factors |
|---|---|---|---|---|---|
| King et al.[34] | 2018 | Qualitative | 100% | Patient | 6 |
| Lamahewa et al.[35] | 2018 | Qualitative | 100% | Mixed | 4 |
| Laryionava et al.[36] | 2021 | Qualitative | 100% | Health team | 6 |
| Latcha[37] | 2019 | Qualitative | 70% | Health team | 2 |
| Lee[38] | 2020 | Qualitative | 90% | Patient | 1 |
| Leibold et al.[39] | 2018 | Qualitative | 100% | Health team | 2 |
| Lesieur et al.[40] | 2018 | Quantitative | 100% | Health team | 1 |
| Lin et al.[41] | 2019 | Quantitative | 79% | Health team | 4 |
| Lin et al.[42] | 2019 | Qualitative | 100% | Mixed | 13 |
| Lobo et al.[43] | 2017 | Quantitative | 100% | Health team | 6 |
| Ludlow et al.[44] | 2021 | Qualitative | 100% | Health team | 7 |
| Mitropoulos et al.[45] | 2019 | Quantitative | 89% | Health team | 2 |
| Ntantana et al.[46] | 2017 | Quantitative | 93% | Health team | 4 |
| Orlovic et al.[47] | 2021 | Qualitative | 100% | Patient | 8 |
| Radhakrishnan et al.[48] | 2017 | Qualitative | 95% | Health team | 6 |
| Rego et al.[49] | 2020 | Mixed | - | Health team | 2 |
| Robijn et al.[50] | 2018 | Qualitative | 100% | Mixed | 2 |
| Robijn et al.[51] | 2020 | Qualitative | 95% | Health team | 5 |
| Sanders et al.[52] | 2019 | Quantitative | 89% | Patient | 4 |
| Scholten et al.[53] | 2018 | Mixed | - | Mixed | 6 |
| Siddiqui et al.[54] | 2018 | Qualitative | 70% | Health team | 1 |
| Simon et al.[55] | 2017 | Qualitative | 75% | Health team | 3 |
| Stalnikowicz et al.[56] | 2020 | Qualitative | 80% | Health team | 6 |
| Subramaniam et al.[57] | 2021 | Quantitative | 100% | Patient | 1 |
| Syed et al.[58] | 2017 | Quantitative | 93% | Health team | 9 |
| Tanaka et al.[59] | 2021 | Qualitative | 100% | Relatives | 6 |
| Taylor et al.[60] | 2017 | Qualitative | 100% | Health team | 9 |
| Van Heerden et al.[61] | 2020 | Qualitative | 75% | Health team | 2 |
| Vanderhaeghen et al.[62] | 2019 | Qualitative | 100% | Health team | 10 |
| Walzl et al.[63] | 2019 | Qualitative | 100% | Mixed | 23 |
| Wen et al.[64] | 2019 | Quantitative | 89% | Patient | 5 |
| Wu et al.[65] | 2020 | Qualitative | 100% | Patient | 6 |
After coding the factors, uniting the factors with the same meaning and categorising them into groups regarding the parts involved (health team, patient, family or surrogates, and decision environment) and also regarding the fields of influence (biological, values and quality of life or context to the decision) according to Jonsen et al.,[66] 89 influencing factors were defined, with the results shown in [Table 3].
| Parts involved | Fields of influence | Total | ||
|---|---|---|---|---|
| Biological | Values and quality of life | Decision context | ||
| Health team | 25 | 18 | 11 | 54 |
| Patient | 7 | 7 | 4 | 18 |
| Family and surrogates | 1 | 6 | 3 | 10 |
| Decision environment | 1 | 1 | 5 | 7 |
| 89 | ||||
The influencing factors are presented in a mosaic of factors [Figures 2 and 3], according to the involved individual and his/her category of the field of influence.
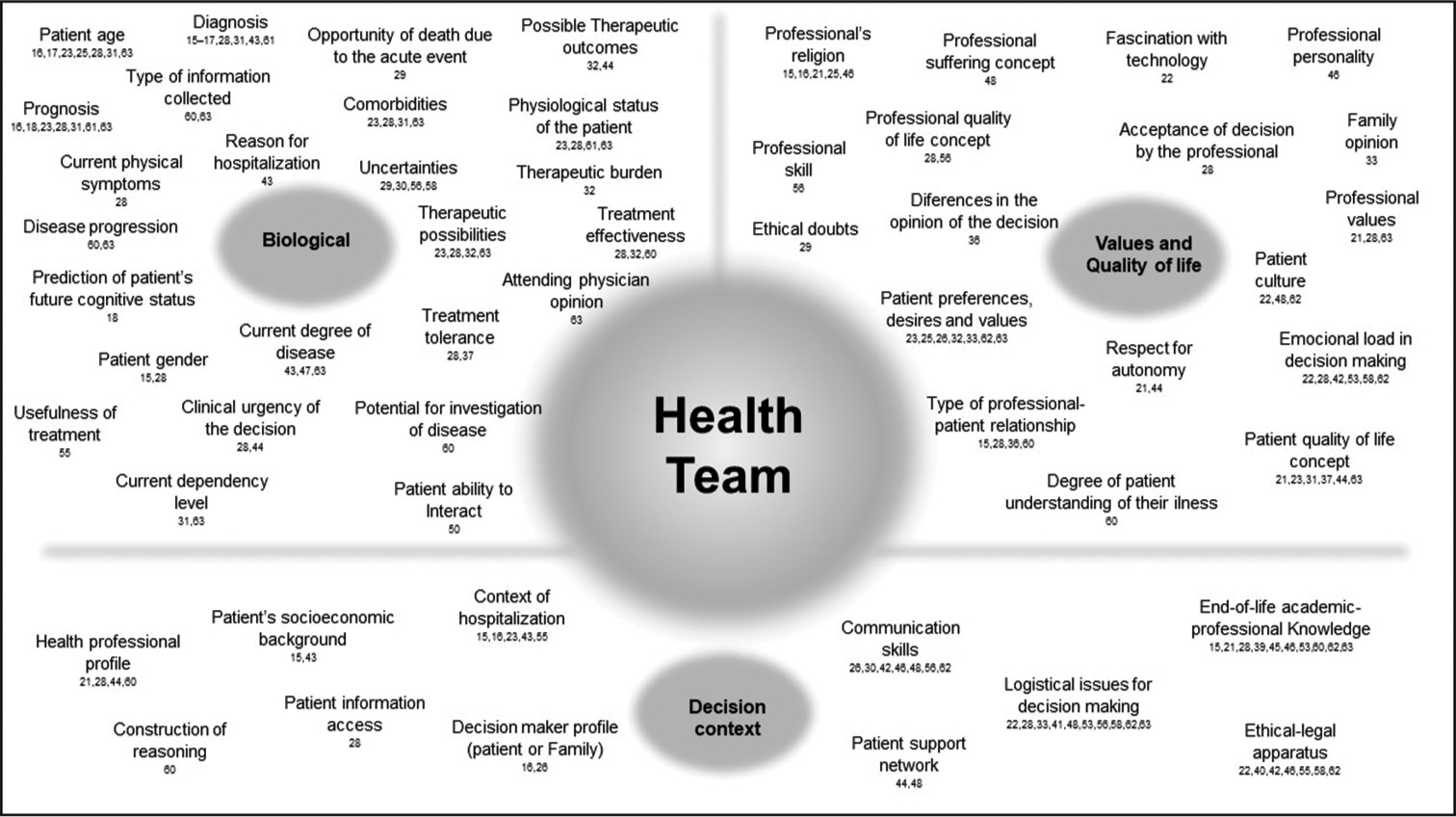
- Influencing factors mosaic for health team.
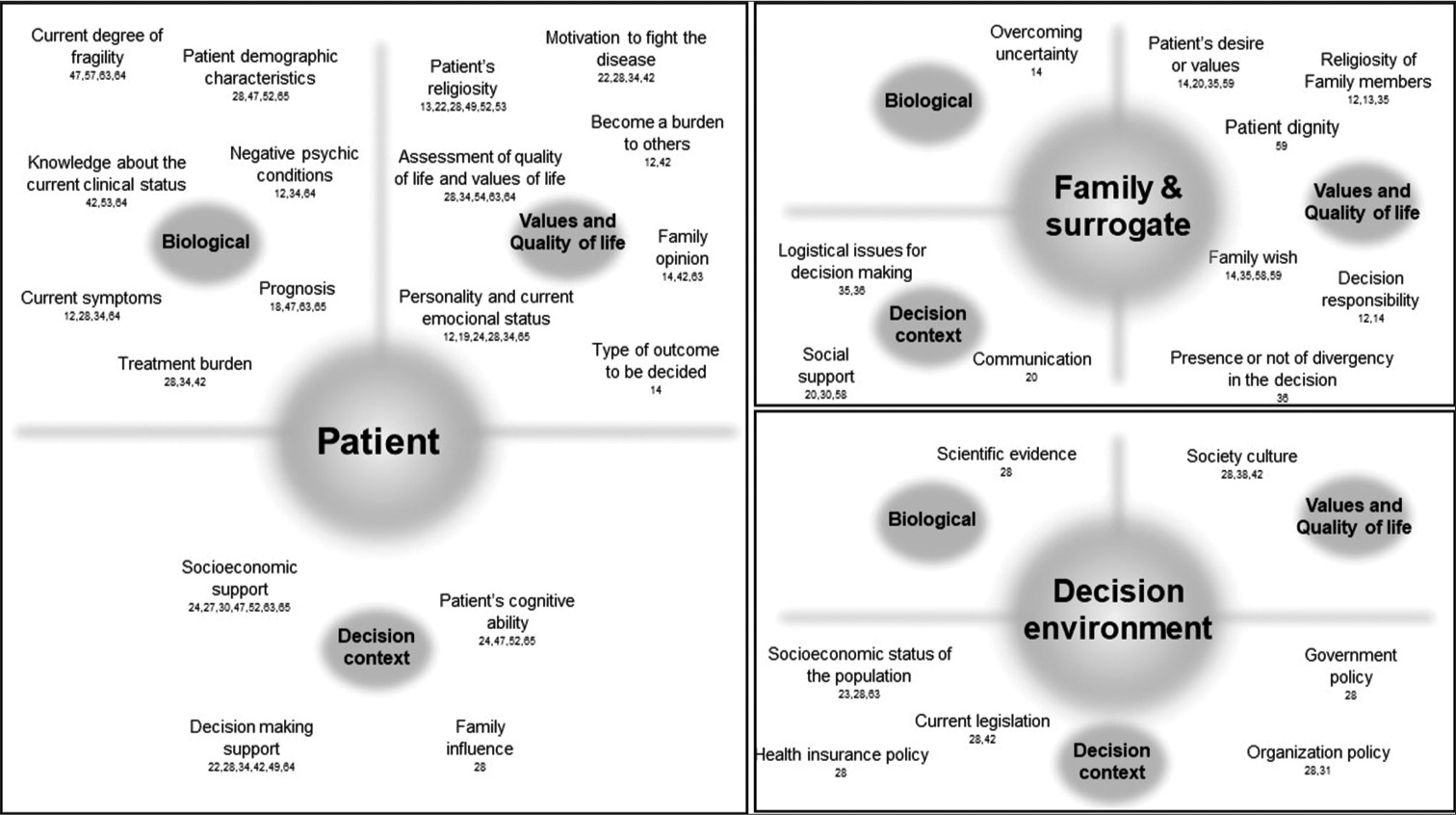
- Influencing factors mosaic for patient, family, surrogate and decision environment.
The factors found in the health team are the most prevalent in the studied literature. These factors are related to the technical aspects of the end-of-life decision, such as the characteristics of the disease, the patient’s clinical status, therapeutic options, and prognoses, but also subjective and individual factors from the health professional, which include ethical, cultural and relationship values between the professional and the patient. Several influencing factors of the decision context were also found. The logistics, knowledge of the subject and communication skills in decision-making were highlighted as factors often cited.
For the patients, the influencing factors are related to the patient’s current clinical condition, the prediction of prognosis, and several factors related to personal values and quality of life. There are also cultural influences on end-of-life concepts, demonstrated through religious influence and dynamics of coping with the disease.
When the decision becomes the responsibility of family members or surrogates factors are alluding to the zeal in the decision, seeking greater certainty, consensus, and shared decisions, which allows for a dilution of responsibility when deciding for third parties.
Finally, all these decisions are made in an environment with a specific influencing factor, such as the society’s culture and the current knowledge of medicine and policies involving the topic are constant influencers of choices.
All these influencing factors are responsible for the final decision-making, where the role of each influencing factor is modified according to the scenario involved.
DISCUSSION
End-of-life decisions are essential processes in end-of-life care. This care is built through a relationship between health professionals, the patient, and their surroundings (family members, surrogates, and environment). Regardless of the relationship model adopted, whether paternalistic, sovereign autonomy (informative model), interpretive or deliberative model,[67] there is a need for participation from the health team, patient, environment, and often the family or a designated surrogate.
The interaction of these participants, influenced by their judgments and values, associated with the search for the patient’s best interests, makes end-of-life decision-making a complex procedure.[6] This complexity can be demonstrated by the wide number of found factors that influence decision-making in this environment.
Of the 89 influencing factors found in our scoping review, more than half are health team influencers, possibly reflecting the search in scientific publications in the health area. These factors were categorised according to the fields of influence, as organised by Jonsen et al.,[66], and also to the biological, values, and quality of life and decision context fields of influence. The discussion will present the influencing factors broken down according to the parts involved, subdividing them into the fields of influence.
Health team
We found 54 influencing factors that referred to health team professionals. Initially, we verified factors associated with the patient’s profile, which includes age,[16,17,23,25,28,31,63] gender,[15,28] comorbidities,[23,28,31,63] physiological status,[23,28,61,63] the patient’s degree of dependence,[31,63] the patient’s ability to interact[50] and the current physical symptoms[28] that the patient is experiencing. The reason for hospitalisation,[43] the type of information that the health professional collected,[60,63] the opinion from assistant physicians who already know the patient[63] and the degree of urgency of this decision-making[28,44] are the elements that build an initial picture of which patient is being approached.
In similar reviews, some of these factors influenced up to 83% (comorbidity) of medical decisions in an emergency setting.[68]
Factors related to the disease, such as diagnosis,[15-17,28,31,43,61] prognosis,[16,18,23,28,31,61,63] current degree of the disease,[43,47,63] the potential for the investigation of the disease[60] and the type of disease progression[60,63] are widely cited. Of these, one of the most frequent factors was the assessment of prognosis, which represents a challenge in many areas of health. Mainly because there is a lot of uncertainty in the estimates.[29] This uncertainty appears as an influencing factor in the review.[29,30,56,58] It also influences the concept of therapeutic futility, since therapeutic futility is a decision based on prognostic estimates, which are subject to uncertainties,[55,63] associated with severe ethical consequences.[69]
The pace of disease progression[60,63] influences decision-making. Different profiles of disease evolution create different expectations and challenges in end-of-life care, requiring changes in approaches and points of concern in care.[70]
Influencing factors related to therapeutic options were also found, such as the possibilities,[23,28,32,63] effectiveness[28,32,60] and usefulness of treatments,[55] as well as the capacity for tolerance[28,37] and the burden[32] that the intervention will result in.
The expectation of therapeutic outcomes[32,44] and the clinical condition after treatment, such as the prediction of the patient’s future cognitive status,[18] must be adjusted to the inherent uncertainties of this information. In addition, the possible loss of the opportunity of death due to the acute phase of the disease must be considered. This concept defends the idea that there is a ‘window of opportunity’ in the acute phase of the event where the patient is physiologically unstable and the withholding or withdrawing therapies at this moment would result in his death, avoiding a progression to a chronic pathological condition, with an indefinite period, which would generate more suffering for the patient.[29]
As far as values go, we found an inconsistency between the health team’s values and the values of the patients, family, or surrogates. This inconsistency is expressed by the influencing factors of the professional’s religion,[15,16,21,25,46] his personal values,[21,28,63] his concepts of suffering[48] and quality of life,[28,56] his feelings of discomfort in the face of death and professional failure,[42,58] in addition to the professional’s personality[46] and respect for the patient’s autonomy.[21,44] On the other hand, there is a need for appreciation of the wishes of the patients or their surrogates,[23,25,26,32,33,62,63] characterized here as valuing the patient’s culture[22,48,62] and their concept of quality of life.[21,23,31,37,44,63]
This inconsistency is balanced through the dynamics of the relationship between professionals and patients or surrogates.[15,28,36,60] This relationship is full of influencing factors, such as the professional’s ability to listen,[56] his emotional charge in this scenario[22,28,42,53,58,62] and whether or not there are differences between the opinions of those involved,[36] which often puts to the test the acceptance of the final decision of the deliberation,[28] influencing the dynamics of the decision.
In relationships that adopt a shared decision model, healthcare professionals and patients or family members work together to reach a mutual consensus on the best course of action. This consensus should include two sources of knowledge, the health professional with technical knowledge and the patient and family nucleus with knowledge of values and preferences, both with equal importance in the final decision.[71] This deliberation should not allow the imposition of values, but a bond in which the final benefit will be achieved based on trust between the parties and the concept of the broader patient’s good, emphasised by Pellegrino and Thomasma.[72] These mentioned authors describe that beneficence is not restricted to the biomedical (technical) good, possibly influenced by a fascination with technology by professionals.[22] Decision-making in this model seeks an integral vision, which includes the values of the patient as a human being with the ability to choose, with individual desires for the specific imposed situation, and with transcendental values, expressed through an ultimate, non-negotiable desire.[72]
Deliberations for decision-making must have prudence as a principle, which seeks an opening in dialogue, with the permission of the intellectual approximation of those involved. Recognising that everyone has something to teach, with the possibility of opening new perspectives capable of making changes, revisions, enrichments, or additions of their points of view.[73] In this deliberating environment, influencing factors of ethical doubts,[29] the family member’s opinions[33], and the patient’s or surrogates’ degree of ability to understand the disease[60] are dealt with.
In the decision context, a frequently mentioned theme was the lack of time available for the end-of-life approach. This research showed it through the mentioning work overload of the health team and the need to reevaluate the policies of relationship followed by the health team when approaching patients.[22,41] This same theme was mentioning by other logistical issues, such as the structure and the need for administrative tools to facilitate this approach.[22,28,33,41,48,53,56,58,62,63]
The technical training of health professionals in the area of end-of-life care,[15,21,28,39,45,46,53,60,62,63] which includes experience in this area of expertise, technical knowledge of symptom control and the knowledge of the ethical-legal aspect of the proposed conduct,[39,62] appears as a negative influence on decision-making due to a deficit in this learning, which shows a fragility in the formation and dissemination of this theme, especially in the practical aspect. The communication skill[26,30,42,46,48,56,62] mainly mentioned in relation to the training in this type of scenario is a strong influencing factor in decision-making.
Other factors of a more pragmatic aspect permeate the decision context, such as the availability of access to patient information,[28] the characteristics of hospitalisation,[15,16,23,43,55] in addition to the profiles of the professional[21,28,44,60] in relation to their responsibility for this decision-making and the decision-maker’s profile, whether he is choosing for himself or a third party (Surrogate).[16,26]
The decision is also made up of surrounding components, which include the support network for practical assistance in the care process[44,48] and the patient’s socioeconomic context,[15,43] indirectly reflecting the help capacity that this patient will be able to find.
Finally, the way in which the reasoning[60] is constructed for this decision-making generates a difference in the choices. The formation of analytical, critical, and more rational reasoning is different from intuitive, spontaneous, and emotion-loaded decisions, which generate more insecurity or biases, especially in the past form of decisions.[74] Intuitive and quick reasoning, commonly observed in clinical routine,[4] uses mental shortcuts for faster conclusions. However, these shortcuts or, also known as heuristics, make reasoning more susceptible to failure.[75] Failures in this reasoning construction process result in heterogeneity of decisions, making them imprecise and unreliable.[76]
Patients
The patients were the second most referenced group in the studies listed in this scoping review, which represents about a quarter of the articles. Despite appearing in second place in terms of frequency of influencing factors, this character is considered to be the most important in decision-making, with the patient’s wishes, advance directives of will, or discussion about autonomy always being mentioned in other topics.
As an influencer in the decision of their end-of-life care, personal characteristics such as age, ethnicity and gender are often cited, which demonstrates that experiences, cultures and the way, in which they deal with life are factors that strongly influence the decision.[28,47,52,65]
On the other hand, the aspects of the disease are also important for the choice of options, especially for the prognosis,[18,47,63,65] including the severity of the clinical condition,[65] its reversibility and the remaining lifetime.[47] In this aspect, disease development[63] is a decision-modifying factor, influencing in a different way depending on the context experienced at the time. Diseases show different ways of reaching the outcome of death and in each subtype of clinical evolution, there are different challenges in the care.[77] The condition of this disease progression brings several influencing factors, such as physical, psychological,[12,34,64] social and spiritual symptoms[12,28,34,64] and the degree of functionality or independence at the time of the decision[47,57,63,64] as elements of this decision-making. The expectation of suffering in the end-of-life process is demonstrated by citing the burden of the treatment,[28,34,42] something that indirectly expresses other influencing factors in the field of values and quality of life.
The patient’s desires,[28,34,54,63,64] cited in several studies on influencing factors, demonstrate their importance in the patient’s decision-making. These values and concept of quality of life are built through the patient’s profile, such as his personality traits (introverted or extroverted)[12,19,24,28,34,65] and his profile of coping with challenges[22,28,34,42] being able to delegate or assume decisions, associated with his cultural acceptance of death,[22,28,34,42] closely linked to his spirituality, presenting themselves in a positive or negative light on the influence of the decision.[13,22,28,49,52,53]
Other external factors influence these values, such as the workload brought by the disease to the patient’s caregivers and the burden imposed on society,[12,42] which can modify the convictions of the choices presented, especially when the decision-making involves the possibility of an outcome of cognitive after-effect and not just the risk of death.[14] Therefore, the family members’ opinion becomes one of the influencing factors for the patient’s decision.[14,42,63]
As far as the burden of the treatment goes, the patient’s socioeconomic capacity and degree of social and financial support to meet the required care are factors of strong influence on patients.[24,27,30,47,52,63,65] However, the support also involves the patient’s relationship with the health team and family members who accompany him, expressed through the trust of this interaction, availability, and freedom to share doubts, feelings, and uncertainties.[22,28,34,42,49,64]
All these factors are moderated by the patient’s ability to understand the situation,[42,53,64] influenced by his cognitive ability and degree of desire for complete knowledge of the clinical condition.
Family and surrogates
End-of-life care and palliative care have as their guiding principle, the inclusion of family members and loved ones as an integrated part of the process.[78] Therefore, the analysis of influencing factors of family members and surrogates is of paramount importance, especially when we are talking about situations in which this component is the decision maker himself, either because the patient is no longer able to express his wishes or in cases of a designation by the patient through advance directives of will.[79]
This review shows that one of the concerns of family members and surrogates as an influencing factor of the decision is overcoming uncertainty about the best decision that the patient would want.[14] It is not always easy to express the wishes for all possible scenarios and it is necessary for the family member or surrogate to decide, even if they are not completely certain. To perform this task, the family member or surrogate takes into account the wishes previously expressed by the patient,[14,20,35,59] but also uses his values and concepts,[14,35,58,59] his spirituality and his concepts of death and end of life,[12,13,35] associated with the moral quality of dignity.[59] The presence of choice divergences[36] as a decision-modifying factor shows that decisions for third parties involve a high level of responsibility,[12,14] especially when there are diversified risks such as death or physical and cognitive after-effects.
Decisions carried out by family members or surrogates are dependent on social support for the decision maker, but this interaction can also result in conflicts that result in more condescending decisions.[58]
Again, it is noted that the quality of the health team’s relationship with the patient and family members is a strong factor influencing the decision. This aspect is presented through communication skills,[20] respecting the educational level and cognitive capacity of the interlocutors and the degree of trust established in this relationship.[35,36]
Decision environment
The decision environment concerns external influencers to the decision individuals (health staff, patients, family members, or surrogates). This includes the technical development of the health area, with better scientific research on topics related to end-of-life care,[28] the culture of the society in which the decision-making takes place[28,38,42], and the socioeconomic capacity of the country.[23,28,63] It also includes the distribution of the financial resources, mainly the funds destined for the promotion of health in palliative care.[28] The end-of-life care policy of health insurance, with their coverages and incentives, as well as the institutional organisation where the care is being carried out (protocols, support, and guidelines) are strong influencers of the decision.[28,31] It can also be noted that the current legislation on this subject influences the decision-making of all members.[28,42]
In view of the data presented, it appears that this scoping review achieved its initial objective, which is to map the influencing factors in end-of-life decision-making in adults and the elderly. However, it does have some limitations; initially, the review was not carried out by peers, with only one reviewer. Second, this scoping review did not delve into the grey literature, which could broaden the mapping of influencing factors. Finally, there was no clear evidence of saturation of the theme, even considering frequent repetitions of some influencing factors among the studies, with an open field for future complementary research.
CONCLUSION
The mapping of influencing factors can help support endof-life decision-making. The recognition of influences can improve our choices, making them increasingly autonomous and competent. There are many opportunities for future studies in the quantitative and qualitative assessment of the weight of the influence of the different factors listed in the different scenarios and decisions in the health area.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Patient and healthcare professional factors influencing end-of-life decision-making during critical illness: A systematic review. Crit Care Med. 2011;39:1174-89.
- [CrossRef] [PubMed] [Google Scholar]
- Biases and heuristics in decision making and their impact on autonomy. Am J Bioeth. 2016;16:5-15.
- [CrossRef] [PubMed] [Google Scholar]
- Cognitive debiasing 1: Origins of bias and theory of debiasing. BMJ Qual Saf. 2013;22:58-64.
- [CrossRef] [PubMed] [Google Scholar]
- Medicine and heuristics: Cognitive biases and medical decision-making. Ir J Med Sci. 2020;189:1477-84.
- [CrossRef] [PubMed] [Google Scholar]
- Ethical content of expert recommendations for end-of-life decision-making in intensive care units: A systematic review. J Crit Care. 2020;58:10-9.
- [CrossRef] [PubMed] [Google Scholar]
- PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467-73.
- [CrossRef] [PubMed] [Google Scholar]
- Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields (1st ed). Edmonton: Alberta Heritage Foundation for Medical Research; 2020.
- [Google Scholar]
- Influences on care preferences of older people with advanced illness: A systematic review and thematic synthesis. J Am Geriatr Soc. 2018;66:1031-9.
- [CrossRef] [PubMed] [Google Scholar]
- Preferences and experiences of muslim patients and their families in muslim-majority countries for end-of-life care: A systematic review and thematic analysis. J Pain Symptom Manage. 2020;60:1223-38.e4.
- [CrossRef] [PubMed] [Google Scholar]
- The role of religious beliefs in ethics committee consultations for conflict over life-sustaining treatment. J Med Ethics. 2017;43:353-8.
- [CrossRef] [PubMed] [Google Scholar]
- A mixed methods investigation of end-of-life surrogate decisions among older adults. BMC Palliat Care. 2020;19:44.
- [CrossRef] [PubMed] [Google Scholar]
- Physician-related determinants of medical endof-life decisions-a mortality follow-back study in Switzerland. PLoS One. 2018;13:e0203960.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with the decision-making process in palliative sedation therapy. The experience of an Italian hospice struggling with balancing various individual autonomies. Cogent Med. 2017;4:1290307.
- [CrossRef] [Google Scholar]
- Limiting treatment and shortening of life: Data from a cross-sectional survey in Germany on frequencies, determinants and patients' involvement. BMC Palliat Care. 2017;16:3.
- [CrossRef] [PubMed] [Google Scholar]
- Complexity analysis of decision-making in the critically ill. J Intensive Care Med. 2018;33:557-66.
- [CrossRef] [PubMed] [Google Scholar]
- Advanced cancer patients' understanding of prognostic information: Applying insights from psychological research. Cancer Med. 2019;8:4081-8.
- [CrossRef] [PubMed] [Google Scholar]
- How family caregivers of persons with advanced cancer assist with upstream healthcare decision-making: A qualitative study. PLoS One. 2019;14:e0212967.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing relationships between muslim physicians' religiosity and end-of-life health-care attitudes and treatment recommendations: An exploratory national survey. Am J Hosp Palliat Med. 2019;36:780-8.
- [CrossRef] [PubMed] [Google Scholar]
- Homing in on the social: System-level influences on overly aggressive treatments at the end of life. J Pain Symptom Manage. 2018;55:282-9.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Physicians' perspective on potentially non-beneficial treatment when assessing patients with advanced disease for ICU admission: A qualitative study. BMJ Open. 2021;11:e046268.
- [CrossRef] [PubMed] [Google Scholar]
- Value awareness: A new goal for end-of-life decision making. MDM Policy Pract. 2019;4:2381468318817523.
- [CrossRef] [PubMed] [Google Scholar]
- Physician decision-making in the setting of advanced illness: An examination of patient disposition and physician religiousness. J Pain Symptom Manage. 2018;55:906-12.
- [CrossRef] [PubMed] [Google Scholar]
- Enhancing shared and surrogate decision making for people living with dementia: A systematic review of the effectiveness of interventions. Health Expect. 2021;24:19-32.
- [CrossRef] [PubMed] [Google Scholar]
- 'It all depends!': A qualitative study of preferences for place of care and place of death in terminally ill patients and their family caregivers. Palliat Med. 2019;33:802-11.
- [CrossRef] [PubMed] [Google Scholar]
- Burying our mistakes: Dealing with prognostic uncertainty after severe brain injury. Bioethics. 2020;34:612-9.
- [CrossRef] [PubMed] [Google Scholar]
- A grounded theory study: Exploring health care professionals decision making when managing end stage heart failure care. J Adv Nurs. 2021;77:3142-55.
- [CrossRef] [PubMed] [Google Scholar]
- Non-readmission decisions in the intensive care unit: A qualitative study of physicians' experience in a multicentre French study. PLoS One. 2021;16:e0244919.
- [CrossRef] [PubMed] [Google Scholar]
- Medical and moral considerations regarding complex medical decisions in older patients with multimorbidity: A compact deliberation framework. BMC Geriatr. 2018;18:25.
- [CrossRef] [PubMed] [Google Scholar]
- To intubate or not to intubate: Emergency medicine physicians' perspective on intubating critically ill, terminal cancer patients. J Pain Symptom Manage. 2017;54:654-60.e1.
- [CrossRef] [PubMed] [Google Scholar]
- A Mixed method thematic review: health related decision making by the older person. J Clin Nurs. 2018;27:e1327-43.
- [CrossRef] [PubMed] [Google Scholar]
- A qualitative study exploring the difficulties influencing decision making at the end of life for people with dementia. Health Expect. 2018;21:118-27.
- [CrossRef] [PubMed] [Google Scholar]
- "Often Relatives are the Key […]"-Family involvement in treatment decision making in patients with advanced cancer near the end of life. Oncologist. 2021;26:e831-7.
- [CrossRef] [PubMed] [Google Scholar]
- Decision making for the initiation and termination of dialysis in patients with advanced cancer. Semin Dial. 2019;32:215-8.
- [CrossRef] [PubMed] [Google Scholar]
- Navigating complex end-of-life decisions in a family-centric society. Nurs Ethics. 2020;27:1003-11.
- [CrossRef] [PubMed] [Google Scholar]
- Is every life worth saving: Does religion and religious beliefs influence paramedic's end-of-life decision-making? A prospective questionnaire-based investigation. Indian J Palliat Care. 2018;24:9-15.
- [Google Scholar]
- Changes in limitations of life-sustaining treatments over time in a French intensive care unit: A prospective observational study. J Crit Care. 2018;47:21-9.
- [CrossRef] [PubMed] [Google Scholar]
- Physician workload associated with do-not-resuscitate decision-making in intensive care units: An observational study using Cox proportional hazards analysis. BMC Med Ethics. 2019;20:15.
- [CrossRef] [PubMed] [Google Scholar]
- What influences patients' decisions regarding palliative care in advance care planning discussions? Perspectives from a qualitative study conducted with advanced cancer patients, families and healthcare professionals. Palliat Med. 2019;33:1299-309.
- [CrossRef] [PubMed] [Google Scholar]
- Decision-making on withholding or withdrawing life support in the ICU: A worldwide perspective. Chest. 2017;152:321-9.
- [CrossRef] [PubMed] [Google Scholar]
- Decisions and dilemmas: The context of prioritization dilemmas and influences on staff members' prioritization decisions in residential aged care. Qual Health Res. 2021;31:1306-18.
- [CrossRef] [PubMed] [Google Scholar]
- Decision-making for older patients by Australian and New Zealand doctors with advance care directives: A vignette-based study. Intern Med J. 2019;49:1146-53.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of healthcare professionals' personality and religious beliefs on the decisions to forego life sustaining treatments: An observational, multicentre, cross-sectional study in Greek intensive care units. BMJ Open. 2017;7:e013916.
- [CrossRef] [PubMed] [Google Scholar]
- End-of-life planning depends on socio-economic and racial background: Evidence from the US health and retirement study (HRS) J Pain Symptom Manage. 2021;62:1198-206.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to and facilitators of South Asian Indian-Americans' engagement in advanced care planning behaviors. J Nurs Scholarsh. 2017;49:294-302.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of spirituality on decision-making in palliative care outpatients: A cross-sectional study. BMC Palliat Care. 2020;19:22.
- [CrossRef] [PubMed] [Google Scholar]
- The involvement of cancer patients in the four stages of decision-making preceding continuous sedation until death: A qualitative study. Palliat Med. 2018;32:1198-207.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers in the decision making about and performance of continuous sedation until death in nursing homes. Gerontologist. 2020;60:916-25.
- [CrossRef] [PubMed] [Google Scholar]
- Differences by race, religiosity, and mental health in preferences for life-prolonging treatment among medicare beneficiaries. J Gen Intern Med. 2019;34:1981-3.
- [CrossRef] [PubMed] [Google Scholar]
- Advance directive: Does the GP know and address what the patient wants? Advance directive in primary care. BMC Med Ethics. 2018;19:58.
- [CrossRef] [PubMed] [Google Scholar]
- In the patient's best interest: Appraising social network site information for surrogate decision making. J Med Ethics. 2018;44:851-6.
- [CrossRef] [PubMed] [Google Scholar]
- "Futile Care"-an emergency medicine approach: Ethical and legal considerations. Ann Emerg Med. 2017;70:707-13.
- [CrossRef] [PubMed] [Google Scholar]
- Meaningful shared decision-making: Complex process demanding cognitive and emotional skills. J Eval Clin Pract. 2020;26:431-8.
- [CrossRef] [PubMed] [Google Scholar]
- Frailty status, timely goals of care documentation and clinical outcomes in older hospitalised medical patients. Intern Med J. 2021;51:2078-86.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers and perceptions regarding code status discussion with families of critically ill patients in a tertiary care hospital of a developing country: A cross-sectional study. Palliat Med. 2017;31:147-57.
- [CrossRef] [PubMed] [Google Scholar]
- Grounds for surrogate decision-making in Japanese clinical practice: A qualitative survey. BMC Med Ethics. 2021;22:5.
- [CrossRef] [Google Scholar]
- Clinical decision making in the recognition of dying: A qualitative interview study. BMC Palliat Care. 2017;16:11.
- [CrossRef] [PubMed] [Google Scholar]
- The wave of very old people in the intensive care unit-a challenge in decision-making. J Crit Care. 2020;60:290-3.
- [CrossRef] [PubMed] [Google Scholar]
- What do hospitalists experience as barriers and helpful factors for having ACP conversations? A systematic qualitative evidence synthesis. Perspect Public Health. 2019;139:97-105.
- [CrossRef] [PubMed] [Google Scholar]
- Ceilings of treatment: A qualitative study in the emergency department. BMC Emerg Med. 2019;19:9.
- [CrossRef] [PubMed] [Google Scholar]
- Factors predisposing terminally ill cancer patients' preferences for distinct patterns/ states of life-sustaining treatments over their last six months. J Pain Symptom Manage. 2019;57:190-8.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Decision-making among the substitute decision makers in intensive care units: An investigation of decision control preferences and decisional conflicts. J Adv Nurs. 2020;76:2323-35.
- [CrossRef] [PubMed] [Google Scholar]
- Ética Clínica: Abordagem Prática Para Decisões Éticas na Medicina Clínica (7th ed). Porto Alegre: AMGH Editora; 2012.
- [Google Scholar]
- Four models of the physician-patient relationship. JAMA J Am Med Assoc. 1992;267:2221-6.
- [CrossRef] [Google Scholar]
- Systematic review of factors influencing decisions to limit treatment in the emergency department. Emerg Med J. 2022;39:147-56.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in palliative care quality between patients with cancer, patients with organ failure and frail patients: A study based on measurements with the Consumer quality index palliative care for bereaved relatives. Palliat Med. 2016;30:780-8.
- [CrossRef] [PubMed] [Google Scholar]
- Making Shared Decision-Making a Reality no Decision about me, without me. 2011. (1st ed). London: The King's Fund; Available from: https://www.kingsfund.org.uk/publications/making-shared-decision-making-reality#:~:text=mean%20in%20practice%3F,Making%20shared%20decision%2Dmaking%20a%20reality%3A%20No%20decision%20about%20me,make%20this%20vision%20a%20reality [Last accessed on 2023 May 21]
- [Google Scholar]
- Para o bem do Paciente: A Restauração da Beneficência nos Cuidados da Saúde (1st ed). São Paulo: Edições Loyola; 2018.
- [Google Scholar]
- Clinical bioethics in diversity: The essential contribution of the deliberative proposal of Diego Gracia. Bioethikos. 2012;6:49-57.
- [Google Scholar]
- Clinical decision-making: heuristics and cognitive biases for the ophthalmologist. Surv Ophthalmol. 2018;63:119-24.
- [CrossRef] [PubMed] [Google Scholar]
- Manual de Cuidados Paliativos (1st ed). São Paulo: Hospital Sírio Libanês, Ministério da Saúde; 2020.
- [Google Scholar]







