Translate this page into:
The Multidisciplinary Team in Palliative Care: A Case Reflection
Address for correspondence: Dr. Liza Bowen; E-mail: lizabowen@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
This essay is a reflection on the multidisciplinary team in palliative care, from the perspective of a final year MBBS student from the UK spending one month with an Indian pain and palliative care team at Institute Rotary Cancer Hospital (IRCH), AIIMS, New Delhi.
Keywords
Family
Multidisciplinary team
Total pain
INTRODUCTION
A multidisciplinary team (MDT) is a group of healthcare professionals of varied disciplines and roles, working together towards a common goal of providing optimal care for a patient. Most areas of healthcare now work in multidisciplinary teams, but palliative care lends itself particularly well to this approach because of the multiple dimensions involved in caring for palliative patients: physical, social and psychological, and with close links to the family.[1] The palliative care I saw in the UK was one of the best functioning multi-disciplinary approaches that I have seen, and I visited India because I was interested to get a cross-cultural perspective. In this essay I reflect on my time spent with the team at IRCH, with reference to one of the cases that I followed.
CASE REPORT
Mrs D was a 36-year-old female patient diagnosed with metastatic triple negative breast cancer (stage T4b N3 M1). The patient had undergone 7 cycles of chemotherapy before being referred to and managed by the pain and palliative care team. Metastases had spread to her cervico-dorsal, lumbar and sacral vertebrae and bilateral pelvic bones. On presentation to the pain control out patients department (OPD) she had severe pain in her head and neck, and was admitted to the inpatient palliative care unit for analgesic titration and control of nausea and vomiting.
Management
The patient was already on anti-sickness medication (Ondansetron); further management of nausea and vomiting included the introduction of a proton pump inhibitor (Pantoprazole) as well as advice on diet and patterns of eating.
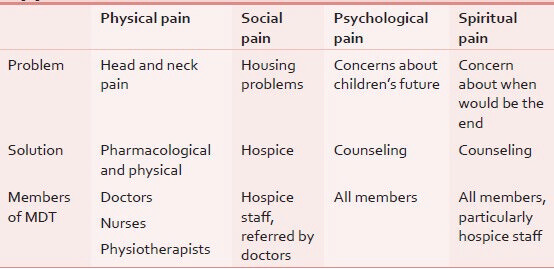
The management of the patient's pain was more complex, and can be framed in the context of total pain [Table 1].[2]
Physical pain control was managed as per the WHO pain ladder.[3] The patient was already on step 3 of the ladder, so her morphine dose was increased from 20 mg every 4 h to 30 mg every 4 h. Due to her head and neck pain, an MRI was done. This was discussed at a cross-disciplinary meeting with the radiologists to clarify what the progression of the disease was and what would be the most appropriate way to move forward with management. Although the progression of disease was such that treatment was no longer an option, a decision to give radiotherapy was taken as a palliative measure in order to prevent spinal cord compression and its complications, as well as to relieve pain and preserve function.[4] As an adjunct to this, the physiotherapists provided advice on movements of the head and neck, and also a neck brace.
The patient's social problems had started when she first fell ill. She had to leave her job of making clothes and therefore lost some of the family income. Her brother and husband were also missing work to bring her to the hospital and spend time with her there, resulting in a further loss of income. Housing problems arose when the family's landlord found out that the patient was in the terminal stages of illness and asked the family to vacate the property. The children went to stay with another family but the patient was left without a home to go to once she was discharged from the palliative care unit. In this situation a non-governmental charity organization was called upon, who run a hospice. The hospice provides care for patients who have nothing further to benefit from cancer treatment, providing symptomatic care for pain and other distressing cancer symptoms (nausea, restlessness, and respiratory problems).
Psychological pain was clearly evident upon speaking with the patient, and support was provided by all members of the palliative care team. I found there was an emphasis on communication and empathy above and beyond what is seen in other medical disciplines in the hospital. The patient's family (daughter, brother and husband) also spent lots of time with her in the hospital and were an ongoing source of psychological support.
I did not witness any interactions with health professionals in the hospital that were explicitly spiritual. However, the approach taken when discussing the patient's prognosis and coming to terms with things implicitly involved some level of spirituality, to a greater degree than is common in the UK. The hospice has more space for spiritual matters; spiritual counselors or leaders can come to the hospice to see the patients, with each religion given equal respect. The hospice state that the sisters themselves interact spiritually with the patient whenever needed and is possible, while maintaining that there is strictly no indoctrination.
Reflections on the role of MDT
The care of the above patient involved doctors from different specialties (anaesthetics, medical oncology, surgical oncology, radiology), as well as other health professionals (nurses, physiotherapists), health professionals working in other sectors (NGOs), and also the patient's family who play a key role in palliative care in India. I will discuss the roles and interactions of different members of the team in turn.
Doctors
Doctors from different specialties worked closely with each other, sharing discussions on ward rounds and between times, so that there was collaboration rather than disciplines working independently on what they believe to be their remit of a patient's care. There was also a smooth system in operation between the OPD management of pain, and the small (6 bed) ward that was reserved for the most urgent cases of pain control. When patients presented to the OPD, if they were suffering from pain that could not be remedied with a simple change in prescription, they were admitted to the ward for titration of analgesics or for an episode that required some other management in the hospital.
Other hospital healthcare workers
The different health professionals worked side by side. It was a hierarchical system, with doctors being in charge of patient care and nurses and physiotherapists involvement arising as instructed by the doctor, but the role of the physiotherapist and nurses was highly valued by the doctors. In outpatient clinics the different professionals were working in the same room so could work closely together.
NGO Sector
Involvement of the NGO sector was complementary to the care given at the hospital. Rather than being two separate entities, the government hospital and NGOs worked together. In the above case, the hospital suggested hospice care and the suitability of this was considered between the doctors, the hospice, the family and the patient. Hospices are far less common than in the UK, and the doctors of this hospice described themselves as acting in a way as a safety net, providing care for people who did not have the option of family care at home as per the norm for Indian society.
In other cases, I saw a further role for NGOs. There was another NGO that provided home support to patients being cared for by their families. Contact with the NGO was usually made by doctors from hospitals, and many patients were both receiving home visit care and visiting outpatient pain clinics. The home support team was able to spend more time with individual patients in their own environment, and also provide practical and emotional support to the families. For this they had a counselor in their team as well as a doctor and a nurse. Because of this emphasis there was a less hierarchical structure, with many patients requiring the counseling services over and above the medical ones, and doctors were not present on all visits. There was communication between the home team doctors and leads of the hospital pain unit, which ensured that both services were operating with the same principles and allowed discussion of difficult cases.
The home care team also collaborated with the hospice, keeping it as an option to suggest for patients or families who were not coping well at home. The role that the home care team NGO provided is somewhat analogous to the Macmillan nurses in the UK. Macmillan nurses are also funded partly by charity, although after a Macmillan nurse role has been operating for three years, the National Health Service takes over the funding. A systematic review of studies from western countries showed that home care can reduce symptom burden as well as making patients more likely to die at home (as many of them wish). The set up is very different in India to that of the western countries in the study, but it shows the potential value of such home care teams, particularly where even more focus is on families caring for dying patients in the home.[5]
The family
In palliative care worldwide the importance of the family is emphasized.[6] In India this importance is manifold, as most patients are cared for in the family home, and die at home. The family then take on a role not just as part of the patients' social and emotional life, but also as carers and therefore part of the healthcare team. The daughter of the patient discussed was doing most of the caring for the mother, cooking and cleaning in the house and helping her to get around as she needed. This requires a different kind of collaboration with families, involving education as to the patients' physical needs as well as emotional.
Linked with this central role of the family in India seemed to be a subtly different reality with respect to the four pillars of medical ethics (autonomy, beneficence, non-maleficence, justice).[7] In the UK there is a strong emphasis on autonomy, and patients' right to knowledge about their health and disease as well as decisions arising from this.[5] Indian law also emphasizes autonomy and consent, but in clinical practice there is sometimes a different reality, with patients not always aware of their diagnosis or prognosis.[8] The philosophy of the palliative care team I was working with was to be open with the patients about their disease status and prognosis and to encourage them to accept this, often addressing these issues with patients for the first time. Even within this strong culture of openness there were still some cases in OPDs where families wanted to shelter their relatives from this information and the family's wishes were upheld. The above patient had full knowledge of her condition and prognosis, and the doctors took time with the relatives when the patient was in the ward to discuss the prognosis and difficulties in uncertainties of not knowing exactly how long the patient had to live.
The role of communication
During my time at IRCH it was World Palliative Care day. Many patients and relatives of patients told their stories of being cared for under this palliative care team. The overall theme to come out of their accounts was the positive effect on both the patients and the families' experience of the end of life. An emphasis on the human aspects of the care received was made, so it is clearly not just the imposition of a structure of individuals from different disciplines working well together, but the nature of those individuals which may be a more difficult or more gradual thing to instill in a department.
CONCLUSION
My experience of the multidisciplinary team in an Indian palliative care was of a team with cohesive structure and relationships. Working between disciplines and between sectors provided a good support structure for patients. A limitation of this is that it is a single center that provides care to patients from a vast geographical area because of the absence of such services elsewhere. To extend the benefits of such teams requires greater education and advocacy of the palliative care approach in other institutions and care providers. The main contrast to the UK that I found was the more practical role of the family in providing care, and patients commonly staying at home throughout the duration of their illness.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- The assessment and treatment of physical pain associated with life-limiting illness. In: Hospice/Palliative Care Training for Physicians: UNIPAC Vol Vol. 3. (1st ed and 3rd ed). Glenview: American Academy of Hospice and Palliative Medicine; 2007.
- [Google Scholar]
- WHO (World Health Organisation), Cancer Pain relief. Geneva: World Health Organisation; 1996.
- Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev. 2013;6:CD007760.
- [Google Scholar]
- Working with families in palliative care: One size does not fit all. J Palliat Med. 2006;9:704-15.
- [Google Scholar]
- Principles of biomedical ethics. In: Principles of Biomedical Ethics (5th ed). United Kingdom: Oxford University Press; 2001.
- [Google Scholar]
- Communication with relatives and collusion in palliative care: A cross-cultural perspective. Indian J Palliat Care. 2009;15:2-9.
- [Google Scholar]






